69
Scapholunate Advanced Collapse
Andrew H. Borom and David B. Siegel
History and Clinical Presentation
A 54-year-old right hand dominant man who works as a museum director presented with a 3-year history of gradually increasing pain, swelling, and loss of mobility in his right wrist. He also noted the recent onset of nocturnal paresthesias in the sensory distribution of the median nerve. There was no history of trauma, although he had played professional basketball for 12 years. A wrist splint, nonsteroidal antiinflammatory medication, and therapeutic modalities did not relieve his symptoms.
PEARLS
- The status of the articular cartilage on the proximal surface of the capitate is critical. Radiographic and intraoperative findings must be reconciled, and a decision must be made at the time of surgery as to the procedure chosen.
- In both operative procedures (proximal row carpectomy and 4-bone arthrodesis) a partial denervation of the wrist is indicated by excision of the terminal branch of the posterior interosseous nerve in the floor of the fourth dorsal compartment.
- Leaving a thin volar shell of bone avoids violation of the palmar extrinsic radiocarpal ligaments and does not appear to compromise the result.
PITFALLS
- Failure to reduce and stabilize the capitolunate joint in the four-bone arthrodesis will compromise outcome and reduce postoperative extension secondary to radiocapitate impingement.
- The pins used to stabilize the intercarpal fusion should not cross the radiocarpal joint.
- Silicone implants to replace the scaphoid are contraindicated, and biologic interposition material adds nothing to success.
Physical Examination
The right wrist had an effusion and was tender over the radial styloid-scaphoid joint. Range of motion was restricted to less than 50% of the contralateral side with complete loss of radial deviation. Extension and radial deviation were most painful. A scaphoid shift test provoked pain but no scaphoid subluxation. Provocative signs for carpal tunnel syndrome were positive; however, there was no thenar atrophy.
Diagnostic Studies
Radiographic imaging included posteroanterior, lateral, and scaphoid oblique views. There was narrowing of the joint space between the radial styloid process and the scaphoid, widening of the scapholunate joint, malrotation of the scaphoid, and narrowing of the capitolunate joint space (Fig. 69–1). There was beaking of the radial styloid process. Electrical diagnostic studies confirmed the presence of carpal tunnel syndrome.
Differential Diagnosis
Posttraumatic osteoarthritis
Scapholunate advanced collapse
Scaphoid nonunion or malunion with collapse
Distal radius fracture with radiocarpal collapse
Inflammatory arthritis
Rheumatoid arthritis
Gout
Diagnosis
Scapholunate Advanced Collapse Pattern of Osteoarthritis
Chronic scapholunate dissociation leads to a predictable pattern of degenerative changes in the radiocarpal and midcarpal joints. The incongruent joint surfaces between the radius and malrotated scaphoid, as well as those between the head of the capitate and dorsiflexed lunate, lead to osteoarthritis. The radiolunate joint is preserved, as it maintains a congruent relationship despite the rotatory malalignment. Joint deterioration follows a predictable sequence with well-described radiographic findings.
Figure 69–1 Preoperative radiograph demonstrates collapse of the radioscaphoid joint, marginal osteophyte formation at the distal tip of the radial styloid process, and mild narrowing of the capitolunate joint.
In stage I, the distal scaphoid-radial styloid articulation narrows and the styloid process develops a marginal osteophyte, which appears as a distally pointing beak. In stage II, the entire radioscaphoid articulation is involved. In stage III, the capitolunate and scaphocapitate joints are involved. Rarely, there is progression to pancarpal arthritis. Subchondral sclerosis and lytic areas suggesting cyst formation are also seen radiographically. This pattern of joint degeneration may also be seen in association with scaphoid nonunion, scaphoid malunion, midcarpal instability, and following other carpal fractures (e.g., scaphocapitate syndrome). This pattern of osteoarthritis is not seen as a late sequela of Kienbock’s disease. The progression to osteoarthritis takes many years and has been seen in asymptomatic individuals as an incidental finding.
Plain radiographs are diagnostic. Other imaging studies are not needed unless associated pathology is suspected. Similarly, if the symptoms are severe enough to consider surgery, then arthroscopy is not indicated, as the wrist joint will be exposed adequately to visualize the pathology. Electrical diagnostic studies may be indicated if there is associated compressive neuropathy of the median nerve.
Nonsurgical Management
The objective of conservative management is to reduce pain. There is little hope of restoring mobility or strength with nonoperative treatment, and attempts to do so usually result in increased pain. Nonsteroidal antiinflammatory and nonnarcotic analgesic medications may be beneficial symptomatically. Wrist or thumb spica splints, applied with the wrist in a comfortable resting position, may provide some relief. Corticosteroid injections with local anesthetic into the radioscaphoid or capitolunate joints may provide transient relief, but rarely have long-term benefit.
Surgical Management
The currently accepted operative procedures are based on the elimination of the radioscaphoid and capitolunate joints. Proximal row carpectomy accomplishes this by excising the scaphoid, lunate, and triquetrum, and preserves motion through the newly created radiocapitate joint. An alternative procedure is scaphoid excision and arthrodesis of the capitate, lunate, triquetrum, and hamate. Total wrist arthrodesis is reserved for the wrist with associated radiolunate arthritis.
Proximal Row Carpectomy
The major prerequisite for this operation is that the articular cartilage on the proximal surface of the capitate and on the lunate fossa of the distal radius is preserved. If there is grossly visible fissuring, cartilage softening, or eburnation on the head of the capitate, then scaphoid excision and four-bone fusion should be performed. Proximal row carpectomy is reserved for stage I and stage II disease.
The wrist joint is approached through a dorsal longitudinal incision. A longitudinal capsulotomy is created with full-thickness capsular flaps elevated radially and ulnarly, preserving the dorsal intercarpal ligament. Initially the lunate is excised, followed by the triquetrum and scaphoid. The extrinsic radiocarpal and ulnocarpal ligaments are preserved. Kirschner wires are often inserted into each of the bones to control rotation and facilitate exposure. It is frequently necessary to fragment the scaphoid to expose the distal pole. The capitate is then translated proximally into the lunate fossa of the radius. Radiographically it appears that the trapezium impinges on the radial styloid process in radial deviation of the wrist. This should be examined intraoperatively, and if there is any impingement, a limited radial styloidectomy is performed, preserving the radioscaphocapitate ligament. However, the trapezium is palmar to the styloid and we rarely find styloidectomy necessary. It has been demonstrated radiographically that the radius of curvature of the proximal pole of the capitate is 60% to 67% of that of the lunate, and that motion at the radiocapitate joint is a combination of angular rotation and translation. This hinge roll is lost if the dorsal capsule is closed too tightly. The joint is not pinned routinely.
The wrist is immobilized in neutral alignment for up to 4 weeks and protective splinting is used for an additional month. Strengthening is allowed after 3 months.
Scaphoid Excision and Ulnar Four-Bone Arthrodesis
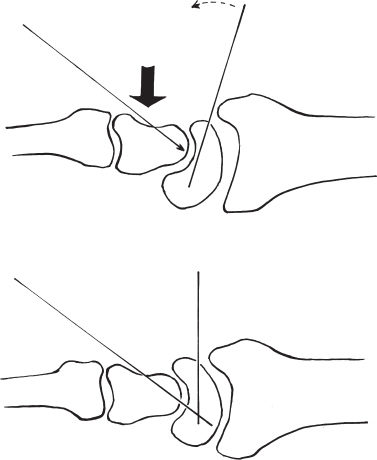
In this patient, the articular cartilage at the head of the capitate was found to be severely degenerated. Therefore, proximal row carpectomy was no longer an option. Conceptually, scaphoid excision and ulnar four-bone fusion should have a better long-term outcome since the radius of curvature of the lunate and radius is the same, and the uninvolved ulnocarpal relationship is preserved. The joint is approached in an identical fashion and the scaphoid excised. The adjoining surfaces of the capitate, lunate, triquetrum, and hamate are decorticated with a rongeur. When decorticating the lunotriquetral joint, it is imperative that the interosseous ligament be preserved. The capitolunate joint is reduced and secured with pin fixation (Fig. 69–2). This reduction to a neutral axial alignment is critical. Furthermore, it is important that the midcarpal joint not be compressed. After pinning, the space between carpal bones is filled with cancellous bone graft harvested from the distal radius (Fig. 69–3). No interposition material is used to fill the defect created by scaphoid excision. The dorsal capsule is approximated, and the wrist immobilized in a short-arm cast for 6 weeks. A splint is applied after cast removal and range-of-motion exercises are begun with the pins in place. Pins are removed after 10 weeks, or when union occurs radiographically.