Chapter 78 Soft Tissue Healing
History
As long as there have been medical writings, attention has been directed to wound healing and attempts to enhance and accelerate it. The use of plant extracts, even bread mold, in healing is at least 2000 years old by written record.9,52 Both the Edwin Smith Surgical Papyrus from 3000 to 2500 BC and the Ebers Papyrus described certain of the earliest known wound manipulations—splinting and honey—to influence outcome.6,19 Among the contributions of Hippocrates, who lived around 400 BC, was his insistence on cleanliness and irrigation of wounds with boiled water. In addition, his prescient emphasis on documentation and accurate recording of events is a primary characteristic of good medical practice to this day. Hippocrates’ scholarship was followed 300 years later by the Roman Celcus and about 100 years after that by Galen, whose work on wounded gladiators of Asia Minor led to his understanding of the venous and arterial systems, wound care dressings, and meticulous follow-up. Descartes wrote the first Western physiology text, and Ambroise Paré deserves credit for one of the most significant contributions to our current approach today, the emphasis on gentle handling of tissues and on the harmful effects of trauma on tissue.26,42 This concept, crucial today in the handling of all surgical wounds, such as avoidance of crushing clamps and prolonged vigorous retraction, is all the more remarkable because it was introduced into a medical world in which wounds were being treated with boiling oil and “laudable pus” was the ideal. Paré insisted that careful tissue handling was the first step to uncomplicated tissue healing, a point we will emphasize.
The late 19th and early 20th centuries saw rapid progress in our understanding of the causes of healing difficulties. Joseph Lister’s practical acceptance of Pasteur’s germ theory of infection, controversial at the time, bore fruit in his description of aseptic technique and the use of carbolic acid as a topical disinfectant in hospitals in which infection was rampant.9 His practical application of this sound principle, coupled with the discovery of antibiotics, sulfanilamide in the late 1930s and penicillin soon after, which resulted in Alexander Fleming’s shared Nobel Prize in 1945, put in place the last essential component of normal wound healing, control of infection, as the second half of the 20th century began.17
Phases of Wound Healing
Wound healing may be separated chronologically into three phases. Although these phases overlap, the events that predominate in each phase are different and together produce the strong, substantial, protective, resilient end point that we called the healed wound.7
Fibroblastic Proliferative Phase
The cellular elements and chemotactants that rapidly accumulate in the wound during the first phase of healing prepare the wound for the migration of fibroblasts, which are the primary synthesizers of collagen, the substance responsible for the healed wound’s strength and durability. This second phase of healing begins at approximately 48 hours after the wound occurs. Fibroblasts climb along the fibrin matrix that has been deposited during the inflammatory phase of platelet aggregation and hemostasis. This crucially important matrix can be interfered with and can be a cause of wound-healing delay.80 As fibroblasts migrate in and provide the predominant cell type present in the healing wound at approximately day 5, they produce ground substance, a gel-like combination of hyaluronic acid and chondroitin 4-sulfate, the glycosaminoglycans. This substrate will act as a matrix for the collagen fibrils synthesized most rapidly during the first few days of wound healing. This first collagen synthesized, tropocollagen, is converted to collagen fibrils, which assume structural and biochemical integrity and on which wound strength is based; it is in the first 3 or so weeks after healing that we see the most rapid rise in wound strength gains.56 Collagen homeostasis is reached at approximately 3 weeks as collagen synthesis and degradation rates approach one another. This stage leads to the last and most prolonged phase of wound healing, the phase of remodeling, or the phase of collagen maturation.
Wound Maturation Phase
In this last phase, the cellular elements producing collagen within the wound are markedly diminished; the collagen fibrils deposited become dramatically more organized and structured in response to a variety of factors, including local mechanical demands. The water content of the wound, along with measurable ground substance, diminishes and is manifested as local induration. The amount of type III collagen, initially present in large amounts, is reduced and replaced by type I collagen as the tissue strength–providing elements much more closely approach the elements that give strength to normal skin. Stronger collagen cross links create mechanical resistance to disruption in the now-maturing wound. This process continues for many months, even years, after the initiating event.68,69
Cellular Elements of Healing
T lymphocytes produce a sustained response to injury in the wound. They generate local influences on the vascular endothelial lining in preparation for regrowth of new vessels. In addition, they produce fibroblast-activating factor, which encourages and regulates fibroblastic activity in the healing wound. T-cell depletion at the time that a wound occurs can significantly deter breaking strength in the healing wound.4,70
Macrophages migrate into the healing wound and are activated as they participate in the initial inflammatory phase. These cells remain in the wound much longer than other responders, such as polymorphonuclear leukocytes, and release cytokines responsible for angiogenesis and for stimulating fibroblast proliferation.55 Some studies have noted significant loss of the essential early functions of fibroplasia and debris clearance if the accumulation or availability of macrophages or their active migration into a wound is interfered with.98
Factors Affecting Soft Tissue Healing
Scarring and Tissue Perfusion
Adequate levels of PO2 in the healing wound are essential. The oxygen delivery system, whereby inspired oxygen traverses the pulmonary vessels, binds to hemoglobin, and is subsequently released in response to tissue demands, can be subject to breakdown at several points.50 Local scarring, irradiated tissue, diabetes, and chronic exposure to cigarette smoke can all interfere with the ability of small vessels to provide sufficient oxygen to the healing wound. Even local swelling or increased tissue pressure, such as that created by a hematoma, can so reduce perfusion that ischemia results.90 Preparation for surgery requires attention to all these factors. At the molecular level, collagen synthesis by fibroblasts will not occur if tissue oxygenation is not adequate.
The mechanism whereby the destructive effect of tissue ischemia occurs, whether the result of poor perfusion, radiation injury, or even small-vessel disease such as seen in diabetes mellitus, is believed to be the production of oxygen free radicals. These free radicals may be a factor in aging skin and its loss of elasticity. Free radicals are in fact cytotoxic to cells, both to cell membranes and to their internal components.58,101 In addition, free radicals can disrupt protein components such as enzymes and cause collagen to degrade prematurely.93 Minimizing free radical production by ensuring adequate tissue oxygenation is one way of minimizing or even reversing these detrimental effects.
When local factors dramatically reduce wound perfusion and create severe local ischemia, the only solution is a dramatic increase in local tissue oxygenation or the local blood supply. One treatment option here is the use of hyperbaric oxygenation therapy. This modality increases the partial pressure of oxygen in plasma by subjecting the patient and wound to an atmosphere of 100% oxygen at twice the normal atmospheric pressure at sea level.103 This creates an elevated PO2 level in the arterioles, thereby forcing increased amounts of oxygen into compromised tissue (Fig. 78-1). For this treatment to be effective, there must be no local infection nor any local perfusion problems. Most notably, hyperbaric oxygenation therapy is not effective in the presence of frank tissue necrosis. Also, the requirement for specialized equipment is an additional economic factor in this choice of treatment. Tissue that is severely ischemic in the postoperative period is treated by local or distant flap transfer, which allows removal of tissue with circulatory compromise and the introduction of healthy, well-vascularized tissue to deliver oxygen so that healing may progress.60
Smoking
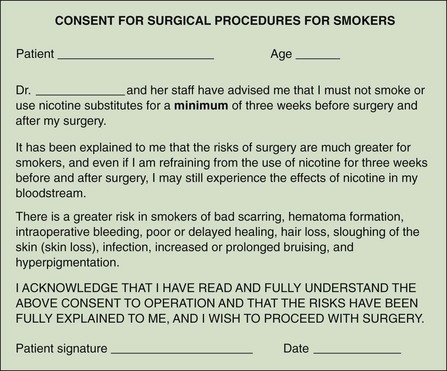
Although cigarette smoking has an unhealthy effect on almost every organ system of the body, the detrimental effects on wound healing can, unfortunately, be manifest in the postoperative period as progressing wound ischemia and marginal necrosis. Absorbed nicotine and its breakdown product, cotinine, have an inhibiting effect on capillary circulation and cause necrosis of skin margins to an unpredictable degree. Moreover, in a cigarette smoker, the addition of even a small degree of overzealous traction may cause wound compromise because the effect is additive to the peripheral circulatory effect of inhaled cigarette smoke. In addition, the carbon monoxide contained in cigarette smoke forms carboxyhemoglobin, a form of hemoglobin that shifts the oxygen dissociation curve to the left, which makes oxygen release to ischemic tissue more difficult.25,32,51,82 This twofold effect of cigarette smoking on tissue oxygenation puts a patient who smokes at risk for wound-healing difficulties. Although there is no hard evidence regarding a well-defined preoperative period of discontinuation of smoking that would ensure uncompromised healing, we insist on at least 3 weeks’ abstention from smoking or from exposure to second-hand smoke and require such abstention until skin sutures are removed in the postoperative period.57 In our practice, smokers are required to sign an additional consent form (Fig. 78-2).
Diabetes Mellitus
The fact that a diabetic patient is prone to a variety of secondary vascular, neurologic, and wound-healing difficulties is well known to surgeons. However, the concept of small-vessel occlusive disease as the primary reason for these secondary illnesses, as well as for the wound-healing difficulties sometimes experienced by diabetic patients, has not been borne out in multiple studies of ischemia in the diabetic wound; other factors seem to play a larger role.54
Diabetic patients have increased blood viscosity secondary to a stiffer, less deformable red blood cell, thus making it more difficult for the red cells to pass through the tiny capillaries supplying oxygen to local tissue.91 The high serum glucose level in a poorly controlled diabetic patient shifts the hemoglobin dissociation curve and inhibits oxygen delivery to the capillaries, thereby causing lower tissue PO2 and resulting in impaired healing.16
Finally, the tibial and peroneal arteries in a diabetic patient seem to be particularly prone to atherosclerotic peripheral vascular disease.65 Preventive measures regarding these vulnerable patients include preoperative vascular examination of the lower extremities, with palpation of the peripheral pulses, and further evaluation if abnormalities are noted, meticulous control of the serum glucose level in the perioperative period, and avoidance of extremity edema and the local compounding of a diabetic’s rheologic changes that edema increases.
Other Factors
Anemia
The evidence regarding anemia as a contributing factor in the failure of wounds to heal is inconclusive. Hemoglobinopathies and extreme drops in the hematocrit level, both of which can compromise delivery of oxygen, have not been proved to compromise soft tissue healing.3,35,43,85
Radiation Exposure
Ionizing radiation causes injury, not just to the target tissue but also to the tissue that surrounds the target. Radiation was at one time used to aid in wound healing and treat scar formation, for keloid control in particular; there are patients today who have had such exposure (Fig. 78-3). The damage caused by ionizing radiation is permanent, progressive, and irreversible. Radiation causes an obliterative endarteritis that results in local tissue ischemia and permanent difficulty with wound healing, normal wound contracture, and the formation of healthy granulation tissue. There is some evidence that these healing difficulties in irradiated tissue are caused by collateral damage to local fibroblasts and their proliferation, on which tissue healing is dependent.30,31,86
Steroids
The effect of steroids on wound healing can be minimized by the administration of vitamin A, topically or orally. Collagen deposition, increase in wound strength, and functional macrophage support are documented effects of oral vitamin A in a steroid-dependent patient.21,37,38
Aspirin and Nonsteroidal Medications
Many prospective total knee replacement patients take nonsteroidal anti-inflammatory drugs (NSAIDs) for pain relief, and a large number of adults take one or more aspirin tablets daily as a cardioprotective regimen. There is some evidence that collagen synthesis is inhibited by normal therapeutic dosages of these medications, even in the normal population, and discontinuation of these medications in the perioperative and postoperative periods is recommended, in part because of this effect.47
Chemotherapy
Medications used to fight cancer inhibit wound healing. Although there is variation in the category and mechanism of action of this group of drugs, they are all designed to target rapidly dividing cells in some fashion. None are selective enough to protect healing tissue while continuing antineoplastic activity elsewhere. It is recommended, when possible, that the perioperative period provide a break in the administration of chemotherapeutic agents.102 The harmful effects seem to be most evident in the early phases of wound healing; a 2-week postoperative delay in administration can mitigate these harmful effects.23,24
Age
It is unclear whether advancing age alone inhibits wound healing. There is ample anecdotal evidence that whereas very young patients heal with scars that remain hyperemic and indurated for prolonged periods, older patients seem much less prone to this type of healing, a fact that is to their advantage when incisions are placed in cosmetically obvious areas such as the face.2,18,27,49,100 There is certainly no evidence that the final results of wound healing in terms of ultimate closure and tensile strength are inhibited or influenced by age. It may simply be that aging produces a slowing in the processes that lead to wound healing and that a more protracted course of collagen synthesis and cross linking is normal in an older patient.
Nutrition
Nutritional factors play a role in wound healing; a serum protein level below 2 g/dL is indicative of severe nutritional deficiency and can result in a prolonged inflammatory phase and impaired fibroplasia.73,77,97 Nutritional factors seem to be most important in the early phases of wound healing, when the local inflammatory response and early fibroplasia are most active. Only when profound malnutrition is present are the phases of wound healing impaired. Although it is most unlikely to encounter this problem in today’s surgical environment, many older patients are at least mildly deficient in one or more vitamins essential to healing; obtaining a nutritional consultation plus supplementing these patients with certain essential elements is an excellent idea.
Vitamin C
An essential element of wound healing, vitamin C, is required for the maintenance of tissue integrity in a normal healthy patient.72 Even a completely healed wound will lose strength over time if vitamin C intake is not adequate. Ascorbic acid is an absolute requirement for the normal synthesis of collagen, so stable structural elements, including the vessel wall, skin integrity, and the type III collagen of healing tissue, are affected when vitamin C intake is deficient. A truly vitamin C–deficient wound can be separated with only the smallest amount of manual pressure and hemorrhage from weakened capillaries is common. Rarely seen today, vitamin C deficiency is easily remedied when recognized.10
Zinc
Zinc is a trace element present in all human tissue and is required in almost every enzymic reaction. Administration of exogenous zinc increases the rate of wound healing only when there is a zinc deficiency; the surgeon may encounter deficiencies of this trace element in patients with chronic alcoholism, cirrhosis, and gastrointestinal absorption problems, such as short bowel syndrome. Zinc is required in such minute amounts for normal healing that only a dramatic loss of absorptive surface will produce a deficiency; in such cases, zinc administration can rapidly and markedly accelerate healing when provided as a supplement.53,76
Delay in the early phases of wound healing has been demonstrated in animal studies of zinc deficiency. Compromise in the cellular and humeral immune systems occurs as well.78,79
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree