CHAPTER 24 Radial Head Fracture
PART A General Considerations, Conservative Treatment, and Open Reduction and Internal Fixation
INTRODUCTION
HISTORICAL REVIEW
Before 1933,10 the literature has been well summarized by Schwartz and Young.110 The first description was probably made by Paul of Aegina (ad 625-690): “The ulna and radius are sometimes fractured together and sometimes one of them only, either in the middle or at one end as at the elbow or the wrist.”2 Early difficulty in making the diagnosis was encountered because of “thick muscle covering.”33,93 In 1891, Hoffa described two types of radial head fractures, displaced and undisplaced.55 Hoffa55 and Helferich50 recommended resection of the radial head for late deformity.
Three to 4 weeks of immobilization,122 passive motion, avoidance of “operative interference,”45 removal of the fracture fragment, and excision of the entire head for severe comminution54 were all recommended in the early 1900s. The first descriptions of a successful osteosynthesis of the fractured radial head was by Albin Lambotte in 1909.71 Other pertinent contributions include the suggestion that surgery is not a matter of election but rather of selection.54 Although much subsequently has been written about this fracture, the focus has changed to the more complex fractures.16,30,67
BIOMECHANICS AND FUNCTION OF THE RADIAL HEAD
Force Transmission
Studies in our laboratory have shown that, under the most demanding of circumstances, up to about 90% of body weight can be demonstrated across the radial head.84 The greatest amount of force transmission occurs with the forearm in pro-nation. This is because of a screw-home mechanism that occurs during pronation with proximal radial migration.
Stability
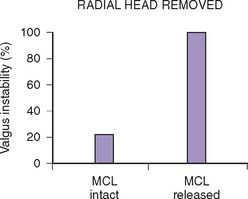
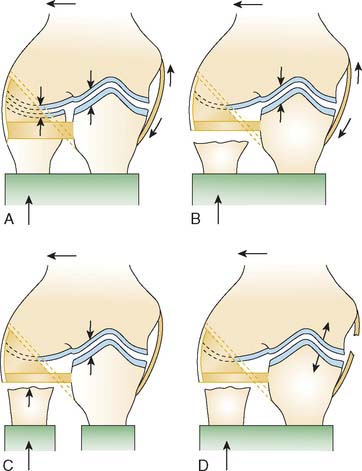
Traditional force-displacement studies have attributed 30% of the resistance to valgus stress to the radial head.57,83,96 Our studies have shown no significant resistance to valgus stability when the medial collateral ligament is intact. On the other hand, if the medial collateral ligament is deficient, the radial head is an important secondary stabilizer in preventing the elbow from dislocating.85 Other investigators115 have also shown a complementary relation of the lateral collateral ligament to the competency of the annular ligament. Therefore, the radial head may be considered a secondary stabilizer to valgus stress, and it does provide an important contribution to joint force transmission (Fig. 24-1).
INCIDENCE OF FRACTURE
Fracture of the radial head and neck has been variously reported as 1.7% to 5.4% of all fractures.27,66,86 Radial head fractures occur in about 17% to 19% of cases of elbow trauma134,137 and account for about 33% of elbow fractures.77 Approximately one in three cases is associated with another injury.127
Age and Sex
In general, about 10% to 15% of these fractures involve the neck,86,122,127 usually in children in whom the physis has not closed.15 Recent demographic data127 from our institution suggest some changes when compared with previously published reports.5,22,23,29,30,135 Gender ratio is approximately 1:1. The male population has more severe fracture types and more often sustain associated injuries. Compared with the literature,22,23,29,30 the age of patients sustaining radial head fractures has increased to a mean age of 45 years, 48 years old for women and 41 years for men.127
MECHANISM OF FRACTURE
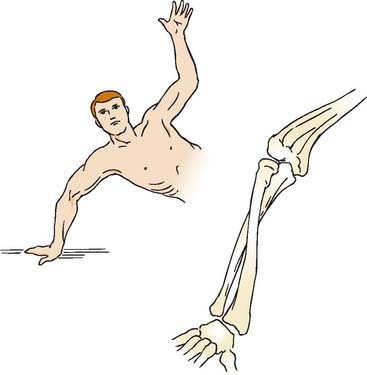
An axial load on the pronated forearm consistently produces a fracture of the radial head similar to that seen in clinical experience (Fig. 24-2).122 Odelberg-Johnsson88 observed precisely the same effect, noting that the fracture (1) occurred with posterior subluxation of the “forearm as far as the ligaments allowed,” and (2) involved the most anterior portion of the radial head when the forearm was pronated. Because the head of the radius is eccentric to the central axis of the neck,118 the posterolateral aspect of the radial head comes into intimate contact with the capitellum during pronation. The common occurrence of an anterolateral fracture fragment supports this theory.29,66 A direct blow is another uncommon cause of radial head fracture.29,41
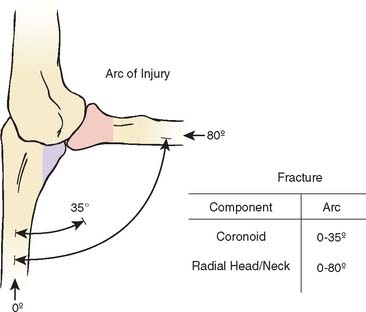
Amis and Miller3 recently enhanced our understanding of this and other fractures by correlating the fracture and the angle of flexion (Fig. 24-3). As is seen experimentally, either the coronoid or radial head may be fractured with the elbow in full extension, but the radial head can be fractured at greater degrees of flexion, approaching 80 degrees of the flexion arc.
ASSOCIATED INJURIES
CONCURRENT FRACTURES ABOUT THE ELBOW
Based on our assessment of 333 radial head fractures seen at the Mayo Clinic, we observed that the likelihood of associated injuries strongly correlates with the severity of the radial head fracture.127 The incidence of associated injuries increases from 20% in nondisplaced fractures to 80% in comminuted radial head fractures. The vast majority of these injuries (90%) are fractures about the elbow, mostly articular surface lesions. Approximately 20% of these articular injuries include the distal humerus, whereas in more than 90%, the proximal ulna is involved.
Fractures or cartilage injuries of the capitellum are common101,133 but not always appreciated.19 The associated fracture of the capitellum has been studied in some detail by Ward and Nunley.132 About one half of capitellar fractures were shown to have associated radial head fractures, whereas approximately 2% of radial head fractures had associated capitellar fractures. Thus, this combination is rather rare.127,132
Fracture of both the olecranon and the radial head is usually considered a variety of the Monteggia fracture and has been analyzed in detail by Scharplatz and Allgower108 and others.44,70,94,112
In 15% of patients, the radial head fracture is complicated by a coronoid fracture.127 Fractures of the coronoid have been discussed in detail by Regan and Morrey.100 If the fragment is large, significant elbow instability may occur.47,101,112
In our series, an elbow dislocation was found in about 15% of radial head fractures,127 as compared with approximately 10% quoted in the literature.1,7,27,29 Combined radial head and coronoid fractures are commonly seen in elbow dislocations. The coronoid process is involved in 80% of patients that sustain a radial head fracture as part of an elbow dislocation.
Bilateral radial head fractures are uncommon and occur in about 2% of patients.29,127
LIGAMENTOUS INJURY AT THE ELBOW
Some degree of ligamentous injury often occurs with radial head fracture; this association is not always fully appreciated (Fig. 24-4).17,49,65,88,133 An incompetent ulnar collateral ligament is suggested by an increased valgus position.22,86,109
Approximately 50% of associated lesions to the elbow involve clinically significant ligamentous injuries. About 10% of patients are diagnosed with a lateral or medial collateral ligament rupture, or a combination of both.127 These clinically relevant injuries are markedly less common than previously described.
Wagner130 observed 24 patients with calcification in the medial collateral ligament, and Arner and associates5 described a 12% incidence of ulnar collateral ligament calcification. Arvidsson and Johansson6 found ligament or capsular disruption by arthrography with various types of radial head fractures. Johansson65 demonstrated positive arthrographic findings in 4% of type I, 21% of type II, and 85% of type III injuries. Using magnetic resonance imaging in patients with types II or III radial head fractures, Itamura and associates63 recently found lesions in the medial collateral ligament in 54%, lateral ulnar collateral ligament in 80%, and lesions of both ligaments in 50%.
OTHER INJURIES
About 10% of patients with a radial head fracture sustain associated injuries other than elbow injuries. Fractures of the hand or wrist are found in about 6%.127 Conversely, radial head fractures are found in 6% of all scaphoid fractures.136 Shoulder injuries are uncommon (2%) and are usually found in nondisplaced radial head fractures.127
A ligamentous injury sustained at the distal radioulnar joint at the time of the radial head fracture15,28,116 is diagnosed in less than 1% of acute cases128 but is well recognized as the Essex-Lopresti injury and has been the subject of several reports.36,46,124 Shortening of 5 to 10 mm can be anticipated (Fig. 24-5).46 Open reduction and internal fixation to stabilize the proximal radius is recommended. Trousdale and associates125 reviewed Mayo experience with 20 patients. Fifteen had radial head resection without knowledge of the wrist injury. Such late detection was treated by reconstructive procedures, with a success rate of only 14%. Proper initial diagnosis was associated with an 80% satisfactory outcome and early treatment.
NEUROVASCULAR COMPLICATIONS
The uncomplicated fracture of the radial head is rarely associated with any neurovascular symptoms. Severe anterior displacement may affect the radial nerve, and a rare case of posterior interosseus nerve injury has been described in the literature.121
CLASSIFICATION OF FRACTURE
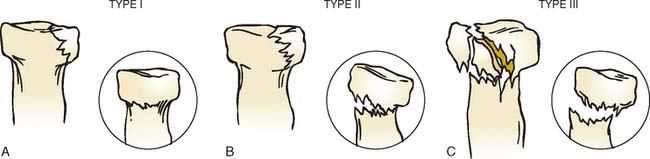
The first classifications of radial head fractures were described by Speed in 1924117 and Eliason in 1925.37 A year later, Cutler reported a second classification29 and this presented the basis for all currently used classifications. The most commonly used classification of radial head fracture is that proposed by Mason (Fig. 24-6).77 A fourth type, the fracture dislocation, was added by Johnston.66 In 1962, Johansson65 added the degree of displacement to his classification and this was later combined with the original Mason classification to form the most recent adaptation of the original Mason classification.57
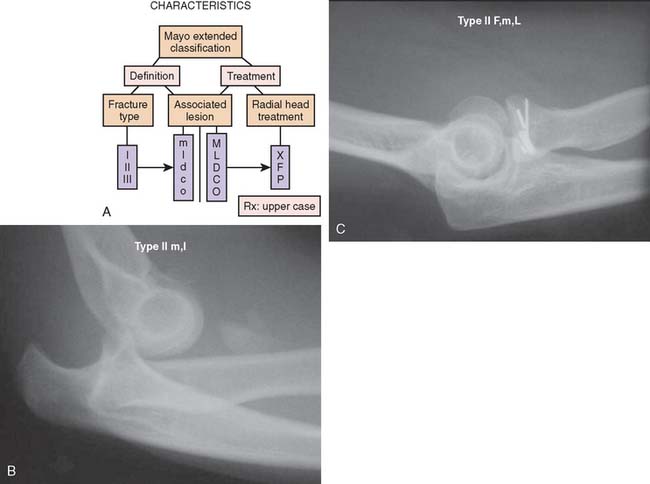
MAYO MODIFICATION OF MASON CLASSIFICATION
In the previous versions of this book, Morrey added a degree of sophistication to Mason’s classification of radial head fractures by dividing them into simple and complex fractures, depending on associated lesions.81,82 However, the division between simple and complex fractures can sometimes be difficult, for example, when suspected ligamentous lesions are not formally investigated due to the limited clinical implications.
Therefore, based on our clinical experience of more than 333 cases, we propose to add a suffix to the original fracture type in order to quantify associated lesions about the elbow.129
A suffix m is used if a medial collateral ligament injury is suspected or proven, but this has questionable impact on elbow stability. A capital M is used if there is an impact on stability, enough to warrant treatment. For lateral ligament injuries, l and L is used respectively. The same is done to document associated fractures to the ulna (U, u) or humerus (H, h). The suffix P is used to indicate that some sort of procedure was performed (Fig. 24-7); x for excision and F for ORIF.
FRACTURE MANAGEMENT
In general, the treatment of radial head fractures is based on the fracture type and the presence of any associated injury. These injuries involve the ligaments or articular elements with variable implications to prognosis and management (Fig. 24-8). Associated injuries should be treated on their own merit, and the following discussion will be limited to the treatment of the radial head fracture as such.
Clinical findings include hemarthrosis and painful rotation of the forearm, especially with palpation of the radial head. Radiographs are not always conclusive, but an elbow fat pad effusion in an otherwise normal radiograph is indicative of an occult radial head fracture in almost 90% of patients89 (Fig. 24-9). Computed tomography scanning may give additional information on the morphology of the fracture57,126 and may aid in planning and assessing the feasibility of a surgical reconstruction (Fig. 24-10).
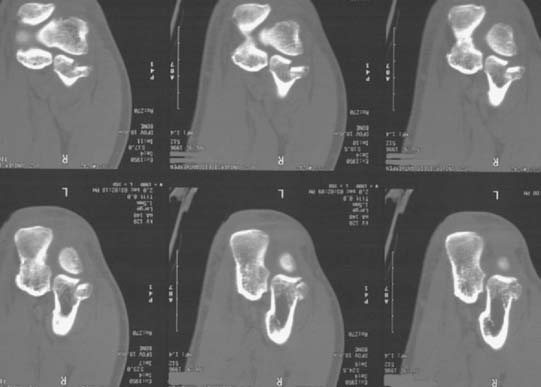
FIGURE 24-10 The computed tomography scan is extremely helpful to diagnose subtle associated articular injuries.
CONSERVATIVE TREATMENT
Conservative treatment of nondisplaced53 or minimally displaced radial head fractures52 has been shown to yield good results at a long-term follow-up of 21 and 19 years, respectively. Results of conservative treatment of displaced radial head fractures are less favorable, and patients have increased pain and decreased strength when compared with surgically managed patients.68,120
Sedation,111 mobilization,* or immobilization with78,98,114 or without111 a plaster cast have been advocated as conservative treatment options. Minor soft tissue injuries rarely need to be addressed.65,78,135
There is little question that the type I fracture (Fig. 24-11), because of its favorable prognosis and lack of concurrent soft tissue or other osseous injury, should be managed with early motion. Mason and Schutkin,76 reporting a military experience, found a mean period of disability of 4 weeks in 18 patients treated with early motion, compared with 7 weeks in seven individuals treated with 3 weeks of immobilization. Immediate mobilization is recommended, but a delay of up to 5 days has no functional implication after a 4-week follow-up.74
The major residuum is loss of extension rather than pain.29 Mason77 reported that about one third of his 62 patients with this fracture lost an average of 7 degrees of extension. This may be associated with hemarthrosis of the joint. In a cadaveric study, McGuigan and Bookout80 demonstrated a decrease in the flexion arc of 2 degrees per milliliter fluid injected into the elbow joint. To facilitate immediate motion, aspiration of the joint, is therefore recommended32,34,40,56,97 and pain relief could be increased by infiltrating some local anesthetic into the joint.27
The most frequent complication of conservative treatment of nondisplaced radial head fractures is degeneration of the articular surfaces, which is found at long-term follow-up in about 80% of patients.52,53 Other complications include displacement or nonunion102 (Fig. 24-12). Delayed excision of the entire radial head can be considered only if any of these complications become symptomatic (Fig. 24-13).26,52,53,102 Among 21 patients treated with delayed excision at the Mayo Clinic, Broberg and Morrey13 reported 75% with decreased pain and 77% with improved motion. The time to delayed excision ranged from 1 month to 20 years (Fig. 24-14).
A rare complication of nondisplaced radial head fractures treated conservatively is arthrofibrosis, which reportedly can be managed successfully with arthroscopic débridement.18,72
RESECTION OF THE RADIAL HEAD
The authors consider this issue somewhat controversial and unresolved. In general, resection is reserved for uncomplicated type III fractures (Fig. 24-15). Rochwerger and colleagues104 compared the treatment of 22 type II fractures. With mean surveillance of 5 years (2 to 23 years), osteosynthesis was found to be superior to resection, as the latter had satisfactory results in just more than 50% of cases. Similar results were found in 28 patients with type III, comminuted radial head fractures. Using a meticulous surgical technique, Ikeda et al60,61 found improved results in the group treated with open reduction and internal fixation (ORIF) over the group of patients treated with resection of the radial head.
Janssen et al64 reported 20 of 21 excellent or good results between 16 and 30 years after excision for comminuted radial head fractures. These investigators did exclude known dislocations. On the other hand, Sanchez-Sotelo et al106 described excision in the face of 10 dislocations, which is consistent with a Mason type IV classification. In this group, nine of 10 were considered satisfactory, similar to that of Janssen. However, they did note a 5-degree increased valgus carrying angle and early asymptomatic degenerative changes of the ulnohumeral joint with a mean of about 4.5 years surveillance (Fig. 24-16). There have been other recent reports regarding excision without radial head replacement that have yielded surprisingly consistent outcomes. A study from Scandinavia of 61 resections noted that the timing of the resection, whether acute or delayed, was much less important than the Mason classification of the lesion. Similar observations were made from Asia by Ikeda, who reported good results at 10 years after 15 patients (four with type II and 11 with type II treated by excision). They did, however, notice that pain was present in about a third of these patients52a and, as noted above, favor fixation.60,61 Wallenbock et al. evaluated radial head resection in 23 instances with a mean follow-up of 17 years with personal evaluation of the entire sample. They demonstrated that 22 of 27 patients had a satisfactory outcome. They observed those with resection after a type III or IV did less well than after a type II fracture. Interestingly, there was no distinction in their group and their observations whether the patients were treated by excision in the early or in the more chronic period.131 Similarly, a report from Italy by Celli of 31 fracture-dislocations noted that only 40% were satisfactory and 60% were unsatisfactory after various treatment options.24 This is consistent with Herbertsson’s observations that the fracture type has greater prognostic importance than the acuteness of the treatment.
The basic treatment rationale, therefore, of simple resection for those fractures that cannot be reduced and fixed does have some merit. This was well summarized by Wallenbock and Potsch,131 who stated that resection is recommended “as long as there are no better long-term results of prosthetic substitution of the radial head.” We hope that prosthetic substitution will prove valuable and effective. However, realistically the long-term follow-up data of those treated by resection certainly justify consideration of this as a treatment option, particularly in those that do not have an associated injury.
OPEN REDUCTION AND INTERNAL FIXATION
Surgical treatment of displaced radial head fractures has evolved from excision of fracture fragments or the entire head of the radius, to several techniques of ORIF and modern types of radial head replacement. ORIF was used sporadically in the past, largely because of the perception that it had “not proved successful in anyone’s hands.”98 The poor earlier results were probably due to an inadequate understanding of anatomy and less refined techniques for effective internal fixation.
The fracture fragment frequently has a periosteal hinge, indicating that its viability is possible.48 The ideal fracture for fixation is a simple, large (constituting 30% of the head) fragment that involves the anterolateral margin of the head (Fig. 24-17). However, despite the bigger technical challenge of fixing smaller fragments, biomechanical studies have also shown a benefit of fixation of fragments smaller than one third of the radial head.8,9 The anterolateral margin of the head does not articulate with the lesser sigmoid notch; instrumented fixation of this fragment does not result in impingement (Fig. 24-18).20,113 If there are multiple but large fragments, open reduction can still be performed,48 but results can be disappointing.69,103
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree