Recurrent oral ulceration
Minor aphthous, major aphthous, or herpetiform ulceration observed by physician or patient recurring at least three times in one 12-month period
Plus two of:
Recurrent genital ulceration
Aphthous ulceration or scarring, observed by physician or patient
Eye lesions
Anterior uveitis, posterior uveitis, cells in the vitreous on slit-lamp examination, or retinal vasculitis observed by ophthalmologist
Skin lesions
Erythema nodosum observed by the physician or patient, pseudofolliculitis, papulopustular lesions, or acneiform nodules observed by physician in post adolescent patients not on corticosteroids treatment
Pathergy test
Read by physician at 24–48 h
Mucocutaneous features are the most common presenting symptoms of the disease. In the absence of ophthalmologic, neurological, or vascular involvement, the disease generally runs a benign course with a rather good prognosis [4]. Other less frequent cutaneous features of BD, which are not discussed in this chapter, are extragenital ulcers, Sweet’s syndrome, pyoderma gangrenosum, and palpable purpura.
Oral Ulcer/Oral Aphthae
Definition
The most common (97–100 %) and characteristic lesion of Behçet’s disease, and often the initial sign, is oral aphthosis. The term aphthae means ulcer and is used to describe areas of ulceration on mucous membranes. An aphthous ulcer is a painful mouth ulcer, resulting from a break in the mucous membrane. The severity may be such that the patient is unable to eat, swallow, and even speak during the acute period.
The most common sites of the lesions are the mucous membranes of the lips, the buccal mucosa, the floor of the mouth, the soft palate, and the tongue. Although rare, hard palate, gums, tonsillar fauces, and pharynx can also be involved. The lesions mostly start as an erythematous, circular, slightly raised area evolving into an oval or round ulcer within 48 h.
There are three well-differentiated clinical forms: minor aphthae, major aphthae, and herpetiform aphthae. Minor aphthae have a diameter <10 mm, are superficial, covered by a gray membranous slough, surrounded by an erythematous rim, and heal without scarring in 1–2 weeks. Major ulcers are morphologically similar but larger (>10 mm), deeper, more painful, and heal in 10–30 days or more often with scarring and tissue loss. In herpetiform ulceration, numerous (up to 100), small pinpoint (1–2 mm), yellowish, papular lesions become confluent and form larger plaques and can heal with scarring. Minor aphthae are seen in most patients, with major aphthae in approximately half, and herpetiform ulcers rarely. More than one type of aphthous ulcer may be present in an individual patient simultaneously (Fig. 42.1).
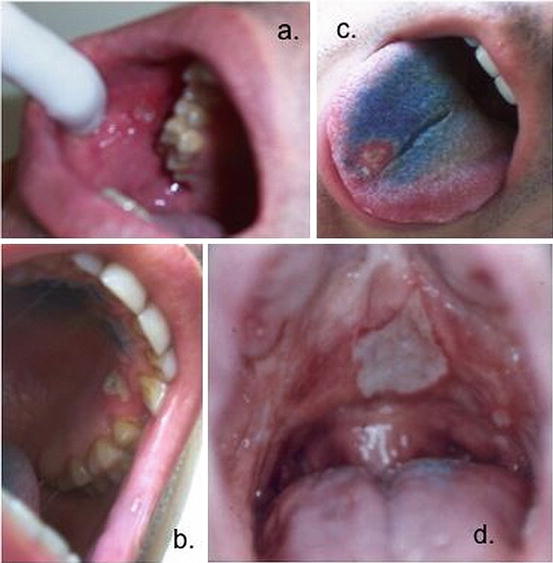
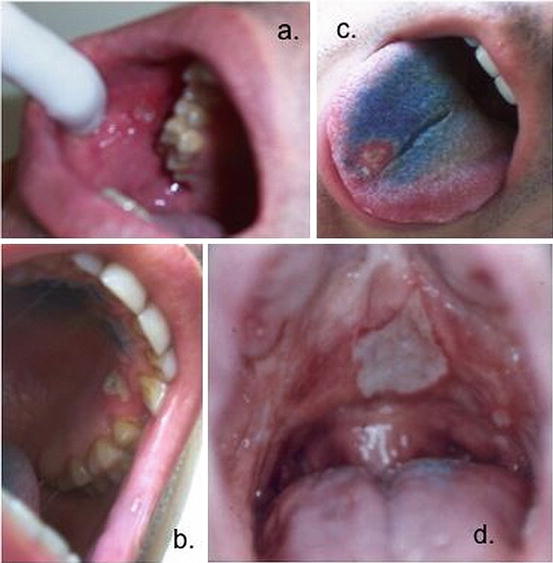
Fig. 42.1
Oral ulcers: (a) a minor ulcer on the buccal mucosa; (b) a minor ulcer on the gingiva; (c) a minor ulcer on the tongue; (d) a single major ulcer and minor ones on the hard palate
Differential Diagnosis
There are no specific tests available for BD, and the diagnosis is largely based on history and clinical features. Therefore, in a patient with recurrent oral aphthae, it is essential to reveal the existence of other clinical features of BD (genital ulcer, uveitis, acne, etc.) to establish a diagnosis [5].
Oral aphthosis is a very common complaint and can be related to various conditions developing within the oral cavity other than BD. One of the most striking feature of oral aphthosis associated with BD is its recurrent nature which may help to eliminate some sporadic causes of aphthosis in the differential diagnosis.
Recurrent multiple ulcers, especially in the absence of concomitant genital ulcers, are most typical (but not limited) of the following conditions: recurrent aphthous stomatitis (RAS), systemic lupus erythematosus (SLE), inflammatory bowel disease, celiac disease, HIV infection, and iron, B12, and folate deficiency. PFAPA syndrome (periodic fever, aphthous stomatitis, pharyngitis, and cervical adenitis) should also be included in the differential diagnosis, especially in pediatric patients with recurrent oral ulcers. Among the entities listed above, RAS is the most common affecting up to 25 % of the general population. Since RAS describes aphthous ulcers in the absence of systemic disease, its diagnosis is one of exclusion.
The pattern of aphthous ulceration is not a reliable guide to underlying causes, and it can be difficult to differentiate oral aphthae of BD from RAS on the basis of severity, duration, and frequency. Nevertheless, some reports suggested that patients with BD tend to have more ulcers (>6 simultaneously) and more frequent involvement of the soft palate and oropharynx than in RAS.
It should also be kept in mind that diagnostic clinical features may not be present at the onset of disease, and therefore, BD should be considered in patients diagnosed previously with RAS on development of potentially related clinical problems.
Biopsy
Histopathologic and immunofluorescent findings may exclude certain entities in the differential diagnosis and may lend support to the diagnosis of BD, but histopathologic findings are not diagnostic. The biopsies of oral lesions from BD show a mononuclear cell infiltrate in all sections. Although the ulcer itself is contained and surrounded by polymorphonuclear cells and contained cell debris, outside this zone and extending diffusely throughout the lamina propria, large numbers of infiltrating lymphocytes and macrophage-like cells can be seen. It is also important to note that histologically, there is no difference between the lesions in BD and those with RAS.
See Also
Aphthae.
Genital Ulcer/Genital Aphthae
Definition
Genital ulcers are the second most common manifestation of BD, present in 60–80 % of patients, and rarely are the first manifestation of the disease. They can be painful, leading to problems both sitting down and walking, pain on intercourse, as well as dysuria. Ulcers may be preceded by papules or pustules, and morphologically their appearance is similar to oral aphthae with round and sharp erythematous border (punched-out), covered with grayish-white pseudomembrane or central yellowish fibrinous base; they tend to occur less often than oral ulcers. They usually occur on the scrotum in the male while they are uncommon on the shaft or on the glans penis (Fig. 42.2). In the female, both major and minor labia are affected most commonly, but vaginal and cervical ulcers occur and may be associated with vaginal discharge. They usually heal in 2–4 weeks. Since they are usually deeper than oral aphthae, scarring may eventuate from intensely inflamed, deep lesions. It is therefore important to search for scars even if there are no signs of active ulcer at the time of examination. The ulcers located at the labia minor, however, may heal without scar formation. Furthermore, vaginal and cervical ulcers may be asymptomatic making speculum examination of the female patient essential.
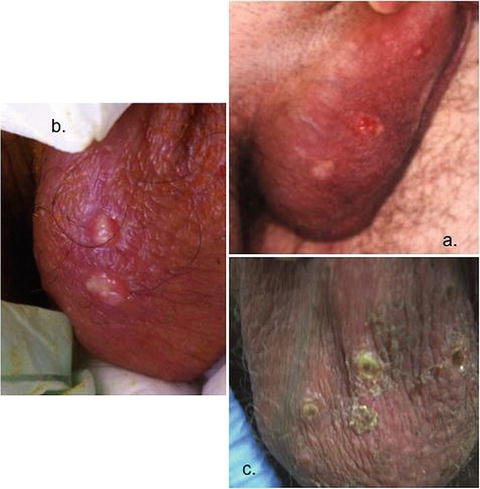
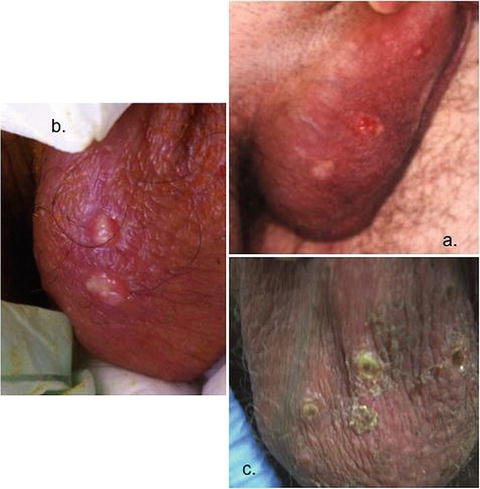
Fig. 42.2
Genital ulcers. (a) Three scrotal genital ulcer on different stages: upper while as a papule, middle while as a punch out ulcer, bottom while as a healed cicatrix; (b) two scrotal ulcer covered by a pseudomembrane; (c) several scrotal ulcer covered by a crust during healing
Differential Diagnosis
Clinically identical genital ulcers may be seen in a variety of disorders, either alone or together with oral ulcers. Differential diagnosis of patients presenting with recurrent genital ulceration accompanied by oral aphthae (orogenital ulceration) should include Reiter’s syndrome, mouth and genital ulcers with inflamed cartilage (MAGIC), inflammatory bowel disease, cyclical neutropenia, and Sweet’s syndrome. Recurrent orogenital ulceration may also be associated with bullous skin disorders, fixed drug reaction, and erythema multiforme.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








