CHAPTER 35 Rupture of the Triceps Tendon
INTRODUCTION
Rupture of the triceps tendon is rare.1,2,3 Anzel and colleagues2 reported that 85% of the 1015 tendon injuries treated at the Mayo Clinic involved the upper extremity. Of this group of 856, only 8 instances of triceps tendon injury were reported, and 4 of these were due to laceration. Since the first report of Partridge in 1868 as cited by Bennett,5 as of 2000, fewer than 50 instances have been recorded in the English literature.6,9,10,11 Unlike ruptures of the distal biceps tendon, this may occur both in men and women, with a female to male ratio of 2:3. The mean age of occurrence is about 33 years, but rupture has been observed in a broader spectrum of ages including children (aged 7) to adolescents in whom the olecranon physes has just closed,14 to individuals in the eighth decade.15
MECHANISM OF INJURY
Rupture of the triceps tendon may occur either spontaneously, after trauma, or after surgical release and reattachment. Two types of traumatic episodes may be implicated. The most common event is a deceleration force imparted to the arm during extension as the triceps muscle is contracting. This usually occurs during a fall, but avulsion has been reported due to simple, uncoordinated triceps muscle contraction against a flexing elbow.4,26 The association of triceps tendon avulsion39 or tear19 associated with body builders is consistent with the observation of muscle unit damage associated with eccentric contractures in the unconditioned muscle.24,31 The possibility of anabolic steroid usage must also be considered in this type of patient. A direct blow to the posterior aspect of the triceps at its insertion in varying positions also has been reported in several instances1,33,45 but is probably an uncommon mechanism of injury.
PREDISPOSING CONDITIONS
An association of olecranon bursitis has been noted to predispose to triceps tendon rupture.10 Disruption of the triceps also may occur spontaneously with minimal trauma in individuals who are compromised by a systemic disease process,35 such as renal osteodystrophy and secondary hyperparathyroidism.9,15 Although the pathophysiology of this association has not been completely explained, an increased amount of elastic fibers in the tendons of patients with renal osteodystrophy undergoing dialysis has been reported.29 Calcification due to the chronic hypercalcemia of secondary hyperparathyroidism may be yet another explanation for the associated tendon ruptures in this group of patients.35 Ruptures also have been reported in association with steroid treatment for lupus erythematosus45 and chronic acidosis,29 and in individuals with osteogenesis imperfecta tarda25 or Marfan’s syndrome.38 Diabetes has been recently implicated in a patient with triceps rupture at the musculotendinous junction.44
In spite of the association with debilitating states and conditions, this injury is well recognized in the athletic population as well. Such diverse activities as power weightlifting and handball have been implicated.13,19,24,39 It should be noted that the injury can be associated with localized hematoma, and there are reports of ulnar nerve compression as a result of hematoma compression after triceps rupture in power lifters.13,19 Triceps deficiency occurring after total elbow replacement is obviously a problem of exposure, and repair and is discussed elsewhere.7
DIAGNOSIS
Without question, a history of acute pain and weakness in extension or an eccentric loading in flexion against forcible triceps contracture, such as a fall on the outstretched hand, is the most reliable method of making this diagnosis. A palpable defect is present in some instances, depending on the extent of triceps retraction (Fig. 35-1). Injury to the muscular tendinous junction results in pain proximal to the olecranon.3,30 Some loss of extension power is universally observed. Some active elbow extension may be present, but extension against gravity is not possible with a complete rupture. The length/tension relationship of the triceps has been studied by Hughes and associates,20 who found that as little as 2 cm shortening between origin and insertion causes a marked (40%) loss of strength.
IMAGING
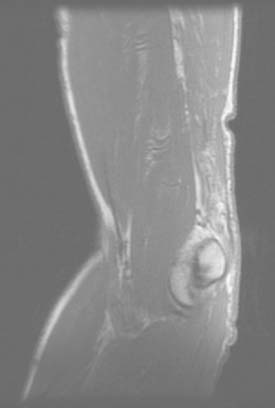
Today, imaging is a most reliable means of making a definitive diagnosis that more precisely defines the location and nature of the tear. A plain radiograph is extremely useful in that uncommon instance in which the triceps rupture occurs with a fleck of bone readilyidentified in the lateral film15,35,38 (Fig. 35-2). Without question, however, the advent of the magnetic resonant imaging has provided an accurate and reliable means of not only diagnosing this injury but also localizing the site and the extent of the pathology (Fig. 35-3).16,34 Ultrasonic diagnosis is also emerging as a reliable and less expensive imaging modality.31,34

FIGURE 35-2 Radiograph of a patient with triceps rupture. The fragment is readily viewed on the lateral film.
PATHOLOGY
Theoretically, three sites of failure may occur and these have also been observed clinically: the muscle belly, the musculotendinous junction, and the osseous tendon insertion.27 For this particular injury, the failure has occurred almost universally at the site of insertion, although failure at the musculotendinous junction has occasionally been reported.18,28,44
Associated injuries also have been reported. Several instances of concurrent fracture of the radial head have been noted,35,42 and a recent report of six such injuries suggests that the association may be more common than is appreciated.23 I have not diagnosed this combination in my practice. A single report of fracture of the wrist22 along with fracture of the radial head supports the case for the mechanism of injury being a fall on the outstretched hand.
PHYSICAL EXAMINATION
The diagnosis of a partial rupture may be difficult. Pain is not dysfunctional; thus, a number of patients present several weeks after the acute event.21 Furthermore, some weak residual extension power may be provided by the anconeus/triceps expansion. This effect can be negated by observing the inability to extend overhead against gravity. The radiograph is of considerable benefit for diagnosis of this injury in some patients, because flecks of avulsed bone are apparent on the lateral film (see Fig. 35-2).14,41
TREATMENT
PARTIAL RUPTURES
Incomplete tendon rupture should be initially treated nonoperatively.1 However, a distinction must be made between a true partial insertional rupture and one occurring at the musculotendinous junction. Improved imaging modalities are helpful to make this distinction.16,34 A true partial detachment from the olecranon does not reliably heal. With an acute injury, we do favor protecting the extremity and observing the amount of progress over a 6- to 8-week period. A strain of the attachment or of the musculotendinous junction will improve. Although appearing to heal, partial ruptures will continue to be symptomatic with increased activity. In the event that there is no clinical contraindication, surgical intervention is indicated. If there is evidence of healing by progressive resolution of symptoms, then in our judgment this represents a strain and not a rupture and nonoperative management is recommended.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree