CHAPTER 77 Septic Arthritis
GENERAL CONSIDERATIONS
An infection can be defined as the clinical manifestation of a host response to a given inoculum. Aspects of the inoculum include the amount of bacteria, the type of entry, and the nature or virulence of the pathogen. Host factors can be classified as congenital or acquired. Congenital immunoincompetence syndromes are associated with deficiencies of the humeral or bursal immunologic systems and have been well described in standard medical textbooks. Acquired failures or alteration of immunocompetence can be either generalized or localized. Generalized processes include diabetes mellitus, corticosteroid therapy, cancer with or without im-munosuppressive therapy, human immunodeficiency virus (HIV) infection, and alcohol or other chemical addiction or abuse. Local processes that alter normal host resistance include anatomic site of involvement, scar formation from previous surgery, burns, radiation, or prior infection. In applying these observations specifically to the elbow, it should be noted that this is a subcutaneous joint. Hence, the elbow is vulnerable to direct inoculation of a pathogen, particularly because host resistance is compromised. In fact, a recent analytic assessment of a 10-year study of infections in England documented an 11% incidence of death with joint sepsis. Of great interest is that a multivariant analysis documented risk factors for mortality to be confusion at presentation, age greater than 65 years of age, multiple joint involvement, and interestingly, involvement of the elbow joint.78
DISEASE-MODIFYING ANTIRHEUMATIC DRUGS
Infection and DMARDS are well known to have dramatically changed the life and prognosis of patients suffering from rheumatoid arthritis. Yet, the orthopedic surgeon is very well aware of the potential adverse effects, both with regard to increased risk in surgical infection, as well as the potential for managing patients with spontaneous sepsis related to this type of medication. In spite of the opinion or perception of the orthopedic community that these agents are responsible for an increased infection rate, the literature is somewhat controversial in this regard.7 One can find as many references that fail to support the relationship between DMARDs and infection as exists to demonstrate that this relationship does exist.7,14,18,19,25 One recent study does reveal that treatment with the tumor necrosis factor (TNF) inhibitors does significantly increase the risk of infection in orthopedic surgery (<0.04).
Our review of the current literature leaves us to conclude that without any question, DMARDs do increase the potential for infection about the elbow. Although this may not be demonstrable for the hip, a fivefold increased risk for elbow infection has been documented.18 Interestingly it has also been noticed that the skin and soft tissues are also potentially at greatest risk.19 Thus, increased problems with wound healing around the elbow supports the increased incidence of infection.
The biggest question that remains unanswered is whether or not withholding the medication in advance subsequently has an effect on this phenomenon. There is evidence that methotrexate need not be withheld,29 whereas others have demonstrated that there is merit in withholding methotrexate therapy in the perioperative period.14
EXPERIENCE AT THE MAYO CLINIC
We are currently in the process of analyzing our experience with infected total elbow arthroplasty and the use of DMARDs. The difficulty of our and all such studies is knowing whether medications behave the same in different patients. To what extent is the drugs effect dose dependent, as appears to be the case in some instances? A study from the Mayo Clinic did demonstrate that the dose itself can be a very significant variable that influences the development of an infection with TNF antibody therapy.7
AUTHOR’S RECOMMENDATION
Based on our review of the literature and our clinical experience, there is little question in our mind that the anti-TNF agents are associated with increased orthopedic infections. For this reason, we do withhold treatment for at least a month before and a month after our surgical intervention. Although we believe that the increased incidence of sepsis is becoming well documented, what is less well known is whether or not all agents have the same adverse impact and whether withholding these agents is of value. What is the “safe period” both before and after surgery? It is hoped that this issue will be resolved over the next several years, but as mentioned earlier, because of the numerous variables that pertain to the issue, it is likely to be debated for many years to come.
OSTEOMYELITIS
Bone infection occurs (1) hematogenously, (2) by direct inoculation after surgery or open fracture, or (3) by contiguous spread from a local process.77
HEMATOGENOUS INFECTION
Hematogenous infection is the most common type of osteomyelitis and has been reported to occur at the elbow in about 4% of such cases.77 In the growing child, the end-arterial loop of the metaphyseal bone causes sluggish bone blood flow. The lack of phagocytic activity in these loops allows maturation of a septic thrombus at the arterial site.37 The abscess spreads through the haversian system into the subperiosteal space. If the metaphysis is intra-articular, as at the hip or shoulder, a septic joint will then result,75 but this is not the case at the elbow. As at other sites, acute hematogenous osteomyelitis is most common in children younger than 3 and older than 7 years of age. The first group is vulnerable owing to the lack of acquired host immunity; the second age group corresponds to the time of rapid growth.51 Our recent study reported 85% septic joints in children were of the knee, hip and ankle; only 8% involved the elbow.11
Presentation and Diagnosis
The clinical presentation is typical and includes local pain, warmth, and swelling. The patient may be afebrile but is not necessarily systemically ill. In children, a predisposing, traumatic event is common,50,83 but identity of a remote focus is less frequent. The elbow is held in flexion and pseudoparalysis, or reflex inhibition may be present. The physical examination includes the following:
Except in the very acute stages, an elevated leukocyte count is variably present,15,53 and the differential count tends to demonstrate a shift to the left in two thirds of the cases. The erythrocyte sedimentation rate has been the most sensitive blood test; it is elevated in the early stages of infection in about 80 percent of persons.15,52 Therefore, it is very sensitive, but not specific. Interestingly, the rate is statistically higher in joint infections than in bone infections and is a valuable means of following the treatment and resolution of the infection.15,41,50 Early radiographs are not helpful. After 7 to 14 days, osteoporosis may be present, followed by periosteal elevation or erosions.
The classic appearance of osteomyelitis by bone scan is a well-defined focal area of increased uptake at the site of active infection (Fig. 77-1). The 99mTc scan may be positive as early as 24 hours after the onset of symptoms in a patient with osteomyelitis.24 The increased activity of equal intensity on both sides of the joint indicates joint disease, arthritis, or synovitis but is not a reliable indicator in the neonate. Nonspecific inflammatory arthritides of rheumatoid arthritis or gout limits the value of the Ga scan.34 False-negative results are also common.72 At the present time, we recommend first a 99mTc scan as a low-cost screening test to provide immediate results and localization. The 111In-labeled leukocyte scan may be useful primarily for more acute suppurative infection. More recently, Erdman states that magnetic resonance imaging (MRI) has 100% sensitivity and 0% specificity in a mixed group of acute and chronic osteomyelitis.17
With the continuing advances being made with imaging techniques, it is currently believed that the MRI and nuclear medicine are the most sensitive and specific modalities for detection of the septic process. MRI is most helpful to determine the extent of damage, and ultrasound is an effective, noninvasive method to assess soft tissue involvement. Computed tomography (CT) helps document sequestra. The newer positron emission tomography (PET) and single photon emission computed tomography (SPECT) are emerging as useful to evaluate chronic conditions.59,71 The T1-weighted images of the MRI are also very useful to detect concurrent osteomyelitis in the presence of the septic joint.38 Ongoing efforts to refine short time inversion recovery (STIR) and T1 spin echo (T1 SE) imaging techniques reveal enhanced sensitivity, specifically for osteomyelitis.45 Joint aspiration remains the most simple and reliable means of making the diagnosis of elbow joint sepsis, but even this is positive in only about 85% of cases.78
SPREAD FROM A CONTIGUOUS FOCUS
Infection by spread from a contiguous focus occurs at the elbow from a septic joint or from an infected olecranon bursa. A recent survey of a 10-year experience with septic bursae from Spain documented that three of 69 patients (7.7%) developed osteomyelitis.21 These circumstances are most commonly noted in a patient with rheumatoid arthritis, and the management is the same as that for a septic joint. Because a sympathetic sterile effusion may occur with metaphyseal osteomyelitis, even though the metaphysis is extra-articular, the joint should be aspirated to exclude septic arthritis in the presence of an effusion.
MICROORGANISMS
The most common pathogen causing acute hematogenous osteomyelitis is Staphylococcus aureus. Opportunistic organisms are isolated in the debilitated patient, and Pseudomonas aeruginosa is most commonly associated with drug addiction or chronic, draining wounds. Organisms not generally considered pathogenic must be viewed as such when isolated on several occasions, particularly in patients with compromised resistance. In one report, two of the three cases of diphtheroid osteomyelitis involved the elbow, and both patients had altered local immunocompetency.52 Serratia infection of open fractures has also been reported in the humerus and forearm in about one third of such cases.40 The infected prosthesis is discussed in Chapter 62.
TREATMENT
For the elbow, there are no unique management features of acute hematogenous osteomyelitis, except that prolonged immobilization is to be strictly avoided. In cases that are diagnosed early, antibiotics alone may be adequate.6,53 Surgery is indicated when there is no response to parenteral antibiotic therapy after 36 to 48 hours. It has been our experience that acute hematogenous osteomyelitis in which symptoms have been present for less than 10 days may be treated with specific intravenous antibiotics for 2 to 3 weeks. If symptoms have been present for more than 10 days, a discrete soft tissue or bone abscess may have developed and must be surgically decompressed. Subperiosteal needle aspiration is sometimes helpful in accurately defining metaphyseal infection. Today we rely on the MRI to assist in the early diagnosis of bone involvement.20
Intravenous antibiotics should be continued for about 3 weeks. Oral agents can be used for an additional 4 weeks, but bactericidal levels should be attained and monitored.43 Infection involving bone may become subacute or chronic, and in this instance, incision and drainage with limited bone débridement and secondary soft tissue healing may be necessary. An extensive débridement of bone severely impairs function because the joint becomes dysfunctionally unstable and is difficult to fuse (Fig. 77-2). Burkhalter and colleagues60 have discussed the upper extremity restrictions of function created by elbow fusion and the common complications of failure of union and secondary fracture (see Chapter 70). They recommended a posterior compression plate and pointed out that often the hardware is exposed during the process of healing of the fusion. They also accurately emphasize the limited indications for and the occurrence of forearm motion loss after arthrodesis.60 Occasionally, spontaneous arthrodesis occurs after débridement, but extensive removal of bone causes gross instability (Fig. 77-3). If soft tissue coverage is a problem, the flexor carpi ulnaris muscle pedicle flap may be used for coverage of the proximal ulna and elbow. Fourteen centimeters of muscle is available from the pedicle entering 5 cm distal to the elbow joint line. Such a flap brings improved blood supply as well as soft tissue coverage.49
In the acute phase of treatment, the joint should be splinted, elevated, and put to rest. As the process resolves, gentle active motion is encouraged as soon as possible. Continuous passive motion may prove to be beneficial in some patients to avoid ankylosis or adhesions.64
RESULTS
In the preantibiotic area, Wilensky80 reported that three of 18 patients developed spontaneous ankylosed elbows owing to immobilization for osteomyelitis of the elbow region. Other long-term residual effects include sinus tract formation, recurrent infection, pathologic fracture, growth disturbances, and development of chronic osteomyelitis. West and associates79 observed that chronic osteomyelitis of the humerus appears to have a better prognosis than chronic infection of the tibia or femur. The duration of the septic process is the most important prognostic feature.53,57 Today, it is anticipated that better function will be realized with better techniques for early detection.
SEPTIC ARTHRITIS OF THE ELBOW
Septic arthritis after joint replacement51 is discussed in Chapter 62. In the experience at the Mayo Clinic, septic arthritis of the elbow occurred in 6% of adults39 and 3% of children diagnosed with septic joints.50 Other investigators report an incidence of 9% to 13%,3,26,78 noting that the ages at risk were those “at the extremes of life.”3 The frequent association of septic arthritis with rheumatoid arthritis is well recognized.30,31,42,61,68 This association is believed to be even more likely in those treated with DMARDs. Kellgren and colleagues42 reported that 33% of septic joints in patients with rheumatoid arthritis involved the elbow. Also noted were the multiple sites of involvement and the high incidence of Staphylococcus aureus organisms (83%).
DIAGNOSIS
An incorrect or delayed initial diagnosis is common.39 The clinical examination and an index of suspicion are crucial for a prompt and correct diagnosis. The maximum capacity of the joint is at about 80 degrees of flexion,55 so the patient will present with the joint held in this position. Pain and swelling about the elbow are invariably present, and gentle, passive motion is painful.
Differential diagnosis of an infected elbow in the child includes juvenile rheumatoid arthritis, unrecognized trauma, acute rheumatic fever (which affects the elbow in about 15% of cases), and transient synovitis. In the adult, 5% of patients with gout or pseudogout will have involvement of the elbow. The occurrence of elbow sepsis in those with immunodeficiency is also becoming recognized.10,22,60 Differentiation from osteoarthritis or post-traumatic arthritis should not be a difficult problem. An additional differential diagnosis is nonsuppurative infectious arthritis; such as that associated with Lyme disease and hepatitis or from mycobacterium.87 Gonococcal arthritis is suspected with appropriate sexual history. Rheumatoid arthritis with a secondary infection is, of course, a difficult clinical diagnosis that is usually resolved only with aspiration.
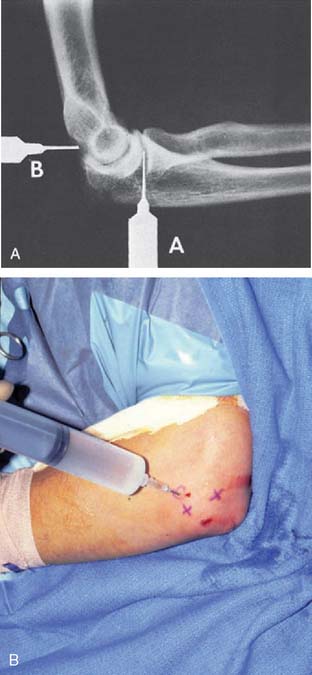
Systemic symptoms are variably present. A leukocytosis is often present early, but the shift to the left of the differential leukocyte count is more reliable. The sedimentation rate is invariably increased, but this does not distinguish the patient with active rheumatoid arthritis.15 Even the infected joint replacement shows elevated sedimentation rates, but the effect of the surgery itself is sometimes a source of confusion.66 As with any joint infection, the key to the diagnosis is joint aspiration. The distended joint is easy to enter either from the lateral “triangle” or at the posterior olecranon fossa (Fig. 77-4). Joint aspiration must be done under sterile conditions, because inoculation of the sterile joint is possible with aspiration and has been reported.3
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree