71
Rheumatoid Arthritis: Distal Interphalangeal Joint Arthrodesis
R. John Naranja, Jr. and Kevin D. Plancher
History and Clinical Presentation
A 38-year-old right hand dominant woman previously diagnosed with rheumatoid arthritis approximately 10 years prior to the current evaluation complains of pain and deformity in the index finger of her right hand. The pain has been progressive in nature, and functionally she has been having increasing difficulty performing activities of daily living that require any type of pinch strength. She has been conservatively managed with a course of occupational therapy, splints, and medical management, without significant relief. Patient denies any associated constitutional symptoms, numbness, paresthesias, or symptoms with cervical spine range of motion.
PEARLS
- Patients with rheumatoid arthritis undergoing surgical intervention require adequate preoperative evaluation of the cervical spine.
- A preoperative neurologic examination in combination with cervical spine radiographs is crucial to avoid complications.
- The “cup-and-cone” type of configuration allows for fine-tuning of the arthrodesis position and can accommodate several fixation techniques.
PITFALLS
- Unrecognized instability of the cervical spine can result in disastrous consequences during anesthetic and operating room maneuvering.
- Complications related to deformity are usually related to surgical technique.
Physical Examination
The cervical spine range of motion is full and nontender. The posture of the index finger demonstrates a 20-degree flexion contracture with pain on attempted range of motion. Palpation of the distal interphalangeal (DIP) joint is tender with associated enlargement of the joint consistent with the presence of osteophytes. There is no evidence of erythema, drainage, or open wounds. Attempts at assessing pinch strength are associated with pain.
Diagnostic Studies
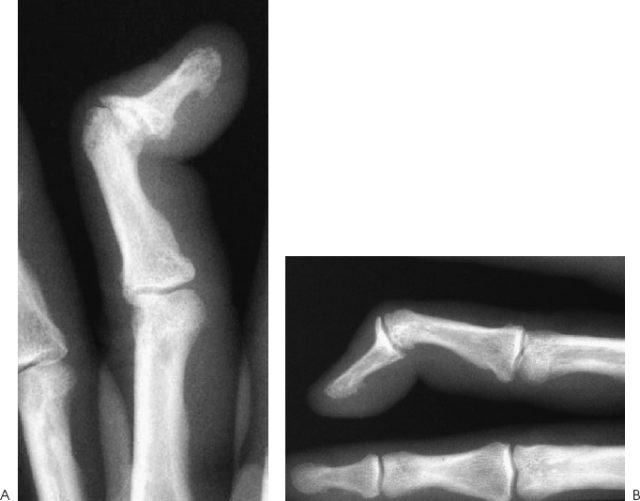
Cervical spine radiographs fail to identify potential instability. Two views of the hand demonstrate severe degenerative changes in the long finger DIP joint with joint space narrowing, sclerosis, and subcortical erosions with osteophyte formation (Fig. 71–1).
Differential Diagnosis
Degenerative joint disease
Rheumatoid arthropathy
Septic joint
Diagnosis
Degenerative Joint Disease of the Index Distal Interphalangeal Joint with Underlying Rheumatoid Arthritis
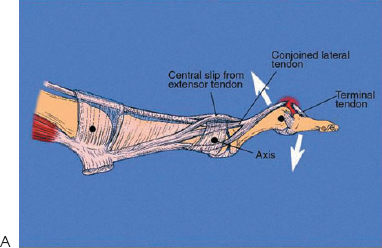
Distal interphalangeal joint disease in the rheumatoid patient encompasses a spectrum of injury patterns ranging from degenerative joint disease to inflammatory arthropathy to deformities such as the swan-neck deformity (Fig. 71–2). Frequently, coexisting conditions at the proximal interphalangeal (PIP) joint and metacarpophalangeal joint must also be addressed. Indications for surgical arthrodesis in the context of these entities typically follow a sequence of treatment alternatives that initially include nonoperative measures such as medical management, occupational therapy, and splints. This is particularly true in cases of degenerative joint disease or end stage inflammatory arthropathy. In cases where conservative measures fail, arthrodesis becomes a reasonable option. The goal of DIP joint arthrodesis is to obtain a painless, stable, and functional hand.
Figure 71–1 (A,B) Radiographs demonstrating severe degenerative changes in the long finger distal interphalangeal (DIP) joint with joint space narrowing, sclerosis, erosions, and osteophyte formation.