Scapula Fractures: Open Reduction Internal Fixation
Peter A. Cole
Babar Shafiq
INTRODUCTION
Scapula fractures are uncommon injuries. A recent epidemiological study from Edinburgh showed that only 52 of 6,986 (0.7%) fractures seen at their fracture clinic involved the scapula (1). It is estimated that scapula fractures account for only 3% to 5% of all fractures about the shoulder girdle, with most occurring in the clavicle or proximal humerus (2, 3, 4 and 5). The robust muscular envelope, the mobility of the scapula on the thoracic cage, its oblique orientation to the chest wall, and the surrounding bones, which are more vulnerable to fracture, protect the scapula making fracture of this bone infrequent.
In the past 25 years, several studies have documented poor results following nonoperative management of displaced scapular fractures (6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17 and 18). With the development of modern techniques in internal fixation, surgeons began repairing selected scapula fractures utilizing the AO principles of restoration of articular reduction, alignment, and stable internal fixation leading to a renewed interest in the operative management of both displaced intra-articular and extra-articular scapular fractures (6,10, 11, 12, 13, 14, 15, 16, 17 and 18). The surgical treatment of these fractures continues to evolve as our knowledge of shoulder anatomy, surgical approaches, and implants has improved.
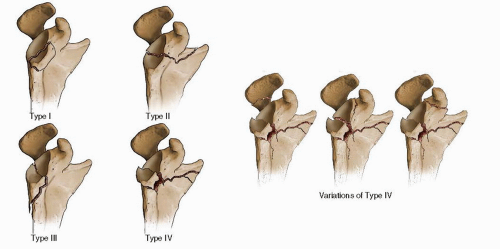
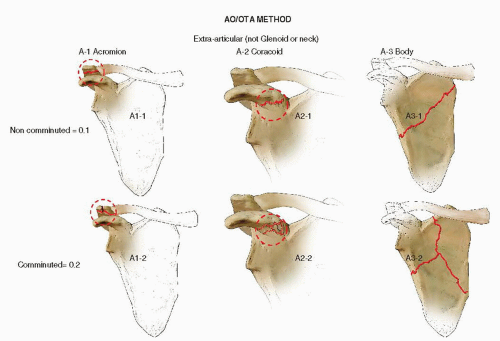
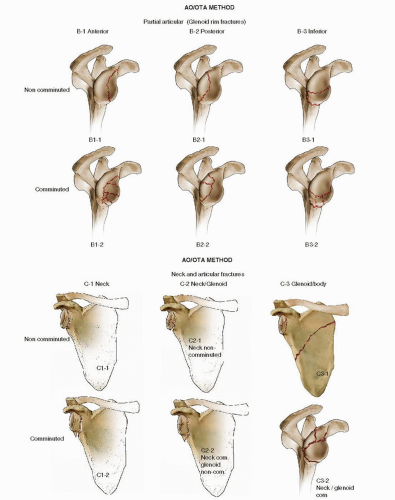
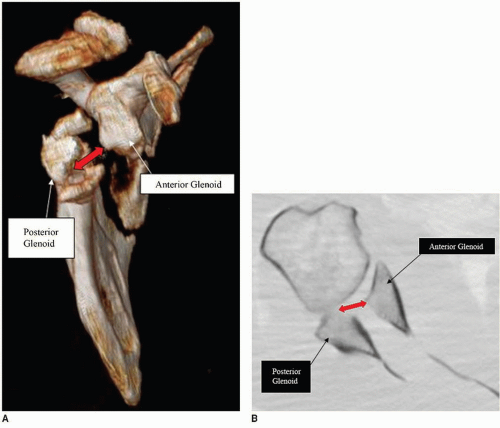
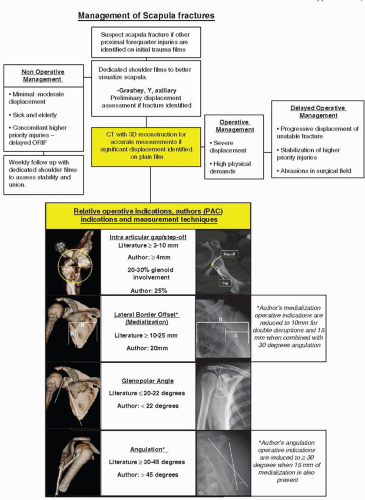
There is no universally accepted classification for scapula fractures. In 1984, Hardegger et al. (7) published a series of 37 operatively treated scapula fractures and introduced a classification scheme that bears his name. Additionally, Ada and Miller (19) proposed a comprehensive classification that was anatomically defined. Mayo et al. (20) modified Ideberg’s classification for intra-articular fractures (21,22), based on radiographs and operative findings of 27 intra-articular glenoid fractures. This classification is also helpful in directing surgical decision making, as it takes into account associated scapular body and process fractures, which frequently occur in association with glenoid fractures (Fig. 2.1). The Orthopaedic Trauma Association (OTA) classification system is an alphanumeric system that classifies both intra- and extra-articular fractures (Fig. 2.2). Its main weakness is that it does not correlate fracture patterns or combinations of injuries with real fractures. Scapula fractures have also been mapped from 3D reconstructions to better illustrate the true nature of fracture patterns and could serve as a basis for a comprehensive classification scheme (Fig. 2.3). The main value of three dimensional mapping, however, is to serve as a useful roadmap for surgical planning and a greater understanding of the muscular force vectors acting on the scapula (16).
INDICATIONS AND CONTRAINDICATIONS
Open reduction and internal fixation of intra-articular glenoid fractures is indicated when there is more than 4 mm of articular step-off and more than 20% of the glenoid is involved (2,7,20,21,23, 24 and 25). However, the literature varies considerably with other authors advocating surgery for articular step-off ranging from 2 to 10 mm (20,25, 26, 27 and 28). The decision for surgery as well as the amount or degree of articular step-off, gap, and percentage of joint involvement should be correlated with the patient’s job, age, activity level, physiologic status, and hand dominance (Fig. 2.4A,B).
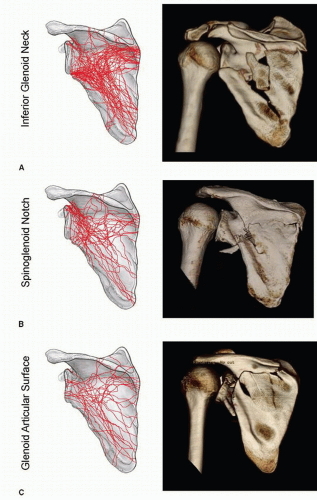 FIGURE 2.3 This illustration shows maps of fractures about the glenoid with three common anatomical zones of involvement in scapular fractures that required surgical treatment. These include (A) the lateral border just inferior to the glenoid, (B) the spinoglenoid notch between the base of the acromion and the superior aspect of the glenoid fossa, and (C) the glenoid cavity with the fracture tracking medially into the body of the scapula. (From Armitage BM, Wijdicks CA, Tarkin IS, et al. Mapping of scapular fractures with three-dimensional computed tomography. J Bone Joint Surg Am 2009;91(9):2222-2228 [Fig 4] with permission.) |
The surgical indications for displaced extra-articular scapula fractures are controversial because there are no randomized controlled studies comparing operative versus nonoperative treatment. Relative indications for internal fixation of extra-articular scapular fractures include the following:
Lateral border offset (sometimes referred to as medialization) >20 mm on an anteroposterior (AP; Grashey) view x-ray of the shoulder (Fig. 2.5A,B)
Angular deformity >45 degrees as seen on a scapular Y radiograph of the shoulder (Fig. 2.6A,B)
Lateral border offset >15 mm plus angular deformity >30 degrees
Glenopolar angle (GPA) <22 degrees as measured on a true AP Grashey view radiograph of the shoulder (Fig. 2.7A,B)
Displaced double lesions of the superior shoulder suspensory complex (SSSC)
Both the clavicle and scapula fractures are displaced >10 mm (Fig. 2.8A,B)
Complete acromioclavicular dislocation and scapula fracture displaced >10 mm
We also advocate operative management of displaced scapular fractures in patients with complex ipsilateral upper extremity injuries particularly in younger highly active patients, when two or more of the above criteria are met (Fig. 2.9).
Contraindications to scapula surgery include extra-articular scapular fractures that are displaced <15 mm and angulated <25 degrees because the outcomes of nonoperative treatment for even moderately displaced scapula fractures are uniformly good (3 and 4,8,29, 30, 31 and 32). Active mobility of the elbow and wrist is encouraged immediately, but a sling and rest are indicated for 10 to 14 days. Scapula fractures heal rapidly due to the rich blood supply in the shoulder girdle. Active range of motion can be started by 4 weeks and advanced quickly. Resistive exercises are begun by 8 weeks and restrictions lifted as symptoms allow by 12 weeks.
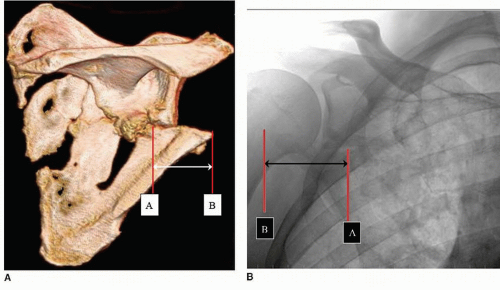 FIGURE 2.5 A, B: 3D-CT (P/A view) and True A/P (Grashey) radiograph of left shoulder demonstrating Lateral Border Offset (sometimes referred to as medialization). Note that the displacement is measured from “A” the anatomic location of the lateral border (inferior and medial to the glenoid) to the tip of the displaced distal fragment “B.” (Anavian J, Conflitti JM, Khanna G, et al. A Reliable Radiographic Measurement Technique for Extra-articular Scapular Fractures. Clin Orthop Relat Res 2011;469(12):3371-3378, with permission.) |
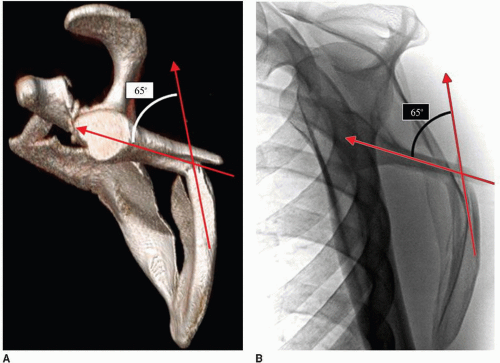 FIGURE 2.6 A, B: Scapular “Y” radiograph and 3D-CT rotated to “Y” view demonstrating angular deformity. (Anavian J, Conflitti JM, Khanna G, et al. A Reliable Radiographic Measurement Technique for Extra-articular Scapular Fractures. Clin Orthop Relat Res 2011;469(12):3371-3378, with permission.) |
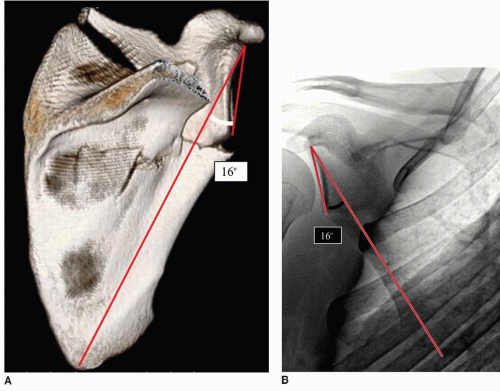 FIGURE 2.7 A, B: 3D-CT (P/A view with acromion subtracted) and True A/P (Grashey) radiograph of right shoulder demonstrating GPA. On the Grashey view, measured from inferior glenoid rim to superior glenoid rim to most distal point of scapula inferior angle. (Anavian J, Conflitti JM, Khanna G, et al. A Reliable Radiographic Measurement Technique for Extra-articular Scapular Fractures. Clin Orthop Relat Res 2011;469(12):3371-3378, with permission.) |
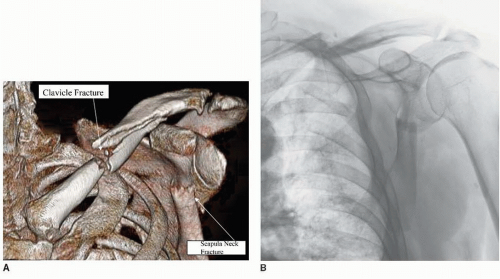 FIGURE 2.8 A, B: 3D-CT and AP shoulder demonstrate double lesion to the SSSC (clavicle fracture and scapula neck fracture). |
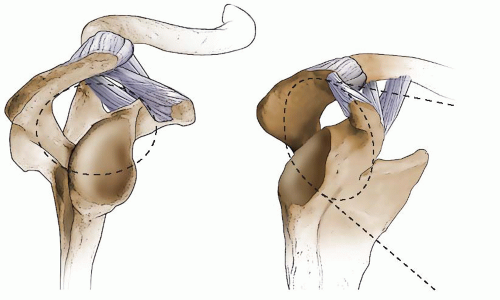 FIGURE 2.10 This illustration depicts the SSSC, which is an osseoligamentous ring made up of the structures along the dotted line. Goss theorized that if two structures in the ring were disrupted, then a “floating shoulder” lesion would be present, implying that there would be no osseous or ligamentous continuity between the axial skeleton and the forequarter. Figure 2.8 shows 3D-CT and AP radiographs of this lesion. |
The term superior shoulder suspensory complex is the osseoligamentous relationship between the three scapula processes, described by Goss in 1993 (33). Goss theorized that if there were two disruptions in this “ring,” made up by the acromion, coracoid, and glenoid, as well as their capsule-ligamentous connections, then the glenohumeral joint would be “floating,” a condition that describes discontinuity between the axial and appendicular skeleton (Fig. 2.10). Though this theory has been challenged by some authors (34, 35 and 36), Goss recommended surgery if two such disruptions occur simultaneously. We agree with Edwards et al. (34) and Ramos et al. (36) that surgery is not indicated when each component of the double displacement is stable and minimally displaced.
Isolated fractures of the acromion or coracoid process are uncommon. Fractures of the acromion process or spine usually occur as a result of a direct blow to the superior shoulder region, whereas coracoid process fractures result from violent traction injuries through the biceps and coracobrachialis. While indications for operative management of these fractures have not been established, we use several criteria to aid in determining the need for surgery. If either an acromion or coracoid fracture is displaced more that 10 mm, or there is an ipsilateral scapula fracture or multiple disruption of the SSSC, then open reduction and internal fixation is warranted (19,37, 38, 39, 40 and 41). When the acromion is displaced more than 5 mm, a supraspinatus outlet view should be obtained and evaluated for acromial depression, which may contribute to an impingement syndrome, much like a type III “hooked” acromion, and occasionally warrant internal fixation.
Outcomes following acromion and coracoid process fixation are good with high rates of union (13,40 and 41). Anavian et al. reported the results of operative management of 14 coracoid and 13 acromion fractures treated operatively. Most were treated with interfragmentary screw fixation and in selective cases with suture fixation. Supplemental mini or small fragment plate fixation was used for coracoid fractures that extended into the glenoid fossa or acromial spine. Similarly, 2.4- or 2.7-mm reconstruction plates were used when fixation of acromion fractures extending into the scapular neck or base. Distal acromion fractures were treated with a tension band or a mini fragment locking plate on the superior surface or along the anterior or posterior acromial edge. Postoperatively, patients were treated with passive- and active-assisted range of motion for the first month, progressing to resistance exercises after 2 months and full, unrestricted activity by 3 months. All patients were pain free at rest and with upper extremity activities at the time of final follow-up (mean 11 months, range 2 to 42 months). Mean DASH score for those patients with functional assessments was 7 (0 to 26), better than that of the uninjured population normative baseline DASH score 10. The only complications in this series were soft-tissue irritation requiring hardware removal in two patients and removal of ectopic bone in one patient (14).
PREOPERATIVE PLANNING
History
Fractures of the scapula occur as the result of blunt trauma with strong of forces applied to the shoulder. Partial articular fractures, usually involving the anterior glenoid, are commonly associated with anterior shoulder dislocations. These fractures are often referred to as bony Bankart lesions (42) and may be characterized by anterior shoulder instability. If shoulder instability is present with subluxation of the humeral head on radiographic examination, or clinical examination, then operative intervention, given an appropriate surgical candidate, is recommended. Surgery is usually necessary when there is involvement of more than 20% of the articular surface.
A second type of scapula fracture involves the glenoid neck and body with or without articular involvement, and this pattern most commonly occurs following high-energy trauma. Associated injuries occur in up to 90% of patients in this group, and a thorough physical examination is necessary to avoid overlooking serious concomitant injuries (2,21,37). In the seriously injured patient, scapular fractures are often overlooked leading to delays in treatment. It is a common misconception that scapulothoracic dissociation occurs following high-energy blunt trauma, but this is not the case as this devastating injury results from a violent traction force to the upper extremity.
Physical Examination
The physical examination must be thorough and complete as associated injuries are common particularly to the spine, cranium, and thorax. When possible, the shoulder and upper extremity should be examined with the patient sitting or standing to give good access to the posterior forequarter, which is difficult when the patient is supine in bed or on a gurney. Medial and caudal displacement of the shoulder may be obvious producing marked asymmetry, particularly if the patient is upright. Medialization may or may not be apparent on the initial radiographic studies, but once the patient is upright and attempts to move the extremity, the shoulder medializes as the scapula rotates forward over the thorax. In some patients with scapula and multiple rib fractures, the chest wall fails to support the scapula and contributes to deformity (Fig. 2.11). Patients with highly displaced scapula fractures, particularly when associated with multiple ribs or a clavicle fracture, are unable to forward elevate or externally rotate their shoulders, even a few weeks after injury.
Skin integrity should be assessed as abrasions are common after the typical mechanism of a direct blow to the shoulder. If surgery is indicated, it should be delayed until there is skin re-epithelialization around 7 to 14 days, after injury (Fig. 2.12). Ipsilateral, concomitant, neurovascular injuries are common and require a very careful assessment of the brachial plexus and peripheral pulses. Brachial plexus injury occurs in over 10% of patients with scapula fractures (5,30). Axillary nerve sensation should be documented; however, motor function to the deltoid is frequently impossible to determine with displaced fractures. The suprascapular nerve is vulnerable and commonly
injured in association with fractures that extend into the spinoglenoid notch at the base of the acromion, so-called true scapula neck variants (18) (Fig. 2.13A). Based upon a review of 96 surgically treated scapula fractures, the senior author identified 14 cases of suprascapular nerve injury almost exclusively associated with these fracture patterns. Consequently, we recommend electrodiagnostic studies (electromyography and nerve conduction studies— EMG/NCS) be performed in patients with fractures involving the suprascapular and/or spinoglenoid notch. These studies are of little diagnostic value immediately after injury and should be performed at least 2 weeks after injury
when fibrillations and positive sharp waves may be present indicating denervation (axonotmesis and neurotmesis) (43,44). Every effort should be made to identify injury early and before surgical intervention, when possible (45).
injured in association with fractures that extend into the spinoglenoid notch at the base of the acromion, so-called true scapula neck variants (18) (Fig. 2.13A). Based upon a review of 96 surgically treated scapula fractures, the senior author identified 14 cases of suprascapular nerve injury almost exclusively associated with these fracture patterns. Consequently, we recommend electrodiagnostic studies (electromyography and nerve conduction studies— EMG/NCS) be performed in patients with fractures involving the suprascapular and/or spinoglenoid notch. These studies are of little diagnostic value immediately after injury and should be performed at least 2 weeks after injury
when fibrillations and positive sharp waves may be present indicating denervation (axonotmesis and neurotmesis) (43,44). Every effort should be made to identify injury early and before surgical intervention, when possible (45).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree