Chapter 30 Secondary, Spontaneous, and Postarthroscopy Osteonecrosis of the Knee
Diagnosis and Management
First described in 1968 by Ahlback and colleagues,3 spontaneous osteonecrosis of the knee has been recognized as a distinct clinical entity, with the potential to cause significant morbidity.39,63 In contrast to cases of secondary osteonecrosis, spontaneous osteonecrosis of the knee tends to affect a different patient population with a different pattern of bony involvement. More recently, osteonecrosis of the knee following arthroscopic surgery has been described, most commonly following arthroscopic meniscectomy. Initially reported by Brahme and associates14 in 1991, postarthroscopic osteonecrosis has also been noted to occur subsequent to anterior cruciate ligament reconstruction and chondroplasty procedures.10,24,58
Spontaneous Osteonecrosis of the Knee
SPONK is a disorder of uncertain cause, classically described as a focal lesion occurring in the medial femoral condyle of a patient in the fifth or sixth decade of life, with women affected almost three to five times as commonly as men.3,8,34,39,63,70 Typically, patients present with the sudden onset of severe pain, localizing to the medial aspect of the knee just proximal to the joint line. Although a traumatic cause has been implicated in SPONK, only a minority of patients recall a specific injury that precipitated their symptoms. In the acute phase of the disease, patients will often report pain with weight-bearing activities and an increase in the severity of their pain at night. Depending on the stage of the lesion and its size, this acute-phase pain will either gradually resolve or become chronically debilitating.
Clinical Evaluation
Examination of the affected knee in the acute phase of SPONK, typically the first 6 to 8 weeks following symptom onset, will demonstrate a small to moderate effusion with limitation of range of motion secondary to pain and associated muscle spasm. Palpation will often elicit a localized area of tenderness over the medial femoral condyle, just proximal to the joint line in the flexed knee. Although the medial femoral condyle is most commonly affected in spontaneous osteonecrosis of the knee, lesions involving the medial tibial plateau, the lateral femoral condyle and, rarely, the patella have also been reported in the orthopedic literature.* Identifying the area of maximal tenderness to palpation can serve as a guide to localizing the involved area. Ligamentous examination of the affected knee is typically normal in cases of SPONK.
Causes
Similar to the proposed mechanisms associated with osteonecrosis of the femoral head, two main causes have been suggested in the pathogenesis of SPONK, traumatic and vascular. With most affected patients being older women with osteoporotic bone, some believe that SPONK develops as a consequence of microfractures occurring in weak subchondral bone secondary to minor trauma.40 It has been suggested that following an episode of trauma to the knee, fluid enters the intercondylar region, filling the potential space created by the subchondral microfractures in the femoral condyle.9,33,70 This fluid increases the intraosseous pressure in the area, leading to focal osseous ischemia and eventual necrosis. Researchers have questioned this theory as the mechanism of SPONK. Mears43 performed histopathologic evaluation of specimens taken from 24 patients diagnosed with SPONK and found that only 1 patient had evidence of bone necrosis. Of the specimens in this study, 75% had demonstrable osteoporosis, implying that osteonecrosis is more of a secondary phenomenon following insufficiency fracture, rather than the primary mechanism of the disease. Others have supported the insufficiency stress fracture theory as the cause of SPONK, believing that when bony necrosis develops, it occurs as a consequence of physiologic resorption and remodeling following fracture.34,55,67
Where a vascular cause continues to be the dominant theory for osteonecrosis of the femoral head, with up to 75% of affected patients showing evidence of an underlying thrombophilia or coagulopathy, these predisposing factors have yet to be consistently demonstrated in patients with SPONK.32,39 In the hip, many believe that the presence of a coagulation disorder, including resistance of activated protein C, low tissue plasminogen activator activity, and hypofibrinolysis, causes intraosseous venous occlusion that culminates in the hypoxic death of bone. Evaluation of the coagulation profiles of patients affected with SPONK is necessary to determine whether this mechanism is present in the pathogenesis of the disease.
The presence of a medial meniscal tear has been proposed as a potential third cause behind the development of SPONK.52,56 Case series have identified medial meniscal tears in 50% to 78% of patients of patients with SPONK, with a recent series by Robertson and colleagues65 noting that tears, specifically in the area of the meniscal root, coexisted with spontaneous osteonecrosis in 24 of their 30 patients (80%). They theorized that in older patients with osteoporotic bone, discontinuity of the medial meniscus results in loss of hoop stress distribution in the medial compartment, increasing the load experienced in the femoral condyle and potentially predisposing patients to the development of subchondral insufficiency fracture.
Radiographic Evaluation and Staging
Cases of suspected SPONK should be initially evaluated with a plain, weight-bearing x-ray series of the knee, including an anteroposterior, 45-degree flexion posteroanterior, lateral, and skyline or Merchant views. Early in the disease process, plain x-rays may fail to identify any abnormalities, despite the presence of significant symptomatology. As the condition progresses, plain film findings may include a radiolucent lesion with a surrounding sclerotic halo in addition to subtle flattening of the involved femoral condyle (Fig. 30-1). In advanced cases, with significant subchondral collapse, secondary degenerative changes may be evident with loss of joint space, sclerosis in the medial tibial plateau, and osteophyte formation (Fig. 30-2).
Several staging systems have been described for SPONK based on plain x-ray appearance.2,39,63,70 In the four-tiered system described by Koshino,36 stage I disease is defined as incipient, with patients reporting pain with activity; however, plain x-rays are negative for pathology. In stage II SPONK, or the avascular stage, a round to oval subchondral lucency in the weight-bearing area is present with associated increased density in the surrounding femoral condyle. Subchondral collapse heralds stage III SPONK. During the collapse or developed stage of disease (stage III), x-rays demonstrate a sclerotic halo bordering the radiolucent lesion. Further subchondral collapse with associated development of arthritic changes in the affected compartment define stage IV disease.
Aglietti and coworkers2 have modified the Koshino staging system to include five stages of disease. In stage I, the x-rays are normal in appearance.39 Subtle flattening of the affected femoral condyle characterizes stage II SPONK, which indicates the potential for subsequent collapse. Stage III describes the characteristic radiolucent lesion with a circumferential sclerotic border, and stage IV disease is heralded by an increase in the size of the sclerotic halo as the subchondral bone begins to collapse. Stage V SPONK includes continued subchondral collapse, with the development of associated secondary degenerative changes.
Prognostic implications can be made based on the plain x-ray appearance of the lesion, primarily based on its size. The width of the lesion can be measured on the anteroposterior view, with those measuring less than 1 cm classified as small and those more than 1 cm classified as large.3,50,70 In many of the early studies of SPONK, the area of the lesion within the condyle was used to predict which cases would progress to severe degenerative arthritis.40,51 Cases in which the lesion was less than 2.5 cm2 were unlikely to progress, whereas those with an area more than 5 cm2 were considered to have a poor prognosis. Another useful plain x-ray measure is the ratio of the width of the lesion compared with the overall width of the femoral condyle on the anteroposterior view.2,7 This measure is not affected by differences in magnification of the view and has been shown to correlate with prognosis. Studies have demonstrated that good outcomes were common in lesions with a size ratio less than 0.45 whereas those with a ratio more than 0.5 typically progress to severe degenerative arthritis.39
In both the hip and knee, magnetic resonance imaging (MRI) has become the standard imaging modality for the detection of osteonecrosis. MRI is both sensitive and specific for the evaluation of SPONK, often demonstrating more extensive involvement than was evident on plain radiography.* T1-weighted imaging in cases of spontaneous osteonecrosis of the knee shows a discrete low-signal area, often surrounded by an area of intermediate signal intensity. A serpiginous low signal line is often present at the margin of the lesion, delineating the necrotic area from the adjacent area of bone marrow edema. T2-weighted images will typically show a high signal intensity at lesion edge, in the region of the bone marrow edema. Some have suggested using gadolinium-enhanced MRI for the evaluation of cases of SPONK. The addition of gadolinium is believed to provide information on the extent of osseous activity and turnover at the edges of the lesion, with enhanced adjacent activity believed to be a positive prognostic sign indicative of healing potential.
Clinical Course
The course and prognosis of patients with spontaneous osteonecrosis of the knee are dependent on the size and stage of the lesion. Most patients present with a similar history and physical examination. Pain is often severe at symptom onset, and is present with weight bearing, with a typical increase in severity at night, and has a significant impact on the patient’s daily activities. The intense pain associated with the acute phase of SPONK may last up to 6 weeks, at which point the extent of the patient’s symptoms divides them into two main groups.39 Those who will have with a satisfactory outcome will typically report improvement in their pain and intermittent swelling after the 6-week time point, although mild symptoms with activity may continue for up to 12 to 18 months. These patients most commonly have smaller lesions evident on imaging studies, with lesions usually less than 40% of the width of the involved femoral condyle. Despite significant improvement in their symptoms and the ability to resume normal daily activities, the vast majority of patients with SPONK will eventually develop osteoarthritic changes in the involved compartment. Insall29 has reported that at 2-year follow-up, almost all patients with osteonecrosis of the knee have evidence of at least grade I osteoarthritis, with joint space narrowing. Patients whose symptoms fail to improve after 6 weeks tend to follow a more relentless and progressive disease course. They are more typically those with large lesions encompassing more than 50% of the width of their femoral condyle. These patients, in the poor prognosis group, often never report improvement in their knee function or extent of pain. Serial imaging will often demonstrate a rapid progression with collapse and the subsequent development of degenerative changes in the affected compartment.
Postarthroscopy Osteonecrosis of the Knee
First reported by Brahme and associates14 in a series of seven patients who developed radiographic evidence of osteonecrosis following the arthroscopic treatment of meniscal pathology, ONPK has been recognized as a rare potential complication of arthroscopic surgery.58,70 Many early case reports describing this entity found it subsequent to arthroscopic meniscectomy, leading it to be referred to as postmeniscectomy osteonecrosis of the knee. However, more recently, osteonecrosis lesions have been noted to occur following other arthroscopic procedures, including chondroplasty and anterior cruciate ligament reconstruction.10,24,31
Considering the large number of arthroscopic procedures performed annually and the relatively few reports of cases of postarthroscopy osteonecrosis, the prevalence of ONPK is very low.31 At present, ONPK following arthroscopic meniscectomy has been described in nine clinical studies, including a total of 47 patients.58 In all 47 cases, postoperative MRI demonstrated evidence of osteonecrosis that was not present in preoperative imaging studies. In contrast to the patient population typically affected by SPONK, ONPK tends to affect slightly younger patients (mean, 58 years; range, 21 to 82 years), with an equal gender distribution (23 women and 24 men).70
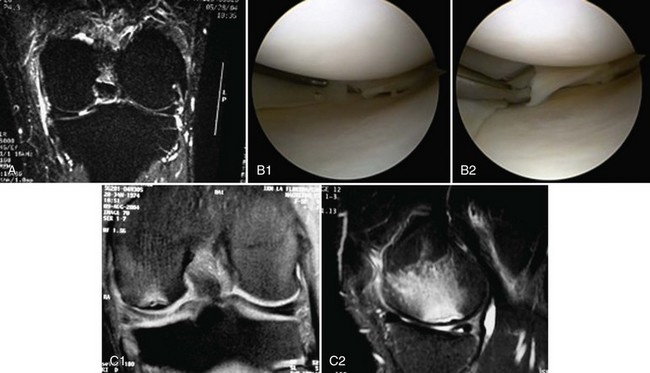
In these 47 patients, lesions of ONPK predominantly affects the medial femoral condyle (39 [82%]), followed by the lateral femoral condyle (4), lateral tibial plateau (2), and medial tibial plateau (1). In each of the reported cases, osteonecrosis developed in the geographic location of the patient’s pathology and arthroscopic procedure, with none arising in the contralateral compartment postoperatively (Fig. 30-3). Concomitant chondral lesions in the region of the meniscal tear were reported to exist in 65% of patients who went on to ONPK, with chondromalacia of the medial compartment noted to exist in 33 of these 47 published cases.
In patients who develop osteonecrosis of the knee following arthroscopic surgery, symptoms of pain, swelling, and limited range of motion may persist or even worsen postoperatively, despite the fact that an adequate resection of their meniscal tear was performed.24,31,53,58 Cases of persistent or worsening symptoms after knee arthroscopy need to be considered for the possibility of an evolving osteonecrosis lesion, a diagnosis that needs to be distinguished from SPONK, bone marrow edema syndrome, and recurrent meniscal tear.
Cause
At present, the exact cause of ONPK has yet to be fully elucidated. Similar to the previously described correlation of meniscal tears with the development of spontaneous osteonecrosis of the knee, some believe that altered knee biomechanics following meniscectomy is responsible for the pathogenesis of the disease.53,58,68 Previous studies have shown that approximately 50% of joint compressive forces are transmitted through the meniscus in extension and up to 85% of the load in 90 degrees of knee flexion.4 Partial meniscectomy increases tibiofemoral contact pressures in the treated compartment, potentially leading to subchondral insufficiency fractures from altered load transmission. Histopathologic evaluation of specimens from cases of ONPK have supported this theory, demonstrating evidence of subchondral insufficiency fractures, with bony necrosis present distal to the fracture site.67 A corollary to the insufficiency fracture theory of ONPK is the possibility that overly aggressive postoperative rehabilitation contributes to the development of this condition. In an attempt to restore function, rapid resumption of weight-bearing activities and exercise are often started within days of the operative procedure. It is possible that if aggressive therapy is resumed prior to bony remodeling in response to the altered load distribution that occurs postmeniscectomy, insufficiency fractures may develop.
Others have hypothesized that the pathologic articular cartilage in the affected compartment has increased permeability to arthroscopic fluid.58,62 This increase in fluid permeability may also occur following the instrumentation of the articular surface, during shaving chondroplasty, or with inadvertent contact of arthroscopic instruments with the femoral condyle during meniscectomy. Influx of arthroscopy fluid may cause subchondral edema and subsequent osteonecrosis from increased intraosseous pressure. Localized osteoarticular injury from the use of a laser or radiofrequency probe during the arthroscopic procedure has been described as a third potential cause of ONPK.23,27,37,70 It has been proposed that direct thermal injury or injury from photoacoustic shock from these instruments induces an inflammatory response, leading to bony edema, increased local intraosseous pressure, and eventual osteonecrosis.
Radiographic Evaluation and Staging
In the early stages of osteonecrosis in the postoperative knee, because the disease is primarily one of the bone marrow, plain x-rays are of limited value in the initial workup. Although the bone scan will often be positive in cases of ONPK, with a high level of sensitivity for changes in local osseous vascularity, its specificity and spatial resolution are poor. The diagnosis of osteonecrosis in the postoperative knee is dependent on an MRI of the affected joint, with two specific criteria that need to be filled, the absence of osteonecrosis on preoperative MRI performed 4 to 6 weeks after the onset of symptoms and a time association between the arthroscopic procedure and the development of a suspicious bone marrow edema pattern on postoperative MRI scans.31,52,58,59
To distinguish cases of ONPK from those of SPONK, the preoperative MRI must be normal with respect to the condition of the bone and bone marrow of the femoral condyle and tibial plateau. However, it is important to acknowledge that in the very early stages of spontaneous osteonecrosis of the knee, MRI of the affected knee may be devoid of findings; this is described as the window period of SPONK, between symptom onset and MRI evidence of signal changes. Most authors have reported using a period of 4 to 6 weeks following the development of symptoms as sufficient time for radiographic evidence of SPONK to be present.31,58 This is largely based on an animal study by Nakamura and coworkers54 in which MRI changes developed in all specimens by 4 weeks following surgically induced femoral head osteonecrosis. Distinction between SPONK and ONPK may not be possible with imaging studies performed prior to this 4- to 6-week time point.
A temporal association between the arthroscopic procedure and postoperative MRI signal changes must be present for the diagnosis of ONPK to be made. In the nine clinical studies reporting cases of osteonecrosis in the postoperative knee, the mean time between arthroscopy and MRI establishing the diagnosis of ONPK was 18 weeks (range, 3 to 176 weeks).58 This criterion is more difficult to assess and qualify, because bone marrow edema commonly occurs following arthroscopic knee procedures. In a study of 93 patients with a mean age of 36.6 years undergoing arthroscopic meniscectomy, Kobayashi and colleagues35 found that 34% had MRI evidence of bone marrow edema in the operative compartment within 8 months of their procedure. Although it may be related to the age of the patients in this study, none progressed to ONPK.
MRI performed in the early stages of ONPK will demonstrate a nonspecific large area of bone marrow edema in the femoral condyle, ipsilateral to the prior meniscectomy, with heterogenous signal present on T2 imaging. By 3 months postoperatively, the extent of edema typically decreases and MRI findings in cases of ONPK are similar to those seen in cases of SPONK, with T1 imaging showing a discrete low-signal area surrounded by an area of intermediate signal intensity. A line of low signal is often present at the margin of the lesion, delineating the necrotic area from the adjacent area of bone marrow edema. T2 images will typically show a high signal intensity at the lesion edge, in the region of the bone marrow edema. As the lesion progresses to its final stages, bone sequestration may be present, with a surrounding high signal rim, along with condylar flattening and the possibility of loose body development.6,58
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree