Soft Tissue Pathology
Bursal, Tendon, and Muscle Diseases
Heidi Prather, Devyani Hunt and Adam Zierenberg
Key Points
• Extra-articular hip disorders coexist with intra-articular hip disorders.
• Biomechanics of the pelvic girdle and its relationship to the hip and spine are complex.
Introduction
Extra-articular hip pain originating from the pelvic girdle has many sources. Extra-articular disorders may be the primary source of hip pain in some cases; others are the result of adaptations or guarding mechanisms for intra-articular hip disorders. Recognizing and differentiating the two can be difficult. Nevertheless, we will attempt to describe extra-articular sources of hip pain by their region of distribution at clinical presentation. These regions include the anterior pelvis and groin, the lateral hip and thigh, and the posterior pelvis (Fig. 39-1).
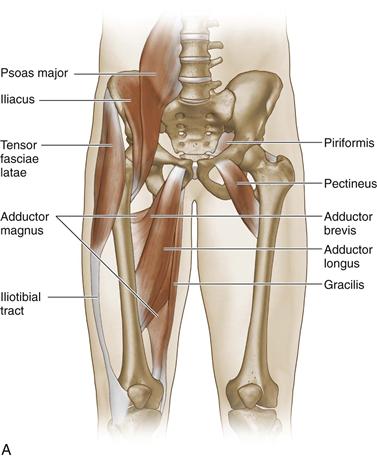
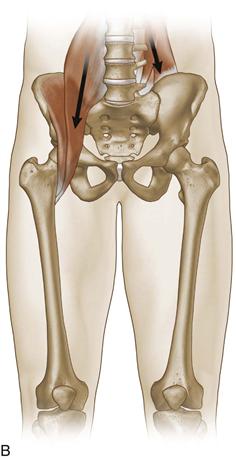

Figure 39-1 A, Muscles and tendons involved in pelvic, groin, and anterior pelvic pain. B, Orientation of activation of iliopsoas in relationship to the spine and the hip.
(Redrawn from DeRosa C: Functional anatomy of the lumbar spine and sacroiliac joint. Paper presented at 4th Interdisciplinary World Congress on Low Back and Pelvic Pain, Montreal, Canada, November 2001.)
C, Muscles, tendons, and ligaments associated with posterior pelvic girdle pain.
Epidemiology and Risk Factors
Hip pain occurs in any age group but is most prevalent between the ages of 40 and 60.1 The prevalence of extra-articular pain differentiated from intra-articular pain is unknown, and it is likely that the two types commonly coexist. The most common site of soft tissue pathology in the hip region is found laterally over the greater trochanter. Reports indicate that the prevalence of greater trochanteric pain in adults ranges between 20% and 35%.6–8 Posterior pelvic pain related to the sacroiliac joint (SIJ) ranges in prevalence between 13% and 62%.9–13 Many reported variations in SIJ prevalence are related to the method of confirming the diagnosis by history and physical examination alone or by image-guided intra-articular injection. Risk factors associated with extra-articular hip pain are many and variable. They include age, female gender, other lower extremity injuries or osteoarthritis, low back pain, previous lumbar spine surgery, and cumulative injury. Chou and colleagues reported that of patients who responded to intra-articular SIJ injection, 44% had a history of trauma and 21% had cumulative trauma. Although the specific mechanisms of cumulative trauma have not been studied, others have described these to include activities that require torsion, repetitive rotation, or single-leg stance.14,15 Acute trauma with loading or a blow to the pelvic girdle is an obvious risk factor for the development of extra-articular hip pain and can be difficult to diagnose in the setting of normal diagnostic imaging.
Pathophysiology
The pathophysiology of extra-articular hip pain is twofold. Some disorders occur as the result of acute overload or trauma. Others may be more insidious in onset and may be related to multiple factors, including guarding, biomechanical failure related to repetitive overuse or overload, biology, and adaptations to underlying articular disorders. The biomechanics about the pelvic girdle is complex, not only because of multidirectional loading and transmission of forces across the pelvic girdle, but also because of the load and transmission of forces through the spine and hip. Extra-articular soft tissue structures function to help reduce load at any one particular joint. Specifically, the pubic symphysis, the L5-S1 three-joint complex (disk and facet joints), the hip, and the sacroiliac joint must share and transfer load as efficiently as possible to decrease the presence of abnormal forces across any or all of these joints and associated soft tissue structures. Any bony disorder such as deformity, fracture, or cartilage injury can then overload the extra-articular structure, causing dysfunction and pain. The large body of work by researchers such as Vleeming, Snijders, and DonTigny has brought to light the complex biomechanics of the lumbar spine and pelvic girdle and the complexity of biomechanical dysfunction. Researchers have tied their findings to clinical implications.16–25
Figures 39-2 through 39-4 demonstrate the roles of muscles and ligaments when accepting an asymmetrical load across the pelvic girdle. A dysfunction in any one of the moving parts may result in secondary adaptations and potentially in painful syndromes. These are just a few examples that reinforce the importance of understanding the complex underlying reasons for extra-articular hip disorders.
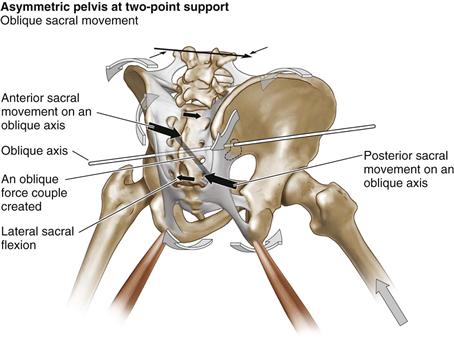
Figure 39-2 Oblique loading causing asymmetry in loading and movement. The longer the stride during the gait cycle, the greater is the asymmetry across the pelvic girdle causing an oblique force. An oblique force couple is created from the posterior interosseous ligament of the sacroiliac joint on the left to the sacrotuberous ligament on the right. The sacral rotation drives trunk rotation toward the side of loading (here it is the right side); this precedes the loading and serves to decrease the impact of loading. (Redrawn from DonTigny RL: Pelvic dynamics and the subluxation of the sacral axis. Havre, Montana, CD-ROM, 2009.)
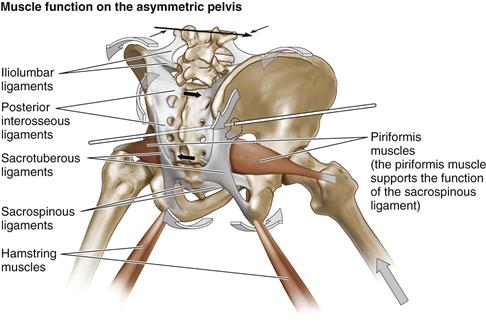
Figure 39-3 Function of the piriformis muscle The piriformis muscle functions to support and assist the sacrospinous ligament in restoring the sacrum to its resting position as the pelvis moves to a position of symmetry at midstep. (Redrawn from DonTigny RL: Pelvic dynamics and the subluxation of the sacral axis. Havre, Montana, CD-ROM, 2009.)
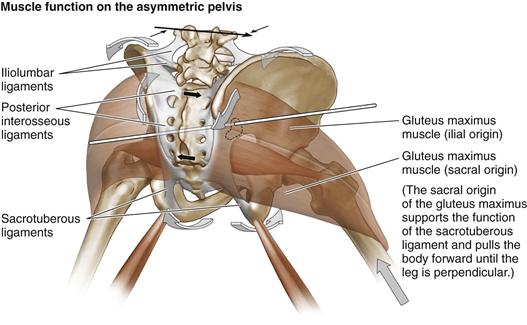
Figure 39-4 Function of the gluteus maximus muscle. The sacral origin of the gluteus maximus serves to assist and support the function of the sacrotuberous ligament in bringing the distal sacrum anteriorly and laterally as the sacrum moves from lateral flexion to its resting position when the pelvis moves to symmetry at midstep. The sacral origin of the gluteus maximus and the piriformis must act as prime movers on the sacroiliac joint when the pelvis is asymmetrically loaded. The sacral origin of the gluteus maximus also functions to pull the pelvis anteriorly over the loaded side until the leg is perpendicular at midstep. The ilial origin of the gluteus maximus then undergoes an eccentric contraction to decrease loading forces on the contralateral side. (Redrawn from DonTigny RL: Pelvic dynamics and the subluxation of the sacral axis. Havre, Montana, CD-ROM, 2009.)
Clinical Features and Diagnosis
A common dilemma for a hip specialist is determining whether a patient’s pain and dysfunction are caused by an intra-articular or extra-articular source. The distribution of pain is a helpful place to start when formulating a differential diagnosis. Intra-articular hip pain is thought to cause anterior groin or lateral hip pain and occasionally posterior pelvic pain.26–30 However, several soft tissue abnormalities may cause the same distribution of pain. The following is a brief description of the clinical features and diagnostic algorithms pertaining to soft tissue abnormalities of the hip (Fig. 39-5 through 39-7).
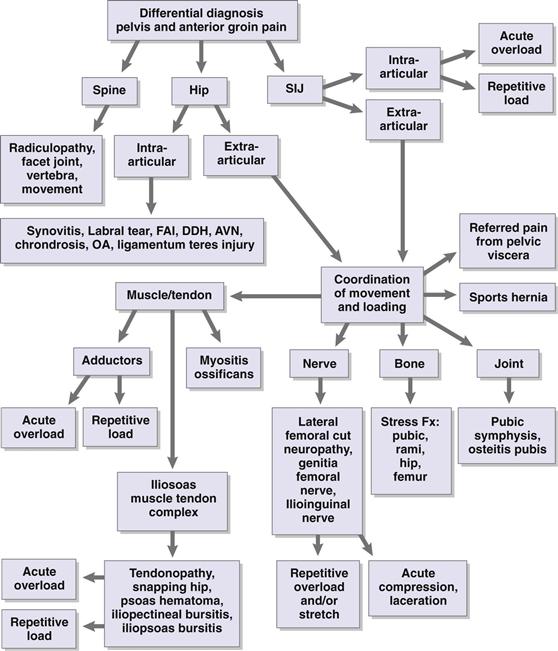
Figure 39-5 Differential diagnosis of pelvic and anterior groin pain.
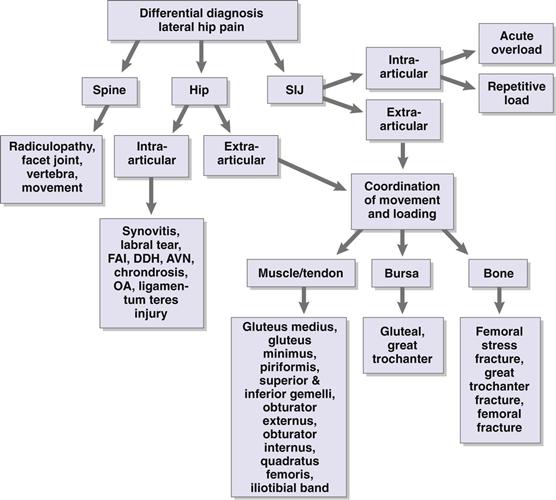
Figure 39-6 Differential diagnosis of lateral hip pain.
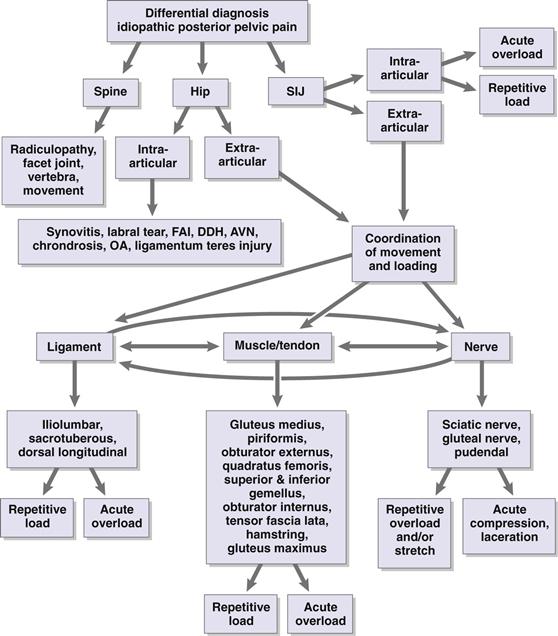
Figure 39-7 Differential diagnosis of idiopathic posterior pelvic pain.
Extra-articular Anterior Hip Pain
Iliopsoas Muscle–Tendon Complex Disorders
The iliopsoas muscle–tendon complex consists of three muscles: the psoas major, the psoas minor, and the iliacus (Fig. 39-1A). The proximal fibers of the psoas muscles originate on the bodies of the 12th thoracic vertebrae and the lumbar vertebrae; they then cross into the pelvis and join with the fibers of the iliacus to make the iliopsoas tendon. The fibers of the tendon hug the anterior aspect of the hip capsule, and the psoas portion rotates as it descends, so the ventral surface becomes the medial aspect. The conjoined tendons of the psoas and iliacus insert onto the lesser trochanter. The innervation of the psoas major is derived from the anterior nerves of the second and third lumbar roots. The psoas minor is innervated by the first lumbar nerve root, and the iliacus by the anterior branches of the second and third lumbar nerves through the anterior crural nerve. The iliopsoas not only functions as the prime mover of hip flexion, it also plays an essential role in the functional stability of the hip, the pelvis, and even the spine (Fig. 39-1B). Unilateral contraction of the iliopsoas muscle facilitates lateral flexion of the lumbar spine and external rotation of the hip. Dysfunction and injury to the complex can manifest as anterior hip pain and can cause compensatory biomechanical alterations in hip functioning and therefore secondary pain complaints. Owing to its close association with the spine, disorders of the iliopsoas are associated with low back pain.31 Cumulative changes to the tendon can occur as the result of increased muscle firing related to guarding for a primary spine or hip dysfunction, or firing of the muscle in an inefficient manner, such as in a lengthened position that may occur secondary to a hip, pelvic girdle, or hip dysfunction. Any of these situations can lead to the development of bursitis in the acute setting and, later, to tendinosis. Iliopsoas muscle–tendon complex disorders are commonly seen in conjunction with an intra-articular hip problem. The pattern of a shortened, painful tendon can develop as the result of compensation for reduced hip internal rotation and extension, leading to pain with hip extension. This pattern is seen in patients with hip osteoarthritis or other intra-articular disorders. Acute injuries to the iliopsoas tendon, such as tears and avulsion injuries, may occur.32,33 These injuries typically are associated with a traumatic event; however, repetitive overuse can predispose to this type of injury.
Patients with iliopsoas muscle tendon disorders present with anterior hip pain or groin pain that is worse with concentric or eccentric contraction of the hip flexor. Sports activities that require forceful hip flexion or adduction are painful, and even low-level activities such as walking or rising from a seated position can be painful.32 Runners describe anterior groin pain when trying to lengthen their stride, during speed training, or with uphill running.32,34
Key features on examination include a tender tendon with palpation and pain with activation of the hip flexor. Hip range of motion (ROM) can also be painful owing to stretching of the tendon and most notably occurs with abduction and extension of the hip.32 Special tests of the hip, including the flexion-abduction-external rotation (FABER) test, can be painful because of a relative stretch to the tendon that occurs in the position of testing. Caution should be taken in drawing conclusions from the examination because the presence of a painful tendon to palpation and pain with activation of the hip flexor does not rule out an intra-articular hip disorder. Secondary dysfunction of the hip flexor muscle–tendon complex commonly occurs as the result of an underlying intra-articular disorder. It is important to examine the hip in weight bearing during dynamic motion to further assess for abnormal motor patterns that contribute to repetitive overuse injuries. Matrix testing35 in three planes of motion (frontal, sagittal, and transverse) has been found to be a reliable measure; it is not specific to the hip joint but gives a general assessment of side-to-side symmetry of motion.30
Snapping Hip Syndrome.
Snapping hip syndrome is a complex of symptoms in which the key feature is an audible snap heard at or around the hip joint.36 Three types of snapping hip have been identified: intra-articular, internal, and external. The most common type, external snapping hip, occurs when the gluteus maximus tendon or the iliotibial band snaps over the greater trochanter. The intra-articular type refers to an abnormality of a structure inside the hip, which causes the “snapping” and typically is associated with pain. Causes include loose bodies, synovial osteochondromatosis, labral tears, cartilage flaps, osteochondral fractures, and transient hip subluxation.34,36
Internal snapping hip occurs when the iliopsoas tendon glides across the iliopectineal prominence, causing an audible snap.37,38 It is usually painful, and the pop or snap occurs in the anterior aspect of the hip as the hip goes from flexion to extension. Snapping can also occur across the femoral head39 or, less commonly, at the lesser trochanter.32,36 The pathophysiology has been studied and numerous causes have been found, including an association with a thickened tendon.34,40 More commonly, the tendon is structurally normal; however, it may not be at its optimal length. It is most likely a part of the continuum of chronic iliopsoas dysfunction. A shortened or lengthened tendon contributes to the development of iliopsoas tendinopathy and snapping. It is important to assess for other soft tissue abnormalities or joint problems at the hip or spine when evaluating the iliopsoas tendon because they commonly occur together.
The clinical presentation of medial snapping hip is similar to those of iliopsoas muscle tendon disorders; however, the hallmark feature is a painful audible snap in the anterior aspect of the hip.32,34 Painful hip ROM and pain with palpation of the iliopsoas muscle and tendon may not always occur. The painful snap can be reproduced by ranging the hip from the FABER position into extension, adduction, and internal rotation.41
Diagnostic Imaging.
Diagnostic imaging for snapping hip pain does not always reveal objective indications for the source of pain and dysfunction in patients without hip deformity or degenerative changes. Radiographs may be normal. Ultrasound evaluation can provide good information regarding the integrity of the iliopsoas tendon and can be used to dynamically assess for a snapping tendon across the iliopectineal prominence.42 MRI can be useful in evaluation of the muscle and tendon and to rule out an intra-articular abnormality.42 Structural changes to the tendon are not always seen, and the diagnosis becomes one of exclusion with the clinician relying on the history and physical examination findings.
Diagnostic injections of anesthetic are useful when the diagnosis remains in question after imaging. The tendon or the bursa can be injected with anesthetic under image guidance (fluoroscopy or ultrasound).42 A diagnostic intra-articular injection should also be considered if an intra-articular abnormality needs to be ruled out.
Specific Considerations for the Treatment of Iliopsoas Muscle–Tendon Complex Disorders.
Initial treatment of iliopsoas muscle–tendon complex disorders consists of conservative measures. A period of rest can be very helpful to reduce acute pain. The rest period should be relative to the activity causing the dysfunction and should be variable in length as determined by evidence of reduction of symptoms and recovery. In chronic conditions that are associated with an abnormal pattern of movement, a relative rest period is necessary to break the cycle of pain. With acute injuries, a rest period is essential to allow the tendon to heal. A course of oral or topical anti-inflammatory medications is recommended.
Evidence suggests that physical therapy should be part of the initial treatment protocol.39,43,44 Physical therapy should focus on the iliopsoas tendon with the goal of optimizing the length and strength of the muscle–tendon complex. The iliopsoas tendon typically is shortened or chronically “turned on” owing to a learned overuse pattern. It is important for physical therapy to address these abnormal movement patterns at the hip, pelvic girdle, and spine and to restore optimal functioning during everyday activities. Once this has been accomplished, advancing to higher-level activities, including sports-specific exercises, is essential for returning to full activity. Modalities such as ultrasound or iontophoresis can be used to decrease inflammation in the tendon or bursa.
If a 3-month period of conservative treatment fails, a lidocaine and corticosteroid steroid injection into the bursa should be considered for iliopsoas or iliopectineal bursitis. The literature also describes corticosteroid injection into the iliopsoas tendon sheath.45 However, caution should be taken because tendon ruptures after steroid injections have been documented.46,47 Injections should be performed under image guidance with fluoroscopy or ultrasound.42,45
Surgical Treatment for Painful Iliopsoas Muscle–Tendon Complex Disorders.
Surgical release or lengthening of the iliopsoas tendon has been used successfully for recalcitrant cases of internal snapping hip. The response to a diagnostic injection of the tendon with lidocaine can predict the response to surgical release.42
Open procedures and arthroscopic approaches have been described.39,48 No comparative data on open and endoscopic procedures are available. Arthroscopically, the tendon can be lengthened at the lesser trochanter, or the tendinous portion of the musculotendinous unit can be released using a transcapsular approach from the peripheral compartment. A study of 19 patients randomly assigned to either approach showed that both groups improved their Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) scores, and no difference in clinical improvement was noted between the groups.49
Postoperative management is patient specific with limitation of active hip flexion. Typically, no range-of-motion or weight-bearing restrictions are recommended. Patients have weak hip flexors postoperatively and require a program of graded strengthening. Return to full activity generally is allowed after 3 to 6 months. Complications resulting from the operation include motor and sensory changes, swelling of the bursa, hematoma formation, heterotopic ossification, hip flexor weakness, and infection.39,48,49
Adductor Strains.
The adductor muscle group consists of six muscles in the medial thigh and includes the adductor longus, adductor brevis, adductor magnus, gracilis, obturator externus, and pectineus. They originate at various points along the pubis and insert into the medial femur. The obturator nerve innervates this group of muscles, except for the pectineus, which is supplied by the femoral nerve. In the open chain, the primary function of this muscle group involves hip adduction. In the closed chain, along with lower abdominal muscles, the adductors stabilize the pelvis and the lower extremity during activity.50 Individual muscles have secondary roles such as femoral flexion and rotation.51,52 The adductor longus is the most commonly strained muscle owing to its poor mechanical advantage.53
Chronic muscle strains and associated pain have been attributed to myofascial trigger points (MTrPs). MTrPs are described as localized areas of tenderness and hyperirritability in a muscle tendon or ligament associated with a characteristic referral pattern.58 Simons and associates59 described the pain associated with MTrPs as stemming from hypersensitive taut bands of muscle, which may have sustained previous injury. Shah and colleagues60 further demonstrated a change in the biochemical milieu surrounding MTrPs. Bradykinins, cytokines, catecholamines, prostaglandins, and other markers are elevated and bind to nociceptors, causing localized pain and tenderness.
Patients with adductor strains typically present with groin pain and or medial thigh pain that is worse with activity. In most cases, this event is insidious in onset, and occasionally it is associated with an inciting event. In these cases, acute rupture or osseous avulsion should be considered.62 On examination, tenderness to palpation is noted, along with associated pain with passive stretch or activation of the adductors. Swelling of the muscle group and weakness of hip adduction have been described.41,63
As with other soft tissue disorders of the hip, radiographic evaluation is of low yield but can be helpful in discerning between this and other bony abnormalities of the hip such as osteitis pubis or pelvic stress fracture. Musculoskeletal ultrasound evaluation can enhance visualization of the tendon, enthesis, muscles, ligaments, and nerves64 (Table 39-1). MRI should be used to confirm the diagnosis or to differentiate other potential soft tissue disorders of the hip.65 Treatment initially consists of relative rest, liberal ice, and oral anti-inflammatory medication. Special rehabilitation considerations for adductor disorders include the importance of balancing muscle length and strength not just of the adductors but of other pelvic girdle muscles that contribute to counterforces across the pelvis. Any associated problems such as intra-articular hip disorders or spine disorders should be evaluated and treated. In recalcitrant cases, serial injections of lidocaine at the site of insertion or in the muscle belly can be helpful to interrupt the pain cycle and reduce symptoms. Surgical management should be considered in cases of acute rupture. Open repair with suture anchors has been described with good results for osseous avulsions.62
Table 39-1
Ultrasound for Diagnosis of Extra-Articular Hip Disorders
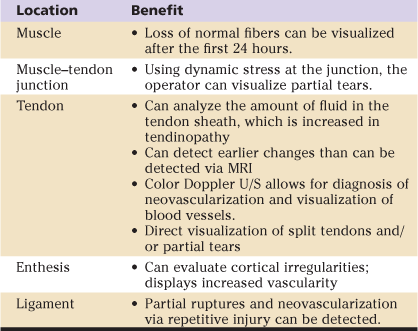
MRI, Magnetic resonance imaging; U/S, ultrasound.
Reproduced from Borg-Stein JZJ, Hanford M: New concepts in the assessment and treatment of regional musculoskeletal pain and sports injury. 1:744–754, 2009.117
Sports Hernia.
Another soft tissue cause of anterior groin pain is a sports hernia, which is also termed athletic pubalgia or rectus abdominis injury.66 The exact cause is highly debated. Meyers and coworkers67 described the cause as a hyperextension injury to the rectus abdominis insertion onto the pubic symphysis. Others describe it as an occult hernia of the posterior inguinal wall without signs of a visualized tear.66,68 This is similar to Gilmore’s groin, which is a tear in the external oblique aponeurosis and conjoint tendon.66 Participants in activities and sports that require repetitive twisting and turning of the upper leg and torso, such as ice hockey, soccer, and rugby, are at risk for sports hernias.66–68 Repetitive trunk hyperextension and thigh hyperabduction cause shearing at the pubic symphysis.66 Another risk factor is muscle imbalance between strong proximal thigh muscles and relatively weaker abdominal muscles.66
Patients typically describe insidious onset of groin pain with activity, worsened by coughing or sneezing or by sudden movement such as sprinting or kicking. Patients can but do not always have tenderness to palpation of the superficial inguinal ring, posterior inguinal canal, pubic tubercle, or conjoined tendon. No hernia is palpable. Patients may have pain with resisted sit-ups, active hip adduction, or Valsalva. MRI is the recommended imaging study because of its good sensitivity and specificity.69
Surgical exploration and repair can be considered after failure of at least 6 to 8 weeks of conservative management consisting of relative rest, icing, nonsteroidal anti-inflammatory drugs (NSAIDs), and physical therapy, to address the muscle imbalances and improve core strengthening.66,68 Both open and laparoscopic approaches are used with or without mesh.66–69 Results of repair and return to play are generally good, and full activity is expected for most patients.66–69
Osteitis Pubis.
The cause of osteitis pubis is debated, but most agree that it represents degenerative changes that occur at the pubic symphysis. The cause is not well understood but has been linked to trauma, pregnancy, rheumatologic disorders, and postinfectious sequelae. In idiopathic cases, musculoskeletal imbalances at the pelvis have been theorized to contribute. In a study of athletes,70 a correlation was found between decreased hip ROM and the development of osteitis pubis. Sports activities that require repetitive and forceful twisting and kicking are associated with pubic symphysis disorders, as are chronic overuse injuries to the adductors and rectus abdominis muscles.71,72
Patients report aching anterior pelvic pain that can radiate into the groin, medial or anterior thigh, or abdomen. The pain can be sharp with activity and worse with weight-bearing activities or sports activities that require twisting or pivoting. Motions that require activation of the lower abdominals or adductors can be painful. The pain can be debilitating and can have a significant effect on ambulation and therefore on activities of daily living.
Examination reveals pain over the pubic symphysis and/or pubic rami. Hip ROM, specifically, internal rotation, can be painful. Passive adduction is painful as is activation of the adductors.71–73 Radiographic evaluation in acute cases of pubic symphysitis is usually normal. In the chronic setting, changes consistent with osteitis pubis may be seen.71–73 These include a widened or narrowed symphysis, sclerosis, and cystic changes to the bone. Views of the pelvis during single-leg stance can be helpful in evaluating for instability or motion at the pubic symphysis.41 Further imaging with nuclear bone scan can show increased uptake, but the clinician should consider that evidence of changes on the bone scan can lag weeks to months behind the development of symptoms.41,71-73 MRI can show evidence of bone edema and is helpful in ruling out parasymphyseal stress fractures and other causes of anterior pelvic pain.71
Treatment options begin with a course of conservative measures. Specific considerations when treating osteitis pubis include addressing movement disorders of the pelvic girdle. A pelvic stabilizing belt such as a sacroiliac joint belt can be used to decrease shear stresses across the pubic symphysis. Image-guided injections with fluoroscopy or ultrasound can be helpful. Injection of anesthetic should be considered in cases in which radiographs do not show significant degenerative changes to the pubic symphysis, and the diagnosis of pubic symphysitis is in question. Corticosteroid injections, which should be considered for recalcitrant cases of osteitis pubis, yield varying results.72,73 Surgical options have been described with mixed results.72,73
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








