Soft-Tissue Coverage: Gastrocnemius and Soleus Rotational Muscle Flaps
Randy Sherman
Wai-Yee Li
INTRODUCTION
Orthopedic trauma management continues to evolve into a technologically driven science as implants for fracture fixation continue to improve. Less invasive surgical approaches for fracture reduction and fixation, 2D and 3D imaging, and earlier and more aggressive rehabilitation continue to improve patient outcomes. However, in a small but significant subset of orthopedic trauma patients, uncomplicated fracture healing can be seriously compromised by complex soft-tissue injuries. Failure of the orthopedic surgeon to appreciate or underestimate the magnitude of the soft-tissue injury may further complicate treatment. High-energy injuries are still associated with a relatively high incidence of delayed union, nonunion, fixation failure, and infection. Early and repeated débridement of open fractures and the surrounding soft tissues is one of the basic pillars of fracture management. Unfortunately, many surgeons attempt to close small- and medium-sized wounds primarily leading to wound breakdown or dehiscence. Early introduction of noninjured, well-vascularized soft tissue is a thoroughly researched, well-documented alternative to maximize wound healing and minimize infectious complications after fracture fixation. This chapter describes the use of the gastrocnemius and soleus rotational muscle flap for coverage of soft-tissue defects in the lower leg.
INDICATIONS AND CONTRAINDICATIONS
A muscle, myocutaneous or fasciocutaneous flap, is indicated when vital structures such as bones, joints, tendons, or hardware remain exposed after injury. Overlying skin and soft tissue that might initially appear viable following injury can be further compromised after additional surgical exposure. Wounds that are closed under tension may result in further ischemia to the skin. The treatment algorithm for soft-tissue reconstruction after a tibial fracture traditionally divides the lower leg into proximal, middle, and distal thirds. For many wounds and defects in the proximal third of the lower leg, a medial or lateral gastrocnemius flap is an excellent option. In the middle third of the leg, small and medium-sized wounds can often be covered by a soleus rotational muscle flap. With large defects in the distal one-third of the leg, ankle, and foot, a free tissue transfer is usually necessary.
When considering soft-tissue reconstruction following lower limb trauma, the ideal muscle flap should be well vascularized, durable, easily harvested, and capable of a broad range of coverage options. Fortunately, of all of the local rotational muscle flaps described, the gastrocnemius is one of the most reliable and is well
situated to aid in the coverage of many proximal third defects. The gastrocnemius is a broad, two-headed muscle with a single proximal vascular pedicle for each segment, the medial and lateral sural arteries, which either take rise directly from the popliteal artery just above the articular line or result as a bifurcation of a single, more proximal sural vessel. Each artery acts as the sole vascular supply for its muscle segment allowing for maximum utilization of the flap in its elevation and arc of rotation. Consequently, the gastrocnemius muscle or a myocutaneous rotational flap is the procedure of choice for soft-tissue coverage of complex open wounds about the knee and proximal third of the tibia and fibula. The use of this flap is indicated in the following circumstances: (a) coverage of acute, proximal third, grade III, open tibial fractures with or without hardware involving exposure of the knee joint, capsule, fracture site, or cortex (Fig. 46.1); (b) obliteration of dead space and wound closure after radical débridement of osteomyelitic wounds or infected nonunions in this region (Fig. 46.2); (c) coverage of exposed total knee arthroplasties or prearthroplasty tissue augmentation in densely scarred wound beds (Fig. 46.3); (d) limb salvage and coverage of endoprostheses or allograft material after resection of musculoskeletal neoplasms (Fig. 46.4); and (e) preservation of stump length in revision amputation surgery. The medial head of the muscle is larger and longer than the lateral head. Each can be utilized to augment or replace defined tissue defects on the ipsilateral side of the tibial surface. Anterior defects are better served by the medial gastrocnemius flap. Distal cutaneous extensions of each flap allow for greater degrees of coverage but complicates donor site closures.
situated to aid in the coverage of many proximal third defects. The gastrocnemius is a broad, two-headed muscle with a single proximal vascular pedicle for each segment, the medial and lateral sural arteries, which either take rise directly from the popliteal artery just above the articular line or result as a bifurcation of a single, more proximal sural vessel. Each artery acts as the sole vascular supply for its muscle segment allowing for maximum utilization of the flap in its elevation and arc of rotation. Consequently, the gastrocnemius muscle or a myocutaneous rotational flap is the procedure of choice for soft-tissue coverage of complex open wounds about the knee and proximal third of the tibia and fibula. The use of this flap is indicated in the following circumstances: (a) coverage of acute, proximal third, grade III, open tibial fractures with or without hardware involving exposure of the knee joint, capsule, fracture site, or cortex (Fig. 46.1); (b) obliteration of dead space and wound closure after radical débridement of osteomyelitic wounds or infected nonunions in this region (Fig. 46.2); (c) coverage of exposed total knee arthroplasties or prearthroplasty tissue augmentation in densely scarred wound beds (Fig. 46.3); (d) limb salvage and coverage of endoprostheses or allograft material after resection of musculoskeletal neoplasms (Fig. 46.4); and (e) preservation of stump length in revision amputation surgery. The medial head of the muscle is larger and longer than the lateral head. Each can be utilized to augment or replace defined tissue defects on the ipsilateral side of the tibial surface. Anterior defects are better served by the medial gastrocnemius flap. Distal cutaneous extensions of each flap allow for greater degrees of coverage but complicates donor site closures.
 FIGURE 46.1 Grade IIIB open tibial-plateau fracture with exposed knee joint after internal fixation and unsuccessful attempt at primary wound closure. |
 FIGURE 46.2 Dead space involving skin, subcutaneous tissue, muscle, and bone in a proximal-third infected nonunion. |
The soleus muscle, without a myocutaneous correlate, has a much more limited arc of rotation and is primarily used for small, medially based open wounds in the middle third of the leg. Parallel to and deep to the gastrocnemius, the soleus muscle resides in the superficial posterior compartment of the lower leg and aids in plantar flexion of the ankle and foot. It arises from the proximal tibia and fibula and inserts conjointly with the gastrocnemius to form the Achilles tendon that inserts onto the calcaneous. It has a dual blood supply from both the posterior tibial and peroneal arteries. Some authors contend that the muscle can be split longitudinally to form a medial and lateral hemisoleus flap. Indications for its use include coverage of smaller, acute open fractures, and chronic osteomyelitic wounds in the middle third of the lower leg (Fig. 46.5).
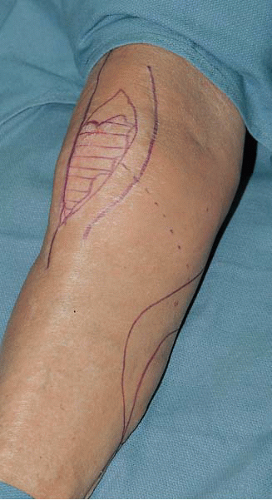 FIGURE 46.3 Scarred, atrophic, prepatella skin in an elderly patient after removal of an infected total-knee arthroplasty. |
 FIGURE 46.4 A 10-year-old girl immediately after tumor extirpation of a proximal tibial osteosarcoma and placement of endoprosthesis after loss of anterior skin. |
Contraindications to the use of the gastrocnemius flap include vascular compromise of the muscle itself by disruption of the sural arterial pedicle, compromise of the popliteal artery from which it emanates, or occlusion of the proximal arterial tree. Recipient site contraindications include a wound in the proximal third region whose size and dimensions are too large for adequate coverage by the gastrocnemius muscle. Significant local trauma to the muscle itself, although rare, prevents its successful rotation. The use of the soleus muscle for middle third lesions is limited and often requires the possible transfer of a distant muscle or fasciocutaneous flap using microvascular techniques. Similarly, injury to the substance of the soleus muscle will hinder its ability to be transposed. Vascular compromise to the soleus muscle is extremely rare because of its segmental inflow. Because of segmental minor arterial branches that exit from the posterior tibial and peroneal arteries distally, the surgeon must take great care to assure adequate vascularity to the most distal aspect of the soleus muscle when a complete transposition is planned. As with the gastrocnemius, a large anterior or laterally located wound in the middle third of the leg may not be completely covered by the soleus muscle (Fig. 46.6), and free tissue transfer may be a better option.
 FIGURE 46.5 Middle-third grade IIIB open-tibial fracture with a bony sequestrum and loss of overlying soft tissue. |
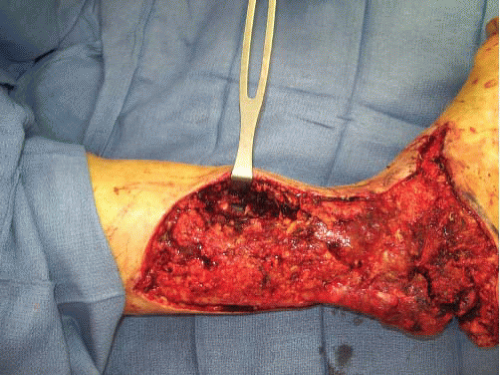 FIGURE 46.6 Large, grade IIIB, open, middle-third tibial fracture cannot be closed by a local soleus flap and requires free tissue transfer. |
Before any muscle coverage procedure, it is critical that infection or tumor recurrence has been adequately treated by débridement or excision before wound closure. No muscle flap will successfully combat ischemic, or necrotic bone, sequestrum, or loose infected hardware, which may serve as a nidus for persistent infection.
A major advancement in modern open fracture management has been the introduction, dissemination, and now wide use of vacuum-assisted dressings for wound care. The Wound VAC (vacuum assisted closure), registered trademark by KCI for Negative Pressure Wound Therapy, is a simple, elegant dressing system that includes a sterile porous sponge, a connecting tube, and a small machine capable of producing either intermittent or constant vacuum. The sponge is cut to fit the size of the recipient wound and held in place by an occlusive, adhesive transparent drape. A small aperture is cut into the drape to which the tube is easily attached. Finally, the far end of the tube is connected to the vacuum source enabled with a canister to collect effluent materials. This wound care system is designed to decrease local swelling, increase local tissue oxygenation by decreasing intracellular hydrostatic pressure, and promote granulation tissue, thereby accelerating wound contraction and closure by secondary intention. The VAC system is widely applicable and easily applied and managed. It can be used in the operating room, the wards, clinics, and at home. It is highly adaptable to various wound sizes and configurations. A constant reliable vacuum source is mandatory and is a keystone to the VAC therapy system. The dressing need only be changed every 2 to 3 days. This has radically decreased nursing labor commitments and dramatically improved patient care comfort during these very difficult perioperative periods. In the open tibial fracture patient, the VAC device is most beneficial when used to prepare a wound for eventual closure using either skin grafting or flap transfer techniques. It should not be seen as a substitute for operative débridement of untidy wounds nor for definitive wound closure procedures. Its effect on how we treat complex extremity wounds cannot be overestimated and continues to grow and adapt with extensive clinical experience.
PREOPERATIVE PLANNING
History and Physical Examination
Critical elements to the patient’s history must include the circumstances and mechanism of injury, the time since wounding and the interval treatments administered. The age and general health of the patient as well as any previous injuries, surgeries, or medical treatments should be delineated. A history of peripheral vascular disease, previous cardiac problems, deep venous thrombosis, pulmonary embolism, obesity, and/or smoking are particularly relevant in perioperative planning and management.
A thorough physical examination of the patient is crucial when planning a muscle flap procedure. Clinical inspection of the leg should be made, with particular attention paid to fracture and wound location. Most often, but not always, these are interrelated. Wound length, width, and depth as well as tissue condition (viability, crush component, maceration, foreign bodies) should be noted. Presence or absence, as well as quantification of pulse strength and location, is mandatory. A detailed vascular examination with palpation of the dorsalis pedis and posterior tibial pulses for arterial inflow, augmented by Doppler examination for venous outflow, should be performed and documented. Sensory and motor examination prior to any planned surgical procedure is critical. Other factors such as induration, discoloration, ecchymosis, and cellulitis must be considered. Any suspicion of a degloving component to the wound should be highlighted and considered when planning further surgical intervention. With acute open fractures, the surgeon should anticipate the need for subsequent soft-tissue closure. If an external fixator is utilized, the frame should allow unrestricted
transposition of the muscles from posterior to medial or anterior. The zone of injury at the fracture site may be difficult to initially categorize, and serial débridement may significantly increase the size of the wound (Fig. 46.7).
transposition of the muscles from posterior to medial or anterior. The zone of injury at the fracture site may be difficult to initially categorize, and serial débridement may significantly increase the size of the wound (Fig. 46.7).
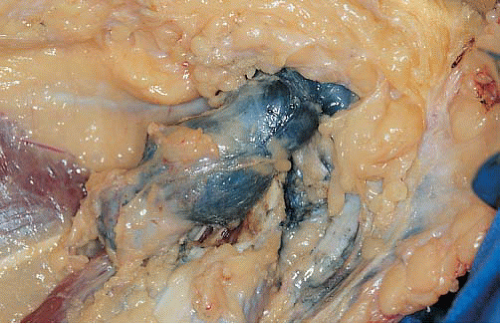 FIGURE 46.7 Large amount of retained titanium from a previously removed, infected, totalknee arthroplasty. |
The function of the posterior compartment muscles should be assessed whenever possible. Sensory examination of the foot must be evaluated, with particular attention given to the posterior tibial, sural, saphenous, and peroneal nerves both before and after each surgical intervention.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








