Simultaneous Total Knee Arthroplasty and Femoral Osteotomy
John M. Siliski
INDICATIONS/CONTRAINDICATIONS
Simultaneous femoral osteotomy and total knee arthroplasty (TKA) should be considered for the treatment of deformities of the femur that would compromise or complicate a TKA done for osteoor posttraumatic arthritis. The deformities within the femur are most commonly the result of fracture malunion but may also be the result of metabolic conditions such as Paget’s disease or rickets. Most patients have had prior surgical treatment of the femur and therefore may have significant prior surgical scars and retained hardware. The most common situation is a mid-to-distal femoral nonunion with a previous lateral subvastus approach and retained lateral plate (1, 2, 3).
The types of femoral deformities encountered include frontal plane angular (varus or valgus deformity), sagittal plane angular (flexion or extension deformity), and torsional (internal or external rotation deformity). Any combination of these deformities may be encountered.
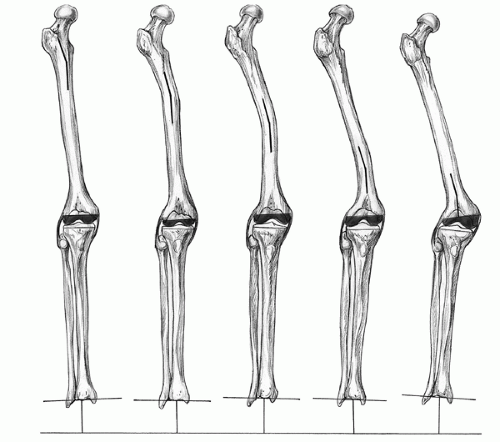
Frontal plane angular deformities are the most common type that lead to an indication for simultaneous osteotomy and knee arthroplasty, because even 10 degrees of deformity in this plane, if left uncorrected, may have significant effects on bone cuts and collateral ligament balance. The location of the deformity along the femur can influence its impact on the distal femoral cut. Hip adduction or abduction can compensate for more proximal deformities so that when the distal femoral cut is made, there is little effect on collateral ligament balance. In the presence of a distal deformity, however, a femoral cut made perpendicular to the mechanical axis can have a much greater impact (Fig. 13-1). Although minor degrees of frontal plane angular deformity can be managed by asymmetric distal femoral bone cuts and ligament balancing, as the varus or valgus femoral deformity becomes greater, so does the asymmetry of the bone cuts and the collateral ligament imbalance (4). By the point at which the frontal plane deformity is 10 degrees or more, a TKA will present a difficult problem of collateral ligament balance in flexion but marked imbalance in extension. The choice may then be either to try to improve ligament balance in extension, which may then lead to imbalance in flexion, or to use a more constrained implant that substitutes for collateral ligament function. The option essentially uses an implant for a primary arthroplasty that is most commonly used to salvage difficult revision knee arthroplasties (5, 6, 7).
If left uncorrected, sagittal plane deformities create several potential problems. If the surgeon places the femoral implant in a normal position on the distal femur, the persisting femoral deformity will result in the joint line not being parallel to the ground, and the leg will have altered mechanics caused by the effective hyperextension or flexion from the periarticular deformity. If the femoral component is placed on the distal femur in a flexed or extended position in an attempt to correct the periarticular deformity, difficulties occur with either femoral notching or overresection of the posterior condyles. It also becomes difficult to maintain proper function of the posterior cruciate ligament and balancing of the flexion and extension gaps. Consequently, sagittal plane deformities above 10 to 20 degrees should be considered for simultaneous osteotomy at the time of knee arthroplasty.
Rotational deformities, if left uncorrected, will leave the knee and foot pointed out or in; this may be tolerable for smaller degrees of malrotation for less active patients. Unfortunately, rotational deformities are minimally correctable during knee arthroplasty because the rotational positioning of the femoral and tibial components must be guided by bony anatomy, patellofemoral tracking, tibiofemoral
tracking, and balancing of the medial and lateral flexion gaps. For the active patient with a femoral rotational deformity greater than 20 degrees, a derotational osteotomy should be considered.
tracking, and balancing of the medial and lateral flexion gaps. For the active patient with a femoral rotational deformity greater than 20 degrees, a derotational osteotomy should be considered.
Contraindications to simultaneous femoral osteotomy and TKA include the following. Patients with knee pain but predicted future low demand for function, such as a nursing home patient who will permanently use a walker anyway, may best be treated without a corrective osteotomy. The knee arthroplasty may be performed with or without an attempt to correct the overall limb alignment. Patients who may have difficulty with the simultaneous rehabilitation of a healing osteotomy and a knee replacement should be considered for the alternative options. If there is any concern about residual infection in the femur, simultaneous osteotomy and knee arthroplasty should be avoided.
PREOPERATIVE PLANNING
Evaluation and Preparation
A standard orthopedic history should be obtained regarding the patient’s past history of injury, treatment, and current symptoms. In most cases, there will be a remote history of a femoral fracture and the more recent development of significant knee pain as arthritic changes have developed. The evaluation must include all aspects of the old injury, any residual effects on the extremity, and the severity of the knee arthritis. The history, examination, and imaging studies must then be processed by the surgeon to decide on a detailed surgical plan that takes into account all aspects of the case: surgical approach, use of tourniquet for the entire procedure or for arthroplasty only, removal of retained hardware, level of the femoral ostetomy, fixation device for the osteotomy, type of knee implant, and type of femoral guide system to be used.
The patient must also be prepared for a combined procedure that requires a longer anesthesia time and greater blood loss. Preoperative autologous blood donations should be considered.
Examination and Imaging Studies
Physical examination should include all the standard aspects for a knee being prepared for arthroplasty, including a detailed knee examination as well as an examination of the hip, foot, and ankle and neurocirculatory function of the limb. In addition, there will be aspects of the examination that should focus on leg length discrepancy, femoral deformity, and pre-existing scars. Any pre-existing scars will need to be considered as part of the overall plan for the exposure for the simultaneous osteotomy and arthroplasty.
Imaging studies should include standard anteroposterior (AP) (standing), lateral, and skyline views to assess the arthritic changes in the knee and their contributions to frontal and sagittal plane deformities in the limb as a whole. A lateral view taken with the knee in maximal extension will help to define the presence or absence of a flexion contracture in the knee. A 3-foot AP view of the extremity will permit assessment of the limb’s overall mechanical axis. AP and lateral views of the femur, based on the proximal segment, will permit assessment of the degree of frontal and sagittal plane angular deformities. An x-ray of the femur taken at the angle that maximizes the femoral angular deformity will permit measurement of the true maximal angular deformity, and in which plane it lies relative to the frontal and sagittal planes.
Instruments and Implants
Instruments for removing existing hardware and for placing the new internal fixation device (either a plate or intramedullary rod) will need to be available for the osteotomy. The surgeon may wish to have a C-arm image intensifier available to check the osteotomy, hardware placement, and mechanical axis. For the TKA, the surgeon needs to have available an extramedullary guide system if the internal fixation device will block use of an intramedullary guide. With the mechanical axis corrected with the osteotomy, a standard posterior cruciate ligament-retaining or substituting knee prosthesis should be all that is necessary for the arthroplasty unless there are additional complicating issues at the level of the knee.
SURGERY
Positioning
The patient is placed supine with a trochanteric roll. A radiolucent table may be chosen if use of image intensification is anticipated. If the limb is long and if the surgical incision will start at or below
the midthigh, a tourniquet may be placed before preparation and draping. If a tourniquet will interfere with the exposure for the osteotomy, it may be better to perform the osteotomy without a tourniquet and then place a sterile tourniquet after the osteotomy part of the surgery is completed.
the midthigh, a tourniquet may be placed before preparation and draping. If a tourniquet will interfere with the exposure for the osteotomy, it may be better to perform the osteotomy without a tourniquet and then place a sterile tourniquet after the osteotomy part of the surgery is completed.