2 Skeletal Assessment of Fractures of the Proximal Femur
Although most proximal femur fractures are easily detected on routine x-ray studies, nondisplaced fractures of the hip are a reality and a challenge for imagers and surgeons alike. Radio-occult fractures of the hip are fractures that escape detection on routine x-ray imaging. A high index of suspicion is needed for patients in excessive pain or those refusing to bear weight. When the clinical situation does not correspond to a “negative hip x-ray,” these patients warrant further investigation. Imaging choices include computed tomography (CT), magnetic resonance imaging (MRI), and bone scan. Bone tomograms are of historical interest but are no longer performed. Rapid diagnosis and early treatment of occult fractures are in the patient’s best interest because this approach reduces the chance that a nondisplaced fracture will displace, a situation that requires more invasive management and increases morbidity.1
Radiologic Evaluation
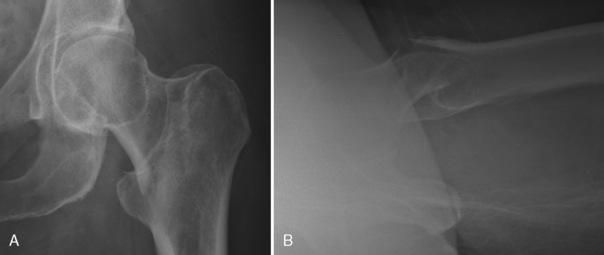
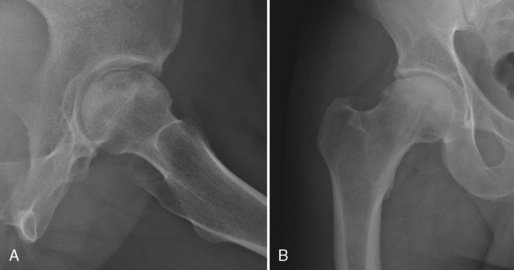
The routine radiographs used to evaluate hip fractures include anteroposterior (AP) and lateral views of the hip (Fig. 2-1). Frog leg views are not recommended in an acute hip fracture for fear of dislocation or displacement of fragments. An AP view of the pelvis is also recommended because so many elderly patients with hip pain and inability to bear weight have pubic rami fractures, which may be more visible on the pelvic x-ray film. In suspected cases of avascular necrosis (AVN) of the hip, a frog leg view can be helpful to evaluate for subchondral fracture of the femoral head (Fig. 2-2).
Computed Tomography
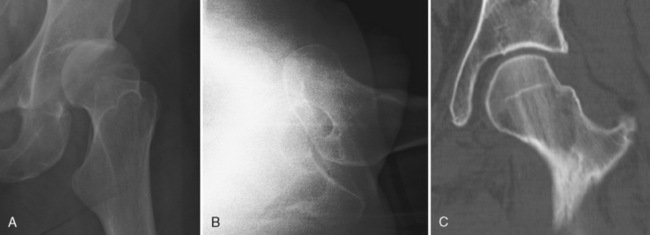
CT is a modality that is often readily available in the hospital setting, especially after hours. The CT imaging protocol has changed significantly in the last few years. Thin-cut slices that are 0.6 mm thick have become routine, whereas in the past much thicker slices, such as 3-mm cuts, were used. The older, thick slices had very choppy reformations, which made fracture detection more difficult. Today’s thin slices allow one to obtain beautifully detailed coronal and sagittal reformatted images (Fig. 2-3). Reformatted images, especially in the coronal plane, are recommended and often show a proximal femur hairline fracture more clearly (Fig. 2-4). In theory, the use of only axial imaging may fail to reveal fractures that are parallel to the axial imaging plane.2
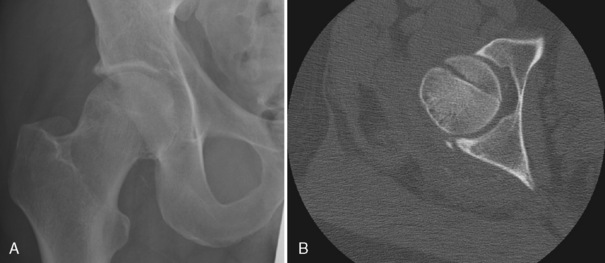
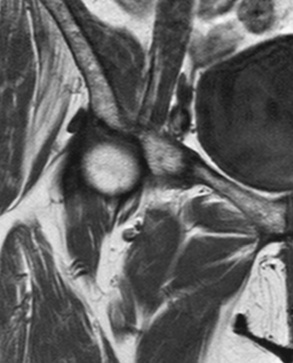
CT can be vital to operative planning in the established proximal femur fracture. This imaging technique allows excellent assessment of intra-articular bone fragments, such as in a patient with a history of hip dislocation3 (Figs. 2-5 and 2-6). It also shows such fine bony detail that articular collapse can be assessed in cases of AVN.
One study showed MRI to be a more accurate modality than CT scan for early diagnosis of occult hip fractures4 (Fig. 2-7). The image slice thickness in that study was 3.2 mm, much thicker than what would be used today.
Magnetic Resonance Imaging
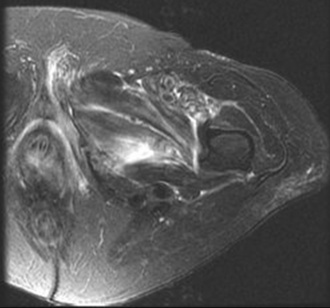
MRI is excellent at detecting occult fractures. A study of 15 osteopenic patients with normal plain radiographs and suspected hip fractures were imaged with MRI. Ten of the 15 patients showed a clear fracture on MRI, and these patients then underwent surgery based on the MRI study. The other 5 patients had no fracture noted on MRI and were successfully treated nonoperatively.5 MRI can also delineate disorders adjacent to fractures, such as infarcts or metastases, and nonsurgical entities such as pubic rami fractures (Fig. 2-8), bursitis, and muscle strain (Fig. 2-9).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree