Chapter 31 Sexual Dysfunction and Disability
Sexual Response and Behavior
Human Sexual Response
The classic model of human sexual response was formulated by Masters and Johnson146 in the 1960s based on a study of 600 able-bodied men and women. The model depicts women and men as having similar sexual responses throughout four phases: excitement, plateau, orgasm, and resolution (Table 31-1).148 In the Masters and Johnson model, men tend to pass through each phase faster than women and achieve only one orgasm per cycle, often with a very short plateau phase. Women can achieve multiple orgasms in the same sexual response cycle. Masters and Johnson146 also noted that women could also become “stalled” at the plateau phase and then pass straight to resolution without achieving orgasm.
Table 31-1 Masters and Johnson Model of Sexual Response
Modified from Masters WH, Johnson VE: Human sexual response, Boston, 1980, Bantam Books.
There have been many critics of the Masters and Johnson sexual response model, primarily because it places too much emphasis on genital responses and does not acknowledge the role of central neurophysiologic control.19,136,188,236 In the late 1970s, Kaplan devised a new model of sexual response with three phases: desire, excitement, and orgasm.119 In the Kaplan model, desire always precedes arousal, and is described as “the specific sensations that motivate the individual to initiate or become responsive to sexual stimulation.”119,125,188 The Kaplan model, like that of Masters and Johnson, proposes that human sexual response is linear and basically invariant between men and women.125
More recent research has furthered our understanding of human sexual response, particularly in regard to the ways in which the sexual response cycle is different in women and men. The Masters and Johnson, and Kaplan models ignore major components of women’s sexual satisfaction, such as the importance of trust, intimacy, affection, respect, and communication.19 Basson19–22 proposed a new model for the female sexual response to address these gender differences in 2000 to 2001 (Figure 31-1).125

FIGURE 31-1 Female sexual response cycle.
(Redrawn from Kingsberg SA, Janata JW. Female sexual disorders: assessment, diagnosis, and treatment, Urol Clin North Am 34:497-506, 2007.)
Basson’s circular model emphasizes that sexual response in women is much more complex than in men. In women a sexual encounter does not necessarily start from a place of spontaneous sexual drive or desire. Women often approach becoming intimate from a point of sexual neutrality, and the decision to become sexually engaged can result from numerous and varied factors, including a wish to emotionally connect with their partner.19,125 Sexual arousal and sexual satisfaction often do not occur solely through physical means such as clitoral stimulation and orgasm, but can also be dependent on intangible factors such as the ability to focus the mind on the present moment and a feeling of security or psychologic well-being.25 The circular sexual response cycle might be repeated many times within the same sexual encounter.25 Janssen et al.112 have also proposed a circular model of human sexual response that is similar to that of Basson, but that might be more applicable to both genders.
Sexual Behavior and Aging
The frequency of sexual activity has been well documented to decline with age.116 Recent research has shown that the degree of decline is much less than was previously thought and that sexuality remains an important contributor to quality of life throughout the entire lifespan.44,116 An important reason for the discrepancy is that older studies tended to quantify sexual activity only as intercourse, but more modern research looks at all aspects of sexuality.116 One study of men and women aged 80 to 102 years found that 63% of men and 30% of women continued to engage in sexual intercourse, whereas 83% of men and 64% of women participated in touching and caressing activities without intercourse, and 72% of men and 40% of women engaged in masturbation.44
Many medical factors influence sexual activity in the elderly, including sexual dysfunction caused by medical illness, increasing frailty, and the side effects of medications. Postmenopausal women tend to experience vulvovaginal atrophy and vaginal dryness, which causes pain with vaginal penetration.118 Men have decreased testosterone with advancing age, which contributes to diminished sexual drive and also has physical effects that contribute to increased frailty.117 Psychosocial barriers to sexual activity in the elderly are numerous, including decreased partner availability, alterations in body image and change in self-perception, cognitive decline, and environmental issues such as the loss of privacy experienced in many residential settings.79,117
Types of Sexual Dysfunction
Classification Systems
Sexual dysfunction is most frequently classified according to the Diagnostic and Statistical Manual, Fourth Edition, Text Revision (DSM-IV-TR).10 To qualify as a sexual dysfunction, a person’s sexual problem must cause “marked distress or interpersonal difficulty.” This distinction is important to remember for patients with disabilities, because they might experience altered sexual response but not have a sexual dysfunction in need of further workup or treatment.219 In the same way that spasticity after stroke or phantom sensations after amputation are not always problems that need to be addressed by the physician, a patient’s sexual difficulties only need to be treated when the patient’s quality of life is adversely affected.
The DSM-IV-TR allows for three subtypes to be applied to all primary diagnoses to further clarify the nature of the sexual dysfunction. The first subtype describes the onset of the disorder—lifelong or acquired (which means it developed after a period of normal functioning). The second subtype is used to designate the context in which the dysfunction occurs—generalized or situational (meaning limited to certain types of stimulation, situations, or partners). The third subtype delineates the etiologic factors associated with the sexual dysfunction—the practitioner must decide whether the problem is due to psychologic factors alone, or due to a combination of psychologic factors and the pathologic effects of a general medical condition. If the sexual disorder is fully explained by a general medical condition or substance abuse, without psychogenic factors, then it is coded separately. The DSM-IV-TR sexual dysfunctions are summarized in Table 31-2.10 There has been recent scholarly debate about the clinical usefulness of the DSM-IV-TR system of classification.13,27,28 It is based on the Masters and Johnson, and Kaplan linear models of human sexual response, and therefore often criticized as not being representative of the true nature of human sexual response, particularly for female sexual dysfunction.19 Another problem with the DSM-IV-TR criteria is that sexual disorders, particularly erectile dysfunction and dyspareunia, are typically diagnosed independent of etiology. Sexual disorders are difficult to fully classify according to criteria which mandate that the etiology is known before diagnosis.27 In addition, research has shown that there is often a high degree of overlap or comorbidity among the sexual disorders, particularly in women, and the DSM-IV-TR classification system does not allow for these findings.27,135,190,206
Table 31-2 Sexual Dysfunctions in the DSM-IV-TR
| Sexual Desire Disorders | |
| 302.71 | Hypoactive Sexual Desire Disorder |
| 302.79 | Sexual Aversion Disorder |
| Sexual Arousal Disorders | |
| 302.72 | Female Sexual Arousal Disorder |
| 302.72 | Male Erectile Disorder |
| Orgasmic Disorders | |
| 302.73 | Female Orgasmic Disorder |
| 302.74 | Male Orgasmic Disorder |
| 302.75 | Premature Ejaculation |
| Sexual Pain Disorders | |
| 302.76 | Dyspareunia (not due to a general medical condition) |
| 306.51 | Vaginismus (not due to a general medical condition |
| Sexual Dysfunction Due to a General Medical Condition | |
| 625.8 | Female Hypoactive Sexual Desire Disorder due to a general medical condition |
| 608.89 | Male Hypoactive Sexual Desire Disorder due to a general medical condition |
| 607.84 | Male Erectile Disorder due to a general medical condition |
| 625.0 | Female Dyspareunia due to a general medical condition |
| 608.89 | Male Dyspareunia due to a general medical condition |
| 625.8 | Other Female Sexual Dysfunction due to a general medical condition |
| 608.89 | Other Male Sexual Dysfunction due to a general medical condition |
| ___.__ | Substance-Induced Sexual Dysfunction (coding is substance-specific) |
| 302.70 | Sexual Dysfunction Not Otherwise Specified |
From American Psychiatric Association: Diagnostic and statistical manual of mental disorders, fourth edition, text revision (DSM-IV-TR), Washington, DC 2000, American Psychiatric Association.
A number of international consensus conferences have been held to address these concerns.26,27,140,141 Their guidelines follow the same general format as the DSV-IV-TR (primarily to retain consistency for research purposes), but they introduced updated definitions of the disorders. The DSM-V is set to be published in 2012, but until that time the reports of these consensus conferences contain the current best set of definitions of sexual dysfunction, and are summarized and expanded on below.11
Male Sexual Dysfunction
The main focus of both clinical care and research for men with sexual dysfunction has traditionally been centered on performance problems, particularly erectile dysfunction and premature ejaculation. There has been a major paradigm shift in the past two decades away from the psychiatric understanding of most sexual disorders in men and toward a medicalization of male sexuality (particularly with the advent of proerection medications).150,156,192 Purely psychogenic male sexual disorders are much more underrepresented in the medical literature and are often misdiagnosed as erectile dysfunction by health practitioners.157 Types of male sexual dysfunction include the following:
Female Sexual Dysfunction
Female sexual dysfunction is very common, with a reported prevalence of 40% to 50% in multiple population-based studies.13,135 Sexual dysfunction in women has become a focus of renewed research interest in the past decade, in part based on the new understanding of the female sexual response cycle proposed by Basson,19 and the implications of that understanding toward diagnosis and treatment.150 In contrast to sexual dysfunction in men, the psychologic aspect of women’s sexual functioning typically receives far more attention than organic etiologies of dysfunction. This discrepancy is partially because of institutional bias, but it is also based on a growing body of data suggesting that psychologic factors correlate more strongly with sexual dysfunction in women than do medical problems.26,135 It is especially important to remember that personal distress is necessary to make a diagnosis of sexual dysfunction when dealing with female patients. Up to 50% of women who report a problem with sexual functioning do not have any associated personal distress, and so they cannot be classified as having a sexual dysfunction.207 Types of female sexual dysfunction include the following:
Sexual Dysfunction in Disability and Chronic Disease
Spinal Cord Injury
In contrast to many of the other disabilities discussed in this chapter, sexual dysfunction in patients with spinal cord injury (SCI) has been well studied in both genders (see Chapter 55). The type of sexual dysfunction the patient will ultimately experience depends in large part on the spinal cord level and the degree of completeness of the injury.162 Multiple studies have shown that the frequency of sexual activity and the level of sexual satisfaction decrease in both men and women after sustaining an SCI.5,53,221
Bors and Comarr41 conducted a pivotal study in 1960 detailing the prevalence of erectile and orgasmic dysfunction in 529 men with SCI. They found that in men with complete UMN lesions, 93% of patients were able to achieve reflexogenic erections, and none were able to attain psychogenic erections. Anterograde ejaculation in complete UMN SCI was seen in 4% of patients. Men with incomplete UMN SCI achieved erections 99% of the time, with 80% of men having only reflexogenic erections and 19% having combined reflex and psychogenic erections. Ejaculation was possible in 32% of patients with incomplete UMN SCI, with 72% of those occurring after reflexogenic erection and 26% occurring after psychogenic erection. Complete LMN lesions showed a very different picture, with 26% of patients able to achieve psychogenic erections and none attaining reflexogenic ones. Ejaculation was possible in 18% of these men. Incomplete LMN lesions fared far better, with 90% of men retaining the ability to achieve erection and 70% the ability to ejaculate. The results of the Bors and Comarr study are summarized in Figures 31-2 and 31-3.
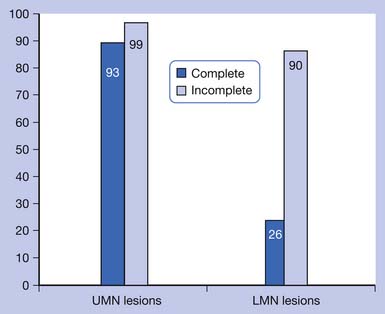
FIGURE 31-2 Percentage of men with spinal cord injury able to achieve erection.
(Data from Bors E, Comarr AE: Neurological disturbances of sexual function with special reference to 529 patients with spinal cord injury, Urol Surv 110:191-221, 1960.)
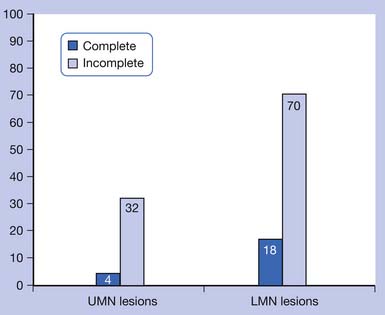
FIGURE 31-3 Percentage of men with spinal cord injury able to achieve anterograde ejaculation.
(Data from Bors E, Comarr AE: Neurological disturbances of sexual function with special reference to 529 patients with spinal cord injury, Urol Surv 110:191-221, 1960.)
Orgasmic ability has been shown to be preserved in 38% to 50% of men with complete UMN SCI, 78% to 84% of men with incomplete UMN injury, and 0% of men with complete LMN injury.5,6,178,218 It should be noted, however, that most studies of men have focused on the ability to ejaculate instead of the ability to have an orgasm, which have more recently been noted to be separate occurrences.6 Some men are also occasionally able to achieve orgasm without anterograde ejaculation, possibly indicating either anejaculation or retrograde ejaculation into the bladder.218
Women with SCI have more recently been shown to have sexual responses that are similar to those of men, with arousal and vaginal lubrication as the female correlate to penile erection.222,223 In women with complete UMN injuries, reflexogenic but not psychogenic lubrication is preserved.223 Sensation to light touch and pinprick in the T11–L2 dermatomes was found to be predictive of the ability for psychogenic vaginal lubrication (which is thought to be sympathetically mediated).222 From 44% to 54% of women with SCI have been shown to be able to achieve orgasm, although orgasm is much less likely in women with LMN injuries affecting the S3–S5 segments.53,110,221,222
Fertility in men with SCI is impaired, in part because of a decreased ability to ejaculate.181 Semen quality has also been found to be poor in men with SCI, with decreased sperm motility, decreased mitochondrial activity, and increased sperm DNA fragmentation.183 Reasons for altered semen quality have been postulated to include seminal fluid stasis, testicular hyperthermia, recurrent genitourinary tract infections, and hormonal dysfunction.183 Fertility in women with SCI is preserved once menstruation resumes, on average about 5 months postinjury.15
Stroke
Stroke is the world’s second leading cause of death and the leading cause of adult disability.54 Sexual dysfunction is a common finding after stroke in both men and women (see Chapter 50). The most common findings for men are erectile and ejaculatory dysfunction (in 40% to 50%) and decreased sexual drive.115,127,145,233 Women tend to experience decreased sexual drive, decreased vaginal lubrication (in approximately 50%), decreased orgasm (in about 20% to 30%), and decreased overall sexual satisfaction.123,127,145,233 The prevalence of decreased sexual drive has been reported to be between about 25% and 60% in both genders after stroke.123,127 Stroke also leads to significantly decreased frequency of sexual activity in both genders, and in one study, approximately 50% of stroke survivors reported no sexual activity whatsoever by 1 year poststroke.86,127,233
The physical effects of stroke that contribute to sexual dysfunction include hemiparesis with its effect on body positioning and movement, hemineglect, hemianopsia, neurogenic bowel and bladder, and spasticity.163,181 Not much is known about the functional neuroanatomy of sexual behavior and control, but some studies have indicated that the right cerebral hemisphere might play a more important role in sexual functioning than the left side.57,83,115 Many studies have suggested that sexual dysfunction after stroke is related to the presence of medical comorbidities (cardiac disease, diabetes, hypercholesterolemia, depression), medications, and psychosocial factors (inability to discuss sexuality with the partner, unwillingness for sexual activity, fear of another stroke, sexuality being unimportant) rather than the direct effect of stroke.∗
Traumatic Brain Injury
The prevalence of sexual dysfunction after traumatic brain injury has been reported at 4% to 71%, a wide range that likely represents the limited number of quality studies and the varied types and severities of injury that are possible201 (see Chapter 49). Types of sexual dysfunction reported have been similar to those seen in patients with stroke, including reduced sexual desire and frequency of sexual activity in both genders, ED and ejaculatory dysfunction in men, and dyspareunia, anorgasmia, and reduced lubrication in women.104,128,181,201 In addition, brain injury can cause hypersexual behavior such as excessive masturbation. This can occur in particular with injury to the limbic system or prefrontal regions, which can cause disinhibition; or to bilateral temporal poles, which produces the Klüver-Bucy syndrome of hypersexuality and hyperorality.46,137,217 The prevalence and type of sexual dysfunction can be associated with both the global amount of brain tissue destroyed and the focality of injuries.181 Sexual dysfunction does not seem to correlate with the amount of cognitive impairment, the length of posttraumatic amnesia, or the burden of neurologic disability.40,181,201 Medications, particularly anticonvulsants, can greatly contribute to the sexual dysfunction witnessed after brain injury.89 Psychosocial factors seems to play a major role in sexual functioning after brain injury, with the presence of depression being the most sensitive indicator for sexual dysfunction.104 Other important psychologic factors include perceived health status and quality of life, low self-esteem, anxiety, and perceived decline in personal sex appeal.104,129
Multiple Sclerosis
Multiple sclerosis (MS)-induced sexual dysfunction is present in 40% to 80% of women and 50% to 90% of men66 (see Chapter 52). Women tend to have decreased sexual desire, anorgasmia, decreased vaginal lubrication, and increased spasticity with sexual activity.61,107,181 Many of these symptoms are thought to be related to the decreased genital sensitivity experienced by 62% of women with advanced MS.107 Men with MS have ED, ejaculatory dysfunction (premature, delayed, or absent), orgasmic dysfunction, decreased genital sensation, and decreased sexual drive.61,181
The sexual disorders have historically been attributed directly to the location and duration of the spinal cord or brain lesion, but more recent research tends to describe a multitude of other factors that also contribute to the development of sexual dysfunction in MS. These include secondary physical limitations, psychologic factors, and the side effects of MS medications.134,227 In one study, sexual dysfunction in men with MS was found to be positively correlated with lower-limb disability and bladder dysfunction, but in women the sexual disorders were most strongly correlated with fatigue.80 Secondary physical limitations include fatigue, bowel and bladder dysfunction, muscle weakness, spasticity, poor coordination, inability to properly position oneself for an enjoyable sexual encounter, numbness, paresthesias, pain, and cognitive impairment.134,227 Psychosocial factors that significantly contribute to MS-related sexual dysfunction include poor self-image, poor self-esteem, fear of isolation and abandonment, shame, dependency on one’s partner to provide for one’s basic needs, and depression.204,227
Other Neurologic Disorders
Parkinson’s disease (PD) is often associated with low testosterone levels, and therefore decreased sexual drive163 (see Chapter 51). In one study of young men with PD (ages 36 to 56 years), up to 40% had low sexual desire. Men with PD also can experience ED and PE.181 Treatment with dopamine and dopamine agonist medications, on the other hand, has been documented to cause hypersexual behavior, which often accompanies mania.238 Hypersexuality has also been described with deep brain stimulation of the subthalamic nucleus.185
Patients with epilepsy can exhibit involuntary sexual gestures, erotic feelings, and orgasm during seizure activity.181 These dysfunctions are most commonly seen with complex partial seizures arising from the temporolimbic or frontolimbic circuitry.181 Ictal genital automatisms (such as self-fondling or pelvic thrusting) were reported in one study to occur in 11% of patients observed with video electroencephalographic monitoring.69 Ictal orgasm has been reported much more frequently in women than in men.181
Peripheral neuropathy can cause sexual dysfunction, particularly when the etiology is diabetes, amyloid, and some of the inherited neuropathies with urogenital symptoms as prominent early features.181 Guillain-Barré syndrome has been linked to ED when there is residual neurologic deficit or disability after recovery.50
Chronic Pain
The reasons for sexual dysfunction in patients with chronic pain are multifactorial, often related to physiologic, pharmacologic, and psychologic factors173 (see Chapter 42). In one study, 73% of patients with chronic pain had pain-related difficulty with sexual activity. The reasons for this included decreased arousal, positioning issues, exacerbations of pain, low confidence, performance worries, and relationship issues.9 In another study, sexual problems were reported in 46% of patients with low back pain.71 Women with low back pain have been shown to have decreased frequency of sexual activity, more pain during sexual intercourse, and decreased sexual desire compared with men with low back pain or patients of either gender with neck pain.143 Sexual dysfunction in patients with chronic pain has been correlated most strongly with the presence of depression, poor coping skills, and shorter pain duration.130 Many of the medications used to treat chronic pain (including opioids, antidepressants, and anticonvulsants) can independently contribute to sexual dysfunction.235 Chronic pelvic pain in women, which frequently causes dyspareunia and other sexual dysfunctions, can be related to childhood physical abuse, sexual abuse, and emotional neglect. It can also have an organic etiology (as detailed previously in this chapter).133
Rheumatologic Disease
Osteoarthritis affects sexual function primarily through associated joint pain, stiffness, and fatigue, and the hip joint is the most often implicated in leading to sexual difficulties38,60,163 (see Chapter 36). Total hip replacement often significantly improves sexual functioning; in one study, 65% of patients found relief from sexual difficulties after the surgery.231 It is important to instruct patients in proper positioning after joint replacement to reduce the risk of dislocation, and many surgeons instruct patients to refrain from sexual intercourse for 1 to 2 months after hip replacement for this reason.220
Rheumatoid arthritis (RA), like osteoarthritis, can cause problems in sexual functioning through joint pain, stiffness, and fatigue.166 RA in men has also been shown to be associated with decreased sexual desire and ED during periods of active inflammation.93 One recent study of women with RA identified 62% with difficulties in sexual performance caused by joint pain and stiffness, and 92% with diminished sexual desire or satisfaction.2 Difficulties in sexual performance were related to the overall level of disability and hip involvement, whereas decreased sexual desire and satisfaction were correlated more with perceived pain, age, and depression.
The effect of fibromyalgia on sexual dysfunction in women has been looked at in one recent study,172 which found that 97% of women with fibromyalgia reported sexual dysfunction, including decreased sexual desire, arousal, and orgasm. The degree of sexual difficulty was found to be very strongly correlated with the degree of depression. Other correlates included level of anxiety, age, pain intensity, and marital and work status.
Amputation
Patients with limb amputation usually have preserved sexual genital functioning (unless there is a comorbid condition such as diabetes or cardiac disease, or the side effects of their medications play a significant detrimental role)108 (see Chapters 12 and 13). But their sexual life can be significantly affected by a variety of factors associated with their amputation, including depression, poor self-esteem and body image, phantom sensations and pain, problems with balance and movement, and difficulties with body positioning during sexual activity.212 Preservation of the knee joint can be helpful for maintaining balance during sexual intercourse, although transfemoral amputees can use pillows to aid in positioning.48 Upper limb amputees would benefit from side-lying or supine positioning to allow for free movement of both the intact arm and the residual limb.220
Diabetes
Diabetes mellitus (DM) is one of the major comorbidities affecting people with disabilities, because its presence is a significant risk factor for subsequent stroke and amputation. DM plays a clear role in the development of sexual dysfunction in men. ED is three times more common in men with DM than in the general population, with prevalence estimates ranging from 35% to 75%.30,144,227 PE has also been documented in 40% and hypoactive sexual desire in 25% of men with diabetes.144 Diabetes-related sexual dysfunction in men is strongly correlated with glycemic control, duration of disease, and burden of diabetic complications.30 The pathogenesis of sexual dysfunction in DM is likely multifactorial, including vasculopathy, autonomic neuropathy, and diminished nitric oxide production, which leads to decreased neurogenic vasodilation.13,227
Diabetes in women has a much less clear effect on sexual functioning, as research is limited and at times contradictory.163 The most commonly reported condition is sexual arousal disorder, with its accompanying decreased vaginal lubrication.13 Low sexual desire, decreased clitoral sensation, orgasmic dysfunction, and dyspareunia have also been infrequently reported.51 Factors for the development of sexual dysfunction in women with diabetes have been analyzed, and a far different picture has emerged than for men with diabetes. There has been no documented correlation to body mass index, presence of diabetic complications, length of disability, or level of glycemic control.13,72,73 Associations have been shown for cardiovascular comorbidity, depression, and age.240
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








