Calcaneal Fractures: Open Reduction Internal Fixation
Michael P. Clare
Roy W. Sanders
INTRODUCTION
Fractures of the calcaneus are among the most challenging fractures for the orthopedic surgeon to effectively manage. Approximately 60% to 75% of all calcaneal fractures are displaced intra-articular fractures, and up to 90% of calcaneal fractures occur in young adult males in their working prime, which underscores the economic impact of these injuries (1,2). A thorough understanding of the relevant pathoanatomy and meticulous softtissue handling is essential in maximizing patient outcomes.
Mechanism of Injury
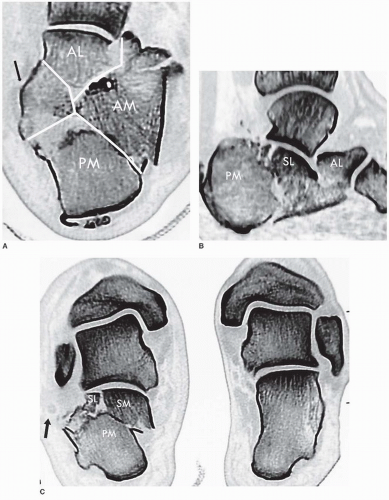
Displaced intra-articular calcaneal fractures generally occur as the result of high-energy trauma, such as a motor vehicle accident or a fall from a height. The mechanism of injury was first proposed by Essex-Lopresti (2) and later confirmed by Carr (3). At the moment of impact, the lateral process of the talus impacts the calcaneus at the crucial angle of Gissane as the subtalar joint is forced into eversion, which divides the lateral wall and body of the calcaneus, and produces the primary fracture line laterally. The residual force dissipates medially into the sustentaculum and, with continued force, extends into the anterior process or calcaneocuboid joint, producing an anterolateral fragment. A secondary fracture line then results from increased force: with a posteriorly directed force, the fracture line continues into and posterior to the posterior facet, producing a joint depression fracture, and with a more inferiorly directed force, the fracture line extends inferior to the posterior facet, producing a tongue-type fracture (Fig. 35.1A-C).
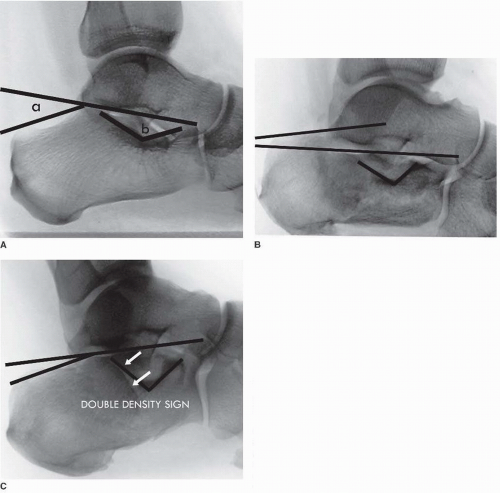
With displaced intra-articular calcaneal fractures, the loss of height through the calcaneus results in a shortened and widened heel, typically with varus malalignment of the tuberosity. This loss of height is reflected by a decreased tuber angle of Böhler, such that the normal downward tilt of the talus is diminished and the talus becomes relatively more horizontal (Fig. 35.2A-C). As the superolateral fragment of the posterior facet is impacted plantarward, the thin lateral wall explodes laterally just posterior to the crucial angle of Gissane. This lateral wall expansion may trap the peroneal tendons against the lateral malleolus; in some cases, a violent contracture of the peroneal tendons may disrupt the superior peroneal retinaculum from the fibula, resulting in an avulsion fracture of the lateral malleolus and dislocation of the peroneal tendons. The anterior process typically displaces superiorly, which directly limits subtalar joint motion by impinging against the lateral process of the talus.
Clarification of fragment terminology is necessary to understand the pathoanatomy of displaced intra-articular calcaneal fractures (Fig. 35.1A-C). The anterolateral fragment encompasses the lateral wall of the anterior process, is typically pyramidal in shape, and may include a portion of the calcaneocuboid articular surface. The anterior main fragment is the large fragment anterior to the primary fracture line, which usually includes the anterior portion of the sustentaculum and anterior process. The superomedial fragment, also known as the sustentacular or constant fragment, is the fragment of variable size found posterior to the primary fracture line; this fragment almost always remains attached to the talus through the deltoid ligament complex and is therefore stable. The superolateral fragment, also referred to as the semilunar or comet fragment, is the lateral portion of the posterior facet that is sheared from the remaining posterior facet in joint depression fractures. The tongue fragment refers to the superolateral fragment that remains attached to a portion of the posterior tuberosity including the Achilles tendon insertion and is found in tongue-type fractures. The posterior main fragment represents the posterior tuberosity.
INDICATIONS FOR OPERATIVE TREATMENT
Operative treatment is generally indicated for displaced intra-articular fractures involving the posterior facet. Specific indications include fractures with intra-articular posterior facet displacement ≥2 mm, ≥20% loss of calcaneal height, or significant lateral wall expansion. Surgical treatment allows restoration of calcaneal height, width, and overall morphology, in addition to the posterior facet articular surface where possible, and allows
for a late in situ arthrodesis as a means of salvage in the event of posttraumatic arthritis. The primary goal of surgery is anatomic restoration of alignment and return of function without pain.
for a late in situ arthrodesis as a means of salvage in the event of posttraumatic arthritis. The primary goal of surgery is anatomic restoration of alignment and return of function without pain.
CONTRAINDICATIONS FOR OPERATIVE TREATMENT
Nonoperative management is reserved for intra-articular fractures that are truly nondisplaced (Sanders type I) on computed tomography (CT) scan (4, 5 and 6). Other specific contraindications include fractures in patients with severe peripheral vascular disease or insulin-dependent diabetes mellitus and peripheral neuropathy, other medical comorbidities prohibiting surgery, and fractures in elderly patients who are minimal (household) ambulators (7). Chronological age itself is not necessarily a contraindication to surgical treatment, as many older patients are healthy and active well into their 70s (8). Although smoking itself is not a contraindication for surgery, patients who are smokers are counseled as to the risks of wound complications and encouraged to quit smoking; heavy smoking (>2 packs per day) is considered a relative contraindication to surgery. Similarly, patients with non-insulin-dependent diabetes mellitus and intact protective sensation are counseled regarding the importance of diligent blood glucose control but are still considered candidates for surgery.
PREOPERATIVE PLANNING
Clinical Evaluation
A patient with a calcaneal fracture typically experiences severe pain in the hind foot, which is related to bleeding into the limited soft-tissue envelope surrounding the heel. The severity of fracture displacement and the extent of soft-tissue disruption are proportional to the amount of force and energy involved in producing the injury—lower energy injuries produce more mild swelling and ecchymosis, while higher energy injuries result in severe soft-tissue disruption and may result in an open fracture.
Open Fractures
An open fracture of the calcaneus may present as a puncture wound medially from a prominent spike of bone from the medial wall of the calcaneus or as a more substantial wound with significant soft-tissue disruption, typically laterally or posteriorly. Open fractures are distinct injuries requiring different treatment and are generally associated with higher complication rates relative to closed fractures.
Compartment Syndrome of the Foot and Skin Necrosis
Within a few hours following the injury, soft-tissue swelling in the hind foot is typically so severe that skin creases in the area are no longer visible. In rare cases, severe swelling may produce a compartment syndrome of the foot, which, if untreated, can result in clawtoe deformities, contracture, weakness, and loss of function. Thus, it is important to ensure that pain associated with the fracture is not due to a compartment syndrome, particularly in the calcaneal compartment, which is contiguous with the deep posterior compartment of the leg. With tongue-type fractures, significant displacement of the tongue fragment may place excessive pressure on the posterior skin, causing necrosis if left untreated.
Associated Injuries
A high index of suspicion must be maintained for other associated injuries, including lumbar spine fractures or other fractures of the lower extremities, particularly with falls from a height. Up to 50% of patients with calcaneus fractures may have other associated injuries—intuitively, these injuries are more common in higherenergy trauma. Appropriate diagnostic evaluation should thus be completed where necessary.
Resolution of Soft-Tissue Swelling
Surgery is ideally performed within the first 3 weeks of injury prior to early consolidation of the fracture. Once fracture consolidation ensues, the fragments become increasingly difficult to separate to obtain an adequate reduction, and the articular cartilage may delaminate from the underlying subchondral bone. Surgery must be delayed, however, until the associated soft-tissue swelling has adequately dissipated, which may require up to 3 weeks. We utilize a Jones dressing and supportive splint initially, combined with limb elevation. Once the initial edema has begun to dissipate, the patient is converted to an elastic compression stocking and fracture boot. Sufficient resolution of soft-tissue edema is indicated by a positive wrinkle test, in which the lateral calcaneal skin is visually assessed and palpated with the foot positioned in dorsiflexion and eversion. The test is positive if skin wrinkling is seen, and no pitting edema remains, indicating that surgical intervention may be safely undertaken (5).
RADIOLOGIC EVALUATION
Plain Radiography
With a suspected calcaneal fracture, plain radiographic evaluation should include a lateral view of the hind foot, an anteroposterior view of the foot, an axial view of the heel, and a mortise view of the ankle.
A calcaneal fracture is most easily identified on the lateral view of the hind foot. With an intra-articular fracture, there is a loss of height in the posterior facet—the articular surface is impacted within the body of the calcaneus and usually rotated anteriorly up to 90 degrees relative to the remaining subtalar joint; a decreased tuber angle of Böhler and an increased crucial angle of Gissane are seen in fracture patterns where the entire posterior facet is separated from the sustentaculum and depressed (Fig. 35.2B); if only the lateral portion of the posterior facet is involved, the split in the articular surface is manifest as a “double density,” in which case the tuber angle of Böhler and crucial angle of Gissane may appear normal (Fig. 35.2C). The lateral view also allows delineation as to whether the fracture is a joint depression or tongue-type fracture (2).
The anteroposterior view of the foot is helpful to identify if there is fracture extension into the calcaneocuboid joint, anterolateral fragments, and widening of the lateral calcaneal wall. The Harris axial view of the heel shows a loss of calcaneal height, increased width, and (typically) varus angulation of the tuberosity fragment, as well as visualization of the articular surface. A mortise view of the ankle often demonstrates involvement of the posterior facet.
Computed Tomography
If the plain radiographs reveal intra-articular extension of the calcaneal fracture, CT scanning is indicated. Images are obtained in 2 to 3-mm intervals in the axial, sagittal, and 30-degree semicoronal planes.
The axial or transverse cuts reveal extension of fracture lines into the anterior process and calcaneocuboid joint as well as the sustentaculum tali and anteroinferior margin of the posterior facet (Fig. 35.1A). The sagittal views demonstrate displacement of the tuberosity fragment, extent of involvement of the anterior process including superior displacement of the anterolateral fragment, anterior rotation of the superolateral posterior facet fragment, and delineation of the fracture as a joint depression or tongue-type pattern (Fig 35.1B) (2). The 30-degree semicoronal images show displacement of articular fragments in the posterior facet, the sustentaculum tali, the extent of widening and shortening of the calcaneal body, expansion of the lateral calcaneal wall, varus angulation of the tuberosity, and location of the peroneal tendons (Fig. 35.1C).
SURGICAL TECHNIQUE
Although a variety of surgical approaches have been described, we prefer the extensile lateral approach for displaced intra-articular fractures, as it consistently allows reduction of the calcaneal body, restoration of calcaneal height and width, even with severe comminution, as well as reduction of the intra-articular surface where possible (6).
OPEN REDUCTION INTERNAL FIXATION: EXTENSILE LATERAL APPROACH FOR JOINT DEPRESSION-TYPE FRACTURES
Patient Positioning/Draping/C-Arm
The patient is given preoperative prophylactic antibiotics and positioned on an operating table with a radiolucent far end is utilized, preferably one with a “diving board” type attachment (i.e., without table legs distally) to facilitate surgeon position and intraoperative fluoroscopy. The patient is placed in the lateral decubitus position on a beanbag. The lower extremities are positioned in a scissor configuration, whereby the operative limb is flexed at the knee and angles toward the distal, posterior corner of the operating table, while the nonoperative limb is extended at the knee and lies away from the eventual surgical field. Protective padding is placed beneath the contralateral limb to protect the peroneal nerve, and an operating “platform” is created with blankets or foam padding to elevate the operative limb (Fig. 35.3).
A pneumatic thigh tourniquet is used in all cases. The procedure should be completed within 120 to 130 minutes of tourniquet time, in order to minimize potential wound complications. A standard C-arm should be utilized rather than a “mini” C-arm, because the arc of “C” is too small to fit around the operating table for a true lateral view. The C-arm approaches the surgical field from opposite the surgeon and perpendicular to the table.
Approach
Soft-tissue complications following the surgical management of calcaneal fractures remain a major source of morbidity with these injuries. Thus, careful attention to detail with respect to placement of the incision and gentle handling of the soft tissues are of paramount importance. The vertical limb of the incision begins
2 cm proximal to the tip of the lateral malleolus, immediately lateral to the Achilles tendon and thus posterior to the sural nerve and the lateral calcaneal artery (9), and extends toward the plantar foot. The horizontal limb continues at the junction of the skin of the lateral foot and heel pad, with a gentle curve connecting the two limbs of the incision (Fig. 35.4A). Dissection is specifically taken “straight to bone” at the level of the calcaneal tuberosity proximally and continues to the midpoint of the horizontal limb.
2 cm proximal to the tip of the lateral malleolus, immediately lateral to the Achilles tendon and thus posterior to the sural nerve and the lateral calcaneal artery (9), and extends toward the plantar foot. The horizontal limb continues at the junction of the skin of the lateral foot and heel pad, with a gentle curve connecting the two limbs of the incision (Fig. 35.4A). Dissection is specifically taken “straight to bone” at the level of the calcaneal tuberosity proximally and continues to the midpoint of the horizontal limb.
 FIGURE 35.3 Intraoperative positioning for extensile lateral approach. Note scissor configuration of operative and nonoperative limbs and operating platform. |
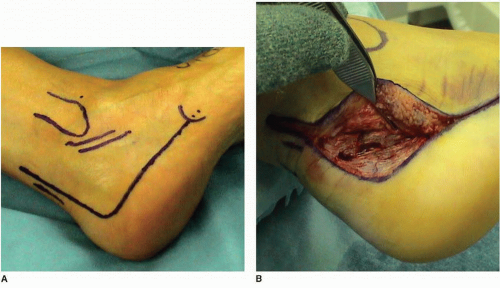 FIGURE 35.4 Extensile lateral approach. A. Proposed incision. B. Full-thickness subperiosteal flap using “no touch” technique.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|