Intra-Articular Fractures of the Distal Humerus: Total Elbow Arthroplasty
Elaine Mau
Michael D. McKee
INTRODUCTION
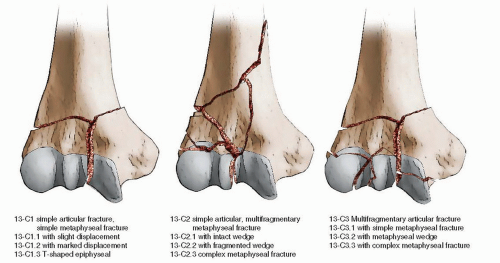
Total elbow arthroplasty (TEA) for the management of displaced and comminuted intra-articular fractures of the distal humerus in the elderly is a relatively new but attractive alternative to open reduction and internal fixation (ORIF) or nonoperative treatment in this subgroup of patients. Traditionally, displaced distal humeral fractures are treated with internal fixation; however, obtaining and maintaining the reduction through healing and rehabilitation in osteoporotic bone can be extremely challenging. These injuries typically occur in elderly patients with compromised bone stock secondary to osteoporosis following a mechanical ground level fall. Fractures of the distal end of the humerus are classified in the AO/OTA system as type 13-C fractures and involve both the articular surface and a metadiaphyseal region (Fig. 9.1).
In the past 15 years, several studies have reported the results of TEA as the primary treatment of selected distal humeral fractures, documenting favorable outcomes compared to open reduction internal fixation (1, 2, 3 and 4). At the same time, there has been renewed interest in distal humeral hemiarthroplasty as an alternative treatment method, but this has not been well described in the literature. The results of primary arthroplasty versus secondary TEA following failed fixation remain unclear. While primary arthroplasty is considered technically easier with a lower complication rate (19), Prasad and Dent (5) recently reported that secondary elbow arthroplasty following failed internal fixation had similar outcomes to primary TEA, with only a marginally higher complication rate.
INDICATIONS AND CONTRAINDICATIONS
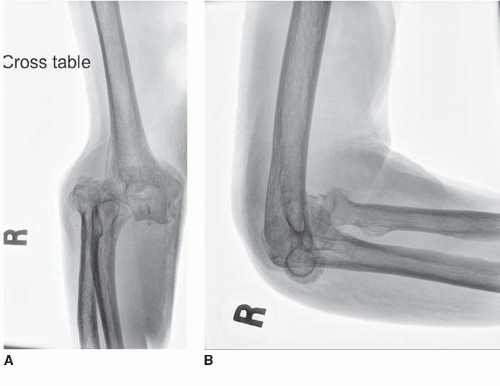
Primary TEA for distal humerus fractures is largely limited to the elderly (>70 years of age) patient population with displaced and comminuted intra-articular fractures (Fig. 9.2A,B). Within this population, other factors favoring TEA include complex articular fractures in patients with preexisting elbow arthritis (6), advanced age with reduced life expectancy, severe osteoporosis, or pathologic bone. Occasionally, younger patients (<70 years of age) with advanced and symptomatic degenerative changes in the elbow joint, with an intra-articular distal humerus fracture, may be a candidate for an elbow replacement procedure. Because older patients with simple fracture patterns do well with ORIF (7,8), age alone should not dictate the method of treatment.
Fracture extension into the diaphysis past the olecranon fossa or flare of the condyles can be treated with arthroplasty, within certain limits. For example, the Coonrad-Morrey system has a revision humeral component with a long anterior flange that is designed for bone loss of up to 8 cm from the joint surface. Fracture extension into the diaphysis should be treated with internal fixation.
There are several absolute contraindications to TEA and include flaccid paralysis of the upper extremity, severe cognitive impairment, a neuropathic joint, or the presence of an active infection. Relative contraindications to primary elbow replacement for fracture include anticipated noncompliance with activity restrictions, high-grade open fractures, soft-tissue compromise that would prevent adequate wound closure, and limbs with vascular compromise. It is important to remember that the vast majority of patients with a displaced intraarticular distal humerus fracture under the age of 70 years should be treated with ORIF.
PREOPERATIVE PLANNING
History and Physical Examination
A complete history and thorough physical examination should be performed. The history should include information on the mechanism of injury, preinjury levels of function, and medical comorbidities such as rheumatoid arthritis, diabetes, or stroke that may influence the method of treatment. In patients with high energy injuries, or in the multiply injured patient, airway management and hemodynamic stability should always take priority and should include a careful assessment of the head, chest, and abdomen prior to further treatment of the injured extremity.
On physical examination, the elbow is invariably swollen, tender, and motion is decreased. The entire upper limb must be evaluated and the soft tissues inspected for abrasions, blisters, or open wounds (typically posterior). If an open fracture is identified, intravenous antibiotics should be started. We use cefazolin for grade I or II open fractures, and an aminoglycoside is added for grade III injuries. A detailed neurovascular examination is performed including evaluation of the brachial and radial pulses, as well as the capillary refill. The function of the radial, median, and ulnar nerves should also be determined and documented as these structures are susceptible to damage, particularly, the ulnar nerve. The forearm should be carefully assessed to rule out a compartment syndrome. In the absence of neurovascular compromise or a compartment syndrome, a closed reduction with correction of any obvious angulation or deformity is performed (which decreases tension on the soft tissues) and a long-arm splint applied.
Imaging
Standard anteroposterior (AP) and lateral radiographs of the elbow are obtained. Film quality should be adequate for assessment of bone quality, fracture displacement, and the extent of intra-articular comminution. In displaced fracture patterns, traction radiographs that use ligamentotaxis to restore length and alignment can provide additional information. A CT scan of the elbow can improve the assessment of articular fragments but is best done following a preliminary closed reduction with some restoration of length and alignment (Fig. 9.3). On occasion, when the fracture pattern is unclear, a CT scan can provide detailed information about the fracture geometry, especially intra-articular comminution or associated fractures. This can help in surgical decision making
regarding the ideal procedure (i.e., TEA vs. ORIF). We have not found MRI scans to be helpful in the acute setting. Additional upper extremity radiographs should be obtained based on the history and physical examination.
regarding the ideal procedure (i.e., TEA vs. ORIF). We have not found MRI scans to be helpful in the acute setting. Additional upper extremity radiographs should be obtained based on the history and physical examination.
 FIGURE 9.3 CT scan with 3D reconstruction of the patient in Figure 9.1. Based on the imaging studies, a decision was made to treat the injury with a TEA. |
Timing of Surgery
The treatment of choice for most displaced, intra-articular distal humerus fractures is ORIF with TEA reserved for complex articular fractures in the elderly low demand patient. We believe that the best results occur when surgery is performed by experienced surgeons working with a knowledgeable operating room staff, and we rarely perform this complicated surgery at night or on the weekends. We proceed with surgical intervention as promptly as logistical preparations can be made, typically within a few days of injury. The role of primary TEA in patients with an open fracture remains highly controversial. If the patient has a minor, grade I puncture posteriorly, there is no gross contamination, and a prompt (<12 hours) thorough débridement is performed, it is probably safe to proceed with primary TEA. In the absence of any of these conditions, or if there is soft-tissue compromise, irrigation/débridement and temporary stabilization should be performed followed by elbow arthroplasty at a later date. If a decision regarding open reduction internal fixation versus elbow replacement cannot be made preoperatively with the available imaging studies, an intraoperative fluoroscopic assessment should be done, and implants for both ORIF and TEA should be available and the patient consented for either procedure. It is important to inform the operating room staff regarding the equipment required.
SURGERY
Approach
The management of the triceps muscle and tendon as well as the olecranon is crucial to achieving consistently good outcomes following TEA. We prefer to perform TEA after resection of the fractured humeral condyles using a triceps-sparing approach, which has many advantages although it is technically more difficult, and the exposure is more limited. For surgeons who do not regularly perform elbow arthroplasty, the triceps-splitting approach is most commonly used. An alternative approach is the triceps-reflecting (Bryan-Morrey) technique involving a medial-to-lateral peel of the triceps to gain adequate exposure. However, given the small but definite risk of triceps detachment with these approaches, our preferred exposure is the triceps-sparing method. The medial and lateral borders of the triceps muscle are incised, and the triceps muscle is freed from the distal humeral shaft. The medial and lateral collateral ligaments (LCLs) are elevated along with the soft tissues as a sleeve during the exposure and later reattached to the triceps at the conclusion of the case. Concomitant fractures of the proximal ulna and olecranon are relative contraindications to successful primary TEA, as they jeopardize the stability of the ulnar component (9,10). Similarly, the use of an olecranon osteotomy for exposure is contraindicated if a TEA is anticipated. Regardless of which surgical approach is chosen, there must be adequate exposure of the distal humerus to visualize the fracture, allow removal of all of the fracture fragments, and allow proper implantation of the prosthesis.
Implant Selection
In general, total elbow prostheses are available as unlinked with separate humeral, ulnar, and occasionally radial components or linked where the ulnar and humeral components are physically joined. A few models may be converted between the two depending on the requirements of the case. Among the linked systems, they are further subdivided into fully constrained and semiconstrained models. These differ in that the latter allow a small amount of varus-valgus and rotational movement, the so-called sloppy hinge, in addition to the full extension and flexion movement at the elbow joint. These semiconstrained implants have a lower loosening rate than the traditional fully constrained, with the rationale being that the looser hinge allows for some accommodation of the stresses seen at the prosthesis-cement and cement-bone interfaces, and this results in lower rates of loosening. Both the semiconstrained and constrained systems are linked, and thus, in contrast to the unlinked systems, are ideal for TEA in the fracture setting since they do not rely on intact ligaments or bony alignment to convey stability to the elbow joint.
Due to the bone loss and loss of ligament attachment that is incurred in acute fracture patterns where a TEA is indicated—namely, OTA/AO type 13 C2-C3—a linked, semiconstrained implant is typically the implant of choice. Examples of this include the Coonrad-Morrey (Zimmer, Warsaw, IN) and Discovery (Biomet Orthopaedics, Warsaw, IN) systems.
SURGICAL TECHNIQUE
Surgery is performed when logistical preparations can be made, usually in the first few days after injury. It is not necessary or desirable to perform this procedure emergently at night or on weekends without skilled staff. Either a general or regional anesthetic technique can be used. The patient is positioned on a “bean bag” in the
lateral decubitus position with the affected side up (Fig. 9.4). A tourniquet is used in all cases, nonsterile or sterile depending on the morphology of the arm. The injured extremity is supported on a padded bolster before prepping and draping. Alternatively, surgery can be performed in the supine position with the injured arm draped free on a sterile bolster across the patient’s chest. A sterile stockinette and flannel or an adherent wrap is placed on the hand. A first-generation cephalosporin is given intravenously prior to inflation of the tourniquet. Intraoperative imaging is necessary only if a decision has to be made on whether to perform an ORIF or TEA. Fluoroscopy is not usually necessary when performing a TEA.
lateral decubitus position with the affected side up (Fig. 9.4). A tourniquet is used in all cases, nonsterile or sterile depending on the morphology of the arm. The injured extremity is supported on a padded bolster before prepping and draping. Alternatively, surgery can be performed in the supine position with the injured arm draped free on a sterile bolster across the patient’s chest. A sterile stockinette and flannel or an adherent wrap is placed on the hand. A first-generation cephalosporin is given intravenously prior to inflation of the tourniquet. Intraoperative imaging is necessary only if a decision has to be made on whether to perform an ORIF or TEA. Fluoroscopy is not usually necessary when performing a TEA.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree