Fig. 28.1
Gottron’s papule of the knee

Fig. 28.2
Gottron’s papules of the hands
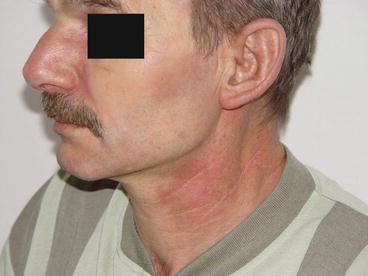
Fig. 28.3
Heliotrope rash and periorbital edema in a young patient with DM

Fig. 28.4
V sign in DM (Courtesy of Katalin Dankó)
The term amyopathic DM (ADM) (synonymous with “DM sine myositis”) and furthermore a closely related form of DM, “hypomyopathic DM,” (HDM) are characterized by the appearance of typical skin disease for at least 6 months without having any muscle weakness [5].
Cancer-associated DM is a subset that is probably much more prevalent in adults than it has previously been suspected, and the majority of patients develop skin symptoms characteristic of DM. Almost all children with DM also develop cutaneous manifestations usually before the diagnosis of myositis [1–4].
Differential Diagnosis
Skin symptoms should be differentiated from those seen in cutaneous manifestations of lupus. Exposure to UV light is a provoking factor in both cases. Pruritus is often an early event in DM that is typically missing in cutaneous lupus. The overall clinical presentation, and autoantibody findings (anti-double-stranded DNA in lupus), usually easily differentiates between these two connective tissue disorders. Skin involvement together with inflammatory disease is typical and characteristic for DM.
Skin biopsy may also help, but by itself does not clearly differentiate between DM and cutaneous manifestation of lupus; however, the lupus band test is negative in most of the cases [6]. Vascular deposits of C5b-9 are described in DM, but not in lupus.
Some other conditions with muscle symptoms should also be differentiated from DM. Infectious myopathies (HIV-1, coxsackie, adenovirus, echovirus, Epstein-Barr virus, hepatitis B virus) and drug-induced myopathies caused by a series of agents (antimalarial, lipid-lowering drugs/statins, and fibrates, colchicines, cyclosporine) as well as alcohol, cocaine, and heroin abuse should be considered in differential diagnosis. Furthermore, endocrine disorders (hypo- and hyperthyroidism, Cushing’s disease) with myopathy also should be considered. There are a large number of myopathies (inclusion body myositis, muscular dystrophies, metabolic myopathies) that should also be carefully considered in differential diagnosis. All of these particular disorders can be differentiated from DM by the specific findings of muscle biopsy and the lack of the classic skin symptoms described above. Detection of myositis-specific autoantibodies is also useful. Patients with anti-Mi2 usually have DM.
The aim of the DM management after a careful confirmation of the diagnosis is to assess all disease manifestations and define the disease activity and the extent of irreversible damage. Then an individualized treatment plan can be developed. The first-line therapy for myositis is corticosteroids. If the response is not sufficient, corticosteroids are supplemented with immunosuppressive agents. Methotrexate and azathioprine are the most commonly used drugs [7]. Physical therapy to restore muscle strength is also important. In refractory cases, other agents including mycophenolate, cyclosporine, tacrolimus, cyclophosphamide, and intravenous gamma globulin may also be efficient.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








