Partial-thickness tear (P): classification according to Ellman
Grade
Size
I
<3 mm deep
II
3–6 mm deep
III
>6 mm deep
Localization
A
Articular surface
B
Bursal surface
C
Interstitial
Partial-thickness tears: classification according to Snyder | |
|---|---|
Type | Location of the tear |
A | Articular surface |
B | Bursal surface |
Type | Severity of the tear |
0 | Normal cuff, with smooth coverings of synovia and bursa |
I | Minimal, superficial bursal or synovia irritation or slight capsular in a small localized area; usually <1 cm |
II | Actually fraying and failure of some rotator cuff fibers in addition to synovial, bursal or capsular injury, usually <2 cm |
III | More severe rotator cuff injury, including fraying and fragmentation of tendon fibers, often involving the whole surface of a cuff tendon (most often the supraspinatus); usually <3 cm |
IV | Very severe partial rotator cuff tear that usually contains, in addition to fraying and fragmentation of tendon tissue, a sizable flap tear and often encompasses more than a single tendon |
Most classifications of full-thickness tears involve the superior and posterior rotator cuff. They comprise the involved tendons and their tear size in the sagittal and frontal plane. The classifications according to Ellman, Bateman, and Patte are commonly used (Tables 1.3, 1.4, and 1.5).
Full-thickness tear (F): classification according to Ellman | ||
|---|---|---|
Grade | Size | Description |
I | <2 cm | Small |
II | 2–4 cm | Large |
III | >4 cm | Massive |
IV | Cuff arthropathy | |
Localization: | ||
A | Supraspinatus | |
B | Infraspinatus | |
C | Teres minor | |
D | Subscapularis | |
Full-thickness tear: classification according to Bateman | ||
|---|---|---|
Grade | Size | Description |
I | <1 cm | Small |
II | 1–3 cm | Medium |
III | 3–5 cm | Large |
IV | >5 cm | Massive |
Table 1.5
Classification of full-thickness tears regarding the amount of tendon retraction according to Patte [12]
Full-thickness tear: classification according to Patte | |
|---|---|
Grade | Description |
I | Tendon between greater tuberosity and apex humeri |
II | Tendon between apex humeri and glenoid |
III | Tendon medial to glenoid |
Evaluation of muscle atrophy and fatty degeneration is important. This information provides valuable prognostic factors in addition to the tear size and retraction. Thomazaeu suggests that the ratio (R) of the supraspinatus muscle belly surface (S1) and the supraspinatus fossa surface (S2) is a good tool for estimating the degree of supraspinatus muscle atrophy [13]. Alternatively, according to Zanetti [14], the tangent sign is a quick, commonly used diagnostic procedure (Tables 1.6 and 1.7).
Supraspinatus atrophy: classification according to Thomazeau | ||
|---|---|---|
Grade | Ratio muscle/fossa supraspinata | Description |
I | 1.00–0.60 | Normal or mild atrophy |
II | 0.60–0.40 | Moderate atrophy |
III | <0.40 | Severe atrophy |
Supraspinatus atrophy in MRI: classification according to Zanetti | |
|---|---|
Positive tangent sign | A line (“tangent”) is drawn through the superior borders of the scapular spine and the superior margin of the coracoid. |
Supraspinatus muscle lies underneath the tangent. | |
Negative tangent sign | A line (“tangent”) is drawn through the superior borders of the scapular spine and the superior margin of the coracoid. |
Supraspinatus muscle lies above the tangent. | |
Subscapularis tendon tears can also be classified according to Fox and Romeo (Table 1.8).
Tears of the subscapularis: classification according to Fox and Romeo | |
|---|---|
Type | Description |
I | Partial thickness tear |
II | Complete tear of the upper 25 % of the tendon |
III | Complete tear of the upper 50 % of the tendon |
IV | Complete rupture of the tendon |
1.5 Diagnostics
1.5.1 History
The typical history contains pain at night and painful elevation of the arm above the horizontal plane. Additionally, a loss of power may be observed. In advanced or acute cases, the patient is unable to elevate the arm at all; a pseudo-paralysis occurs. Many patients report a recent moderate trauma, however, most of cuff tears derive from a degenerative disease.
1.5.2 Clinical Examination
The clinical examination begins with the inspection of the complete shoulder girdle. Atrophies of the supraspinatus and infraspinatus muscles can be easily detected. Palpation of the anatomic landmarks is helpful to elicit pain spots. The active and passive range of motion should be documented according to the neutral zero method and functionally as well. Signs of capsular stiffness are crucial. Functional isometric testing of each rotator muscle is helpful but should be considered with care inasmuch as the powerful deltoid muscle might distort the involvement of the rotator cuff muscles. In these cases, the lag signs according to Hertel are valuable tests [16]. Additionally, impingement tests, according to Neer, Hawkins, and Kennedy, may underline the diagnosis. Specific tests for detecting pathologies of the long head of the biceps are also useful because they are seen frequently in association with rotator cuff tears and may influence later surgical therapy.
Finally, it is important to evaluate the cervical spine as well, inasmuch as many pain syndromes can derive from this area.
1.5.3 Plain X-Rays
Conventional X-rays should be carried out in all symptomatic patients. Without being able to view the rotator cuff tear itself, X-rays provide much crucial information. They can display differential diagnosis (e.g., calcifying tendinitis, severe acromioclavicular and glenohumeral joint arthritis). Moreover, they demonstrate the centering of the humeral head. An upward migration of the humeral head is a valuable diagnostic and prognostic factor in terms of rotator cuff tears. The acromiohumeral distance (AHD) is defined as the distance between the acromion and the top of the humeral head. If the AHD is smaller than 1 cm, the presence of a rotator cuff tear is indicated. An AHD greater than 7 mm implies a good prognosis for cuff repair [17]. AHD less than 5 mm indicates a poor prognosis. A cuff repair should be considered with care (Fig. 1.1).


Fig. 1.1
Plain ap-view X-ray demonstrating an upward-migrated humeral head. The acromio-humeral distance is significantly reduced (4 mm)
1.5.4 Ultrasound
Ultrasound is a noninvasive and easy accessible method for investigation of the rotator cuff. In a recent meta-analysis, ultrasonography provided good sensitivity and specificity for the assessment of partial thickness rotator cuff tears (sensitivity: 0.84; specificity: 0.89). Even higher rates could be achieved in detection of full-thickness rotator cuff tears (sensitivity: 0.96; specificity: 0.93) [18]. A limitation of the method is that the detection of fatty muscle atrophy or tendon retraction underneath the acromion is impaired by technical limitations.
1.5.5 Magnetic Resonance Imaging (MRI)
As with other joints, MRI has become a standard examination tool for investigation of the injured shoulder. In a recent meta-analysis of 44 studies with 2,710 patients, the pooled sensitivity and specificity values for the detection of partial-thickness rotator cuff tears were 0.80 (95 % confidence interval (CI): 0.79–0.84) and 0.95 (95 % CI: 0.94–0.97), respectively. The sensitivity and specificity values for the detection of full-thickness tears were 0.91 (95 % CI: 0.86–0.94) and 0.97 (95 % CI: 0.96–0.98), respectively [19]. In addition to the detection of the rotator cuff tear itself, it provides additional information such as tear size, morphology, retraction, muscle atrophy and fatty degeneration, tendon thickness, and quality [14] (Fig. 1.2).
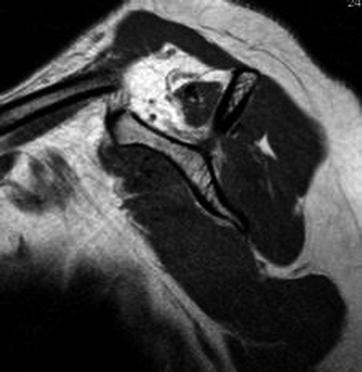
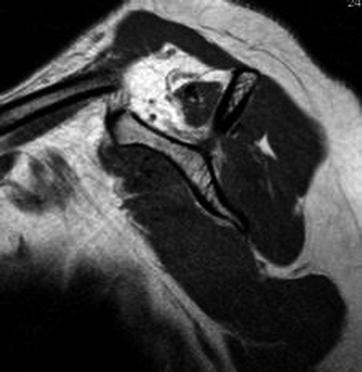
Fig. 1.2
Parasagittal sequence of MRI demonstrating a marked fatty degeneration of the supraspinatus muscle
1.6 Treatment
1.6.1 Nonoperative Treatment
1.6.1.1 Indications
All forms of asymptomatic chronic rotator cuff tears
All chronic rotator cuff tears, symptomatic <6 weeks
1.6.1.2 Treatment
Nonoperative treatment of rotator cuff tears should include anti-inflammatory medication together with subacromial injection of local anesthetics and steroids no more than twice. This treatment should be supported by physical therapy. Physical therapy should aim for maintenance or restoration of free active and passive range of motion and strengthening of the shoulder girdle.
1.6.1.3 Results
Only a few studies have reported on the outcome of nonoperative treatment of rotator cuff tears. Additionally, most of these suffer a selection bias, as the study population was asymptomatic at the time of decision-making or undesirable for operative treatment. However, Bokor et al. reported on 53 patients treated nonoperatively with rotator cuff tears [20]. After 7 years, 74 % of patients had minor or no pain and 86 % rated their result as satisfactory. Two-thirds of the patients complaining of pain less than 3 months stayed asymptomatic until follow-up. Only 56 % of patients with symptoms for longer than 6 months remained asymptomatic. Patients with moderate symptoms can be managed nonoperatively over several years without significant progression of degenerative structural joint. But there is a risk of progression from a reparable to an irreparable tear within 4 years [21].
1.6.2 Operative Treatment
1.6.2.1 General Considerations
Christian Gerber once stated that the ideal tendon repair should have high initial fixation strength, allow minimal gap formation and maintain mechanical stability until solid healing has occurred [22]. Today, several fixation techniques meet these requirements. However, depending on the shape and size of the cuff tear or stage of tendon degeneration, tears reoccur in 11–94 % [3].
Fortunately, even after a re-rupture, the majority of patients experience significant increase of the shoulder scores, predominantly as a result of a reduction in pain.
Several studies demonstrate that clinical outcome and number of re-ruptures are comparable after arthroscopic or mini-open procedures for reconstruction of supraspinatus and subscapularis tears [23–25]. Therefore, the choice of the operative procedure should depend on the surgeon’s skills. Further, there is no evidence for superiority of performing subacromial decompression at the time of rotator cuff reconstruction [26]. An evolution of fixation techniques can be seen in arthroscopic cuff repair. Single-row repair was followed by the development of double-row repair and double-row suture bridge repair techniques. In biomechanical testing, the primary stability of the double-row suture bridge technique seems to be superior in comparison to single-row fixation. They provide a higher load to failure, self-reinforcing characteristics (stronger under load), and better resistance to shear and rotational forces. In clinical studies, the double-row suture bridge repair tends to have higher outcome in shoulder scores and lower re-tear rates compared with single-row reconstruction in small and moderate tears [27–29]. However, in massive rotator-cuff tears, double-row fixation of the tendon provides significantly superior clinical and radiologic outcome [30].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








