CHAPTER 72 Spastic Dysfunction of the Elbow
CEREBRAL PALSY
Cerebral palsy (CP) is a nonprogressive perinatal injury to the developing central nervous system (CNS). CP produces motor dysfunction, movement disorders, weakness, and impaired function.36 The incidence of CP is 1 to 7 per 1000 children worldwide, and 2 to 3 per 1000 in developed countries.33 The incidence has been fairly constant over the past 40 years; a lesser incidence due to improved prenatal and perinatal care, balanced with a greater incidence of enhanced survival of the very preterm births, has lead to a net constant incidence over time.7
The etiology of CP has been described as a causal pathway with a sequence of conditions culminating in injury to the CNS. A recent 15-year review of the incidence of CP determined that risk factors for preterm infants were periventricular leukomalacia (magnetic resonance imaging evidence of brain structural changes), prolonged rupture of membranes, and patent ductus arteriosus. Risk factors for infants with a gestational age of greater than 34 weeks included size small for gestational age, neonatal transfer (patient transfer at birth from the hospital where they were delivered to a hospital with higher levels of care), and a history of sepsis or meningitis.39
CP is most commonly classified by its anatomic distribution (Box 72-1). Diplegic refers to involvement of both lower extremities. Hemiplegic is involvement of one upper and one lower extremity on the same side. Triplegic is involvement of one upper and both lower extremities. Quadriplegic is involvement of all four limbs. The type of muscle tone is attributed to manifestations of CNS dysfunction and further classifies the disorder to include spasticity, dystonia (athetosis), flaccidity, or mixed patterns.
BOX 72-1 Simple Classification of Cerebral Palsy
Geographic Distribution
*Hemiplegia: principally one-sided (one arm, one leg)
Diplegia: principally lower extremity involvement (two legs)
Triplegia: one arm and both legs involvement
Life priorities for individuals with CP differ due to their motor system disabilities. According to Bleck, the top four self-reported life priorities for individuals with CP were, in order of importance, (1) communication with others; (2) ability to perform activities of daily living, particularly personal hygiene; (3) mobility in the community; and (4) walking.2 As our society becomes more technologically sophisticated, use of the upper extremities becomes more critical. Care of the patient with CP has shifted toward an increased emphasis on improved upper extremity use.
DIAGNOSIS
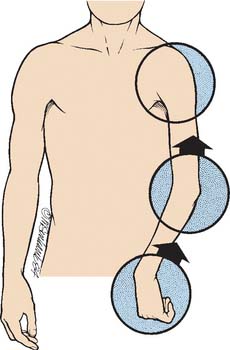
CP is a disorder of the CNS that manifests itself in peripheral motor dysfunction and joint malpositioning. In spastic hemiplegia due to CP, the most common peripheral manifestations in the upper limb are shoulder internal rotation, elbow flexion, forearm pronation, wrist flexion/ulnar deviation, finger clenching (flexor spasticity), swan-necking, and thumb-in-palm deformity, as shown in Figure 72-1. Increased muscle spasticity causes muscle imbalance across joints, which initially leads to impaired function and eventually causes joint contractures with skeletal deformity. The typical elbow deformity of CP is elbow flexion and forearm pronation. Occasionally, it results in posterior dislocation of the radial head,32 which requires no treatment unless in adult life it results in a painful bursa; then the radial head may be excised. Flexion-supination contractures of the elbow can occur but are rare in CP.
CLINICAL ASSESSMENT
Physical examination includes assessment of passive range of motion, active range of motion, muscle tone/control, and overall function of the limb (including hand function assessment). The limb is first examined for passive range of motion of the shoulder, elbow, forearm, wrist, and hand, evaluating for joint and muscle contractures. Even if only the elbow is to be treated, the shoulder, forearm, wrist, and hand need to be assessed because they are essential for the individual to effectively use the upper limb. Muscle tone is noted through the passive evaluation of joint mobility. Passive range of motion needs to be done slowly to overcome muscle spasticity with gentle sustained resistance. Assessment for muscle and joint contracture by passive mobility of the joint and passive stretch of the muscle is performed. The tightness and contracture of some of the muscles around the elbow can be easily palpated, particularly the biceps, brachialis, brachioradialis, and pronator teres.
DEFINITION OF GOALS
In the past, sensory deficiencies of the hand were believed to be a contraindication to surgery in CP. If tested carefully, sensory deficiencies are present in nearly all children with CP.42 Several recent studies have shown that impaired sensation is not a contraindication to surgical intervention in the patient with CP.6,8,42 Appropriate consultation or multispecialty approach to care should be considered before considering surgical intervention. Several alternatives to surgical intervention exist and should be considered. Exploration of the treatment pros and cons may require discussions that include the rehabilitation physicians, neurologists, and neurosurgeons to adequately explore the options of tone reducing medications (diazepam [Valium], baclofen), tone-reducing injections (botulinum toxin, phenol), tone-reducing neurosurgery interventions (selective dorsal rhizotomy), or therapy interventions (splinting, stretching programs). At many institutions, a spasticity management team of specialists is involved with patient evaluation for tone-reducing interventions, and helps guide the orthopedic surgeon as to other treatment alternatives.
TRAUMATIC BRAIN INJURY
Most often, brain damage acquired in childhood is the result of trauma. The associated spasticity usually does not reach its maximum point until 1 to 2 months after the incident; then muscle tone may gradually decrease during the next 2 years.22,23
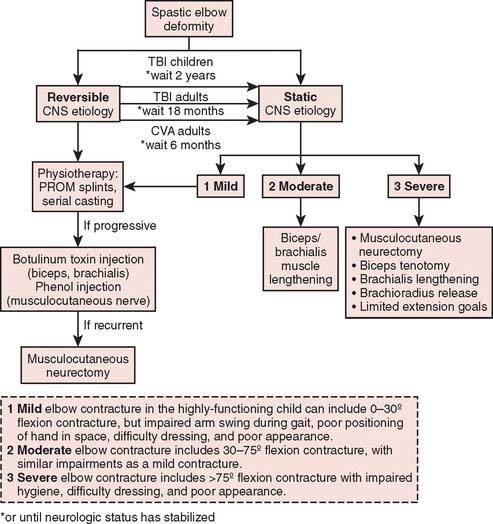
Irreversible surgical procedures should not be performed in children with acquired brain damage in the first 2 years after the insult. During this period, serial casting or splinting can be combined with botulinum toxin or phenol injections to deal with elbows with significant flexor tone. Another problem in children with acquired brain injury is heterotopic bone formation, usually about the anterior aspect of the elbow.35 Unlike adults, most children eventually resorb the heterotopic bone. Therefore, we recommend gentle motion and re-evaluation at least 6 months before any attempt is made at excision.
STROKE AND HEAD TRAUMA IN ADULTS
Stroke and head trauma produce permanent impairment in approximately 3 million adults in the United States. Abnormal elbow function due to spasticity and loss of motor control is a common disability. The surgeon treating these conditions must be fully cognizant of the complex rehabilitation process after CNS illness, particularly hand rehabilitation. Surgery is undertaken only after careful assessment of the many factors that determine the patient’s potential to use the limb.3
Substantial neurologic recovery generally follows strokes and head injury. In stroke patients, most neurologic recovery is completed in the first 6 months; in head trauma, patients’ substantial recovery extends over the first year and a half.17 Definitive surgical procedures to improve function are deferred until after the patient’s neurologic condition has stabilized and he or she has learned to cope with the disability and has received appropriate nonoperative therapy.
Prevention of elbow muscle and joint contractures is paramount. Nonoperative therapy should include passive range of motion, splints, and serial casts; if progressive elbow flexion deformity develops before neurologic recovery, then botulinum toxin of the biceps and brachialis or phenol injection of the musculocutaneous nerve is performed.13 Elbow flexion contracture due to spasticity is the most common problem that ultimately requires surgical attention, because it commonly affects patients with nonfunctional hands. Surgery is indicated to correct contracture deformities that interfere with hygiene or cause pain; rarely, it is used to improve cosmesis. Operative intervention is usually deferred until neurologic recovery is complete, which is in 6 to 18 months.
PREOPERATIVE EVALUATION
Dynamic electromyography19,38,41 is becoming increasingly useful because it enables surgeons to determine more precisely which flexor muscles are responsible for a deformity (Fig. 72-2) or whether surgical ablation of a given muscle will be effective.26 Kozin et al reports its use in distinguishing spasticity patterns of the brachioradialis, biceps, and brachialis. This information is particularly valuable for patients with functional elbow motion because it enables the surgeon to release or lengthen only the muscles most involved and to preserve those that are less involved. Slow and fast volitional elbow flexion and extension are assessed. Attempts to move the elbow rapidly enhance an abnormal flexor response.
Last, preoperative evaluation always includes a detailed assessment by a therapist and/or cooperation with a spasticity management team: evaluation of motor and perceptual function of the elbow, hand, and shoulder and examination of cognitive, vocational, and social factors that are important determinants of arm function and treatment goals.
TREATMENT OPTIONS
Treatment of the spastic elbow includes several options. If the deformity is not fixed, and the major goal is reduced muscle tone to improve joint position and function, the elbow flexor tone can be diminished by several methods. Tone-reducing medications (Valium, baclofen) would be indicated if the overall global tone is severely affected; consultation with a neurologist or rehabilitation specialist to initiate this treatment would be indicated. Mild elbow contractures can be diminished by range-of-motion stretches and elbow splinting; referral to a physical or occupational therapist to initiate this treatment would be indicated.1
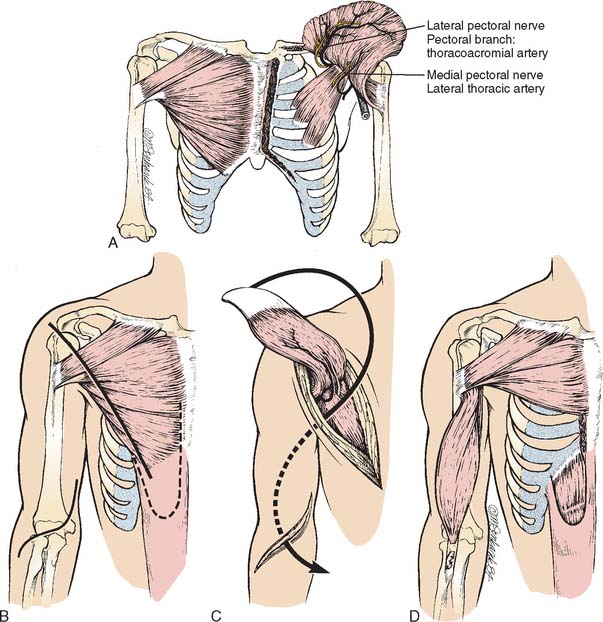
Tone reduction specifically localized to the elbow can be achieved through the use of botulinum toxin injections, and phenol injections; a more permanent tone reduction can be achieved with neurectomy or muscle-lengthening procedures. Muscle-lengthening procedures are the most common surgical procedure performed in the elbow for CP. In order to reduce the flexion posturing of the elbow, lengthening of the biceps and brachialis would be indicated. If the flexion posturing includes pronation deformity of the forearm with wrist flexion and finger flexion posturing, then a flexor pronator slide would be indicated.
As shown in Figure 72-3, timing of surgical intervention is critical and depends on the presenting diagnosis. Because spasticity develops as a consequence of an upper motor neuron dysfunction in the CNS, it is imperative that neurologic recovery is complete before definitive surgical interventions are performed. Botulinum toxin injections and phenol injections are often recommended as temporary measures during neurologic return, or as interventions in the growing child with worsening contractures. Definitive surgical procedures include musculocutaneous neurectomy or elbow muscle lengthenings of the biceps, brachialis, or brachioradialis muscles or flexor pronator slide. Heterotopic ossification of the elbow can occur with traumatic brain injury or stroke, and is discussed as well.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree