Humeral Shaft Fractures: Open Reduction Internal Fixation
Bruce H. Ziran
Navid M. Ziran
INTRODUCTION
The humerus, like the femur, is a single large tubular bone protected by a large circumferential muscle envelope. Fractures of the humerus are common injuries and account for 2% to 3% of all fractures seen in clinical practice. They follow a classic bimodal distribution with lower-energy injuries in the elderly and higher-energy fractures in younger patients. The humerus is designated as number 1 in the AO/OTA classification, with fractures of the proximal, middle, or distal third assigned a second numeral one, two, or three, respectively. The classification is further subdivided based on articular involvement or complexity into A, B, and C patterns (Fig. 6.1). Most fractures of the humerus occur in the middle one-third and are managed nonoperatively with initial splinting and conversion to a functional brace 10 to 14 days after injury. With nonoperative treatment, nonunion rates are <2% for closed fractures and 6% for open fractures (1). Regardless of the method of treatment, the goals for the surgeon and patient remain fracture union with good alignment and rotation along with restoration of shoulder and elbow function. While there is broad consensus regarding many aspects of humeral fracture care, several treatment controversies remain. These include the indications for nonoperative versus surgical management, when to use a nail versus a plate, the use of conventional versus locked plating, the number of cortices required for fixation, and the management of associated radial nerve palsies. This chapter discusses current concepts in management as well as the surgical approaches to the humeral shaft.
INDICATIONS AND CONTRAINDICATIONS FOR SURGERY
The majority of isolated lower-energy closed humeral shaft fractures are best managed nonoperatively. Klenerman first established guidelines for nonsurgical management in 1966. These guidelines were based more on the cosmetic appearance of the limb rather than functional outcomes. He proposed upper limits of 30 degrees of varus, 20 degrees apex anterior angulation, 15 degrees of malrotation, and 3 cm of shortening as compatible with good function. In general, malunions following nonoperative treatment of humerus fractures are well tolerated due to the compensatory range of motion at the shoulder and elbow and are predominantly a cosmetic issue. Additionally, the large muscle mass of the upper arm conceals moderate degrees of deformity (1).
Strong indications for surgical repair of displaced humeral shaft fractures include the following (Table 6.1).
Polytrauma
The multiply injured patient with a concomitant humeral shaft fracture may benefit from early surgical stabilization to improve mobilization, facilitate nursing care, and decrease pain (2, 3 and 4). However, the optimal timing for surgical fixation in these patients is unknown since many of these patients have other serious injuries, and
early or ill-advised surgery may activate the systemic inflammatory response system leading to a “second hit” phenomena. Most patients with closed fractures who are unable to undergo early surgery should be placed into a well-padded coaptation splint. In patients with open fractures, temporary external fixation can be helpful (damage-control orthopaedics) with conversion to internal fixation when the patient’s overall condition permits (5). If external fixation is performed, the pins should be placed away from the fracture zone to decrease the risk of infection.
early or ill-advised surgery may activate the systemic inflammatory response system leading to a “second hit” phenomena. Most patients with closed fractures who are unable to undergo early surgery should be placed into a well-padded coaptation splint. In patients with open fractures, temporary external fixation can be helpful (damage-control orthopaedics) with conversion to internal fixation when the patient’s overall condition permits (5). If external fixation is performed, the pins should be placed away from the fracture zone to decrease the risk of infection.
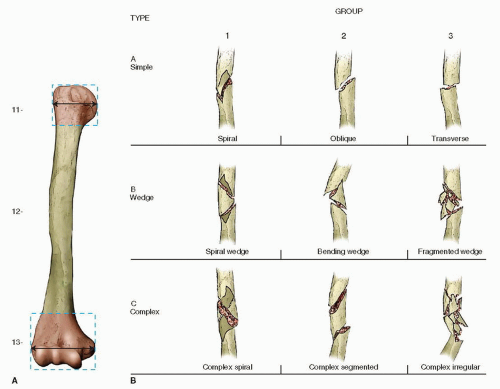 FIGURE 6.1 AO/OTA classification of humeral shaft fractures. The humerus is designated as number 1. The second number refers to the location along the shaft (proximal = 1, middle = 2, distal = 3)—the humeral diaphysis would be designated as 1 and 2. The letters A, B, and C refer to the type of the diaphyseal fracture (simple, wedge, or complex) with further numeral classification (1, 2, 3) based on fracture group. Lastly, subgroup classification further localizes the fracture to the proximal, middle, or distal zone (.1,.2, or.3, respectively). For example, a simple, oblique midshaft humeral shaft fracture would be 12-A2.1. |
TABLE 6.1 Indications for Surgical Fixation of Humeral Shaft Fractures | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
Segmental Fractures
Segmental fractures with significant fragment displacement or angulation are difficult to manage nonoperatively. Intramedullary nailing or plate osteosynthesis may be indicated to prevent malunion or nonunion. Minimally displaced segmental humeral shaft fractures can often be treated nonoperatively if alignment can be maintained.
Ipsilateral Forearm Fracture
Patients with both a displaced humeral shaft and ipsilateral forearm fracture—the so-called floating elbow— often benefit from early internal fixation of both fractures to facilitate rehabilitation of the elbow. Nonoperative treatment of the humeral fracture is associated with an increased risk of nonunion in this infrequent injury pattern (6).
Pathologic Fracture
Impending and pathologic fractures of the humerus are usually the result of metastatic cancer, and patients often benefit from internal fixation to relieve pain and improve function. Due to compromised bone and the possibility of skip lesions, locked intramedullary nailing is the preferred method of treatment because of less surgical dissection, technical ease, and satisfactory pain relief (7). In patients with very proximal and distal pathologic lesions, locked plating with or without cement augmentation may provide better stability.
Bilateral Fractures
Simultaneous fracture of both humeri is uncommon and is usually associated with polytrauma. These patients often benefit from fixation of either one or both fractures to improve rehabilitation, ease nursing care, and decrease pain.
Vascular Injury
Combined vascular injury and humeral shaft fractures can be limb-threatening injuries. The order of treatment is based on the ischemic state of the limb. When vascularization is the priority, a simple external fixation device should be employed to stabilize the fracture out to length and prevent disruption of the vascular repair when internal fixation is required. In a smaller number of cases, the use of a temporary vascular shunt allows more definitive fracture treatment followed by vascular repair.
Ipsilateral Brachial Plexus Injury
There is very little literature on humeral shaft fractures with ipsilateral brachial plexus injuries. Brien et al. (8) showed improved union rates following plate fixation of the humerus compared to external fixation or intramedullary nailing.
Open Fractures
Open fractures of the humerus usually require prompt stabilization after irrigation and débridement. In lowergrade open fractures, immediate internal fixation is safe and effective if the patient’s overall condition permits. In high-grade open injuries, if the wound is contaminated or there is a significant soft-tissue disruption, irrigation and débridement with temporary external fixation should be strongly considered.
PREOPERATIVE PLANNING
History and Physical Exam
A careful history and physical exam should be performed on all patients with a humerus fracture. The history should identify the mechanism of injury (low- vs. high-energy, ballistic injury, etc.), pertinent comorbidities (diabetes mellitus, cardiac problems, etc.), pertinent past surgical history, medications, and drug allergies. hand dominance with any upper-extremity injury should be established. The physical exam should evaluate and
document objective findings such as swelling, ecchymosis, open wounds, neurologic status, and peripheral pulses. A full trauma workup is necessary in patients with high-energy trauma, complex associated injuries and in patients who are obtunded or have a closed-head injury.
document objective findings such as swelling, ecchymosis, open wounds, neurologic status, and peripheral pulses. A full trauma workup is necessary in patients with high-energy trauma, complex associated injuries and in patients who are obtunded or have a closed-head injury.
Imaging Studies
In patients with suspected extremity injuries, anteroposterior (AP) and lateral radiographs should be obtained that include the “joint above and below.” Frequently, due to significant pain, high-quality orthogonal radiographs are difficult to obtain in the conscious patient. Traction films with light sedation can be helpful in a cooperative patient. For some patients, optimal films cannot be obtained until the patient is under anesthesia in the operating room. CT scans are not usually necessary and are most often used in humeral fractures with proximal or distal fracture extension into shoulder or elbow joints.
Timing of Surgery
The timing of surgery with humeral shaft fractures depends on whether the fracture is open or closed. With open fractures, irrigation and débridement should be performed as soon as the patient’s condition and institutional resources permit. Patients with Grade I and II open fractures who are also hemodynamically stable may benefit from immediate internal fixation. In Grade III open fractures or in patients with highly contaminated wounds, splinting or external fixation is preferred with delayed internal fixation. If there is a vascular injury, exploration, repair, and external fixation should be performed urgently in collaboration with a vascular surgeon. Low-velocity gunshot wounds without a neurovascular injury are treated with local wound care, antibiotic administration, and fracture stabilization if indicated. For most closed fractures of the humerus, internal fixation can be performed electively in the first few days.
Surgical Tactic
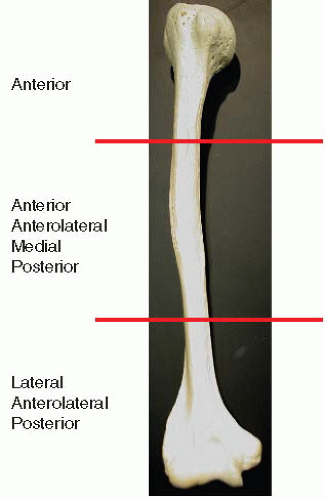
Part of the preoperative plan includes choosing an appropriate surgical approach based on the location of the fracture or traumatic wound (Fig. 6.2). Fractures that are located in the proximal and midshaft of the humerus are usually addressed through an anterior or anterolateral approach. The straight lateral approach has also been advocated for midshaft fractures, but extensive mobilization of the radial nerve with this exposure increases the chance of an iatrogenic injury. The posterior approach is most often used for fractures in the distal one half of the humerus. However, patient positioning makes it more difficult in multiply injured patients. The distal anterolateral approach was less useful in the past because contouring a plate to the anterolateral column was difficult, and there was limited opportunity for fixation in the relatively narrow lateral pillar. However, newer locked plating systems provide better fixation in “short” segment situations and now make the anterolateral approach a more attractive option for selected distal fractures. A summary of the approach and plate placement based on fracture location is shown in Table 6.2.
TABLE 6.2 Surgical Approach and Plate Placement Based on Anatomic Fracture Location | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
In open fractures, some of the soft-tissue dissection may have occurred due to soft-tissue stripping at the time of injury and may influence the surgical approach. Surgical “versatility” is important to minimize additional soft-tissue injury by performing a separate approach through compromised soft tissues. If the soft-tissue lesion is primarily on the medial aspect of the arm, the surgeon should be prepared to utilize a medial approach for fixation.
RADIAL NERVE INJURY
The function of the radial nerve is critical, and its integrity must be carefully evaluated and documented in patients with humeral shaft fractures. A radial nerve palsy that occurs at the time of fracture is seen in 6% to 15% of cases (9, 10 and 11). A recent meta-analysis of more than 1,000 cases of humeral fractures documented an average incidence of radial nerve lesions in 11.8% of patients (12). In closed fractures, these injuries are usually a neuropraxia and are seen most commonly in fractures in the lower third of the humerus (13). Numerous studies have shown that treatment is observation since spontaneous recovery occurs in the vast majority of cases (9, 10 and 11).
On the other hand, if the radial nerve palsy occurs in the presence of an open fracture, most authors favor nerve exploration and fracture stabilization since the nerve is frequently damaged or interposed between fracture fragments (14). If there is a clean transection of the nerve with minimal soft-tissue contamination, acute repair is indicated. In patients with gross contamination or traumatic nerve loss, delayed reconstruction is preferable. In nerve lesions that span several centimeters, shortening of the humerus by 2 to 3 cm may facilitate a tensionfree nerve repair. In irreparable nerve lesions, cable grafting with or without tendon transfers may be indicated.
The management of a radial nerve palsy after closed reduction (secondary nerve palsy) is more controversial. In a meta-analysis of over 1,000 humeral fractures, Shao et al. (12) demonstrated no significant difference in recovery rate between primary (88.6%) and secondary (93.1%) nerve palsies (including those palsies after closed reduction)—although the number of secondary nerve palsies from closed reduction was not quantitated in this study.
The treatment of a radial nerve palsy includes functional splinting of the wrist and hand as well as range of motion to prevent contractures. Electromyography/nerve conduction velocity studies should be performed between 4 and 12 weeks after injury if there are no clinical signs of recovery. A positive prognostic sign of recovery is an advancing Tinel’s sign indicating the nerve regeneration. The brachioradialis is the first muscle to recover, but wrist extension is easier to monitor.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree