CHAPTER 74 Rheumatoid Arthritis
INTRODUCTION
Rheumatoid arthritis (RA) is an inflammatory disease of unknown etiology that has been known to exist since at least the 1800s,75,109 when the first detailed description was reported. Indirect evidence that it may have existed as far back as 4000 to 5000 years ago has been reported.100,102,103 Despite extensive research into its etiology and many theories about its pathogenesis, no uniform idea explains its many presentations and clinical course.17,64 In this chapter, the issue is discussed in general terms. The surgical management of the elbow is discussed in Chapters 54 and 55.
EPIDEMIOLOGY
This disease occurs worldwide and has a prevalence of about 0.5% to 2%.112 There is a female preponderance of 2 to 4 in most studies. The etiology of this disease is unknown. The presence of HLA-DR4, the gene for the major histocompatibility complex (MHC), in an increased frequency in patients with RA was a landmark observation,120 and several studies reconfirmed this and showed an increased risk of developing RA in individuals positive for the MHC class II DR-4 gene. Several studies show a strong correlation with the presence of HLA-Dw4 and Dw14 (HLA alleles DRB1*0401 and HLA-DRB1*0404).81,87 This, however, explains only a part of the genetic risk.2,52 The fact that only 1 : 20 to 1 : 35 individuals in the general white population who inherit these genes are at risk for developing RA suggests that other genetic and nongenetic factors3,86,110,133 are involved. Several investigators are currently trying to perform microsatellite mapping to identify other genes that may influence the disease. This approach has led to several likely candidates in animal studies using the rat collagen–induced model of RA.48,95 It would be of interest to see whether these can be confirmed in human studies also. Nongenetic factors that have been suggested include infections,28 pregnancy,111 and smoking,113 and others. These factors continue to be investigated.
PATHOPHYSIOLOGY
The etiology of RA is unknown. The genetic predisposition, the involvement of activated immune cells, the clonal expansion of the cells in the pathologic lesions, and the response to immunosuppressive therapy suggest that this disease is immune mediated. The observation that MHC gene HLA-DR4 was associated with RA120 directly linked the antigen-presenting cells with the immune response and suggested that antigen-induced activation was central to the pathogenesis of this disease.134 Soon, however, it was observed that other HLA-DR antigens (HLA-DR9, HLA-DR3, and HLA-Dw16) were similarly associated in different populations.66,106,138 Some of the initial differences were explained by Gregersen and colleagues’ proposal of the shared epitope hypothesis,46,87 which suggested the significance of the shared sequence in the third hypervariable region. Further studies have led to the observation that multiple genes contribute to the genetic component of susceptibility.121,135 Synovial membrane biopsies of recent-onset disease reveal inflammatory cells, including macrophages, T cells, B cells, occasionally plasma cells, and fair number of polymorphonuclear leukocytes, along with edema and increased vascular permeability. As the disease progresses, the inflammatory process intensifies, with macrophages and lymphocytes either developing into nodular aggregates or as diffuse infiltrates. Increased angiogenesis is evident. This inflammatory process progresses and starts to invade normal tissue, leading to erosions, joint space narrowing, and ultimately, destruction of the joint.
Interest in recognizing the putative antigen is high, and several candidate antigens have been and are being investigated. These include type II collagen,79 proteoglycans,60 cartilage link protein,92 Epstein-Barr virus,6 65-kDa heat shock protein,141 and Proteus mirabilis.31 Some evidence exists for each of them, and yet no one antigen explains the whole picture. This suggests that several different antigens can trigger the disease, with cross-reactivity to a self-antigen leading to a self-perpetuating autoimmune process. Local production and release of cytokines, including interleukin-1 (IL-1), tumor necrosis factor-α (TNF-α), IL-8, fibroblast growth factor (FGF), and platelet-derived growth factor (PDGF), and increased expression of intercellular adhesion molecular (ICAM) and lymphocyte function-associated molecules (LFA) and others, contribute to the enhancement of the inflammatory process.119 Of the various cytokines released, TNF-α, a proinflammatory cytokine, is thought to play a prominent role in the pathogenesis of this disease and this has led to development of various new therapeutic agents that are capable of blocking TNF (see below under treatment). B cells are activated and may be involved in antigen presentation.45 They also help plasma cells to produce increased amounts of immunoglobulins, particularly rheumatoid factors (RF). These form immune complexes, which are capable of activating the complement system, leading to enhanced local inflammation. Local release of enzymes capable of damaging the joint (e.g., stromelysin, gelatinase, collagenase) has been demonstrated. These contribute to the ongoing damage.49,143
CLINICAL FEATURES
The presentation of RA can be variable. Obviously, when patients present with a symmetric polyarthritis, the diagnosis of RA is very high on the list of possibilities. On the other hand, when patients present with systemic symptoms, the diagnosis is more uncertain. Subacute bacterial endocarditis, a paraneoplastic syndrome, malignancy,33 hepatitis C,99 or other connective tissue disease should be kept in mind. Patients have been known to present with fever of unknown origin and a clinical picture of Still’s disease, prominent fibrositis that can be mistaken for polymyalgia rheumatica, and episodic oligoarthritis (palindromic rheumatism). All of these conditions can be presenting features of RA (Box 74-1). Even when the joint symptoms are dominant, the pattern of presentation can be variable. Patients can present with a single joint swelling (21%), few swollen joints (44%), or a more typical polyarthritis (35%). The onset may be acute (days or weeks) in about half of the patients, whereas an insidious presentation is seen in the other half. About 32% of the patients present with disease of the small joint, whereas 16% present with medium-sized joints involved. Twenty-nine percent have large joints involved at onset, and 26% have a combination.36 Although the American College of Rheumatology revised the criteria for RA (Box 74-2), it is important to remember that these are for classification of groups of patients who are entered into studies and should not be used as diagnostic criteria in individual patients.8
BOX 74-2 American College of Rheumatology Classification Criteria for Rheumatoid Arthritis
The joint reacts to an insult in a limited number of ways. It is stiff, painful, tender, and swells. Loss of function may result. If the process continues, the joint sustains damage, which may lead to deformity andpermanent compromise in function. Inflammation affects all the joints in the same way, and one can observe these changes in various diarthroidal joints in the patient with RA. Stiffness that improves with use lasting more than 30 minutes is considered significant. It is thought to be due to swelling of the joint and periarticular tissues, leading to redistribution of interstitial fluid when the joint is in one position for several hours (e.g., overnight). Some of these patients also experience a generalized stiffness involving the trunk, shoulder girdles, and hip girdles. This also improves with physical activity21 but recurs with rest and inactivity. The mechanism of this systemic stiffness is not clear but correlates with the activity of disease and can be used as a measure of response to treatment.
Pain experienced by the patients is due to the ongoing inflammation. This leads to local (intra-articular) fluid accumulation and swelling of the synovial lining. Typically, the swelling observed is symmetric in a joint in contrast to the swelling seen in degenerative osteoarthritis, which is asymmetric. The cause of predominant bilateral symmetry is not known, but local innervation and release of inflammatory neuropeptides have been suggested as factors.61,90,105 The presence of synovial swelling and synovial fluid is characteristic evidence of inflammation in the joint, as pain and decreased function can be present owing to extra-articular disease. Motion must contribute to the damage, since joints spared from this are spared by the disease.14,44,124 The diarthrodial joints of the thoracic and lumber spine are very rarely involved, and motion may play a role in this also.96,115
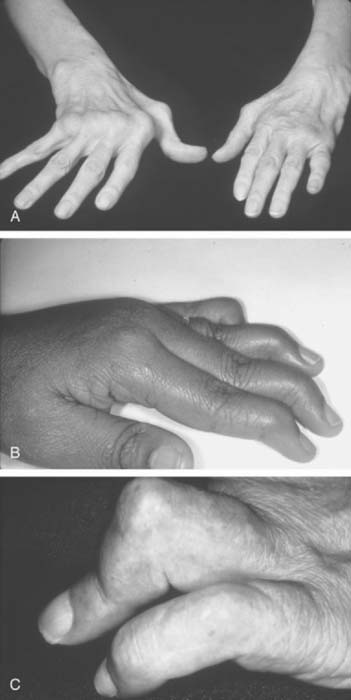
The inflammation in RA goes through intermittent exacerbations and remissions. This cycle leads to stretching and damage of the joint capsule and ligaments. Disuse and inflammation lead to weakness of the supporting muscles.108,123 These factors, and recurring mechanical forces that change as the stability of the supporting tissues is compromised, lead to development of deformities that gradually increase with time (Figs. 74-1 and 74-2).
The hands and wrist are the most common joints involved in this disease and cause the most disability. Elbow involvement has been reported in 20% to 65% of patients with RA. The earliest change noted in the elbow is loss of extension. In most cases, this occurs imperceptibly, because the patient has involvement of the hands and wrist at the same time, and these deformities are usually more disabling. Loss of the groove on either side of the olecranon is usually good evidence of elbow involvement.91 Disease progression is similar to that with other joints; occasionally, large cystic swellings can occur (Fig. 74-3).
EXTRA-ARTICULAR MANIFESTATIONS
Rheumatoid Nodules
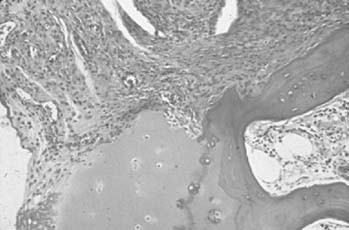
Nodules occur in about 20% of patients with progressive seropositive disease. These nodules are most commonly subcutaneous and occur along the extensor surfaces of the arms, elbows, olecranon bursae, spine, occiput (Fig. 74-4), and other areas exposed to mechanical pressure. They can be very small, for example, ranging from less than 1.00 mm in size to several centimeters in diameter. The latter usually are collections of many nodules occurring together. These nodules have a very characteristic histology in that they are made up of a central area of fibrinoid necrosis surrounded by an area of palisading epithelial cells and fibrocytes. Surrounding this is an area of lymphocytes, plasma cells, and fibrocytes tissue. Detailed study of the early lesion suggests small vessel vasculitis as the initiating event,118 with deposition of immune complexes,88 and localization of HLA-DR-positive cells.9 These nodules can be observed in tendon sheaths, heart, lungs, liver, eyes, and the meninges.54 The presence of multiple nodules should alert the physician to the presence of vasculitis, and ulcerated nodules can be a source of bacteremia.
Hematologic Manifestations
Anemia is a very common presentation of RA. The prevalence depends on the stage and duration of disease, and the severity on disease activity. The cause of the anemia is multifactorial, resulting from several factors, including subclinical hemolysis, chronic blood loss as a side effect of prolonged use of nonsteroidal anti-inflammatory drugs (NSAIDs). The most common cause of the anemia is poor iron utilization from stores in the reticuloendothelial system and reduced erythropoietin levels. The increased production of proinflammatory cytokines in the bone marrow contributes to the anemia of chronic disease.53,69 The anemia is usually normocytic normochromic, although the picture can change depending on other complicating factors. Usually, these patients are not iron deficient, unless they have significant blood loss, and it is not always easy to distinguish between these conditions.77 When these patients schedule surgery, they may not be able to donate autologous blood for use during surgery. Recent experience with the use of synthetic erythropoietin suggests that this may be an option for some selected patients.70,71 This needs more study, because there are patients who may not respond to synthetic erythropoietin.10
Usually, the white blood cells are normal in these patients; however, about 1% of patients with RA develop a neutropenia, and splenomegaly. These patients do have an increased risk of bacterial infections and skin ulcerations. Therapy with agents used to treat RA (e.g., intramuscular gold, d-penicillamine, corticosteroids, and methotrexate) have been successful, although recently, granulocyte-macrophage colony-stimulating factor (GM-CSF) has also been used in small numbers of patients.13,32,63 Surgery should be avoided until the granulocytopenia has resolved. Splenectomy may help, but usually for that episode only, and is best avoided unless a life-threatening situation exists.97
Pulmonary Involvement
Pulmonary involvement in this disease is very common, with many patients with this condition being unrecognized and found to have involvement only at autopsy. In most cases, pleural involvement is asymptomatic and may be noted on incidental chest radiographs taken for other reasons (Fig. 74-5). The effusions may require aspiration, mostly for diagnostic reasons. These effusions are exudates with increased cells, protein, and lactate dehydrogenase (LDH). Complement levels are low, and characteristically these patients have very low glucose in the effusion compared with the concomitant blood glucose. These effusions resolve with treatment of the systemic disease, leaving behind fibrosed pleura.
Rheumatoid nodules occur in the lungs in patients who are RF positive and have subcutaneous nodules. These can be single or multiple, unilateral or bilateral, or small or large. The nodules can be particularly large in patients with pneumoconiosis. Malignancy is always a consideration when a new nodule appears in the setting of a stable pulmonary picture. Without a biopsy, this possibility cannot be ruled out.127
Lungs are involved in RA patients in many different ways, although clinically, the patients may present with radiographic changes before symptoms develop. Interstitial fibrosis usually affecting the bases and spreading to the other areas of the lungs can be observed. The clinical picture is similar to that in idiopathic pulmonary fibrosis or the picture of interstitial fibrosis seen in connective tissue diseases. Although as many as 50% of RA patients may develop interstitial disease, only 5% are symptomatic. Pulmonary function tests and high-resolution computed tomography can aid in the recognition of small airway disease.30,43,51,68,144 Smoking has been found to be a risk factor for developing interstitial lung disease.104
Cardiac Conditions
Pericarditis, similar to pleuritis, can be found in almost 50% of the patients with RA at autopsy. The patients may be asymptomatic or may have moderate to large effusions. Fluid removed shows characteristics similar to those of pleural effusions; that is, they are exudates with increased cell counts, increased protein, LDH, low complement levels, and low glucose. Some patients present with pericardial tamponade that requires emergency aspiration or surgery. Recurrent episodes with resulting fibrosis lead to the development of constrictive pericarditis. Pericardiectomy, pericardial window, or repeated pericardial aspirations can be life-saving; without these, the mortality rates are very high.56,126
Myocarditis and endocarditis can occur in RA patients. Myocarditis is usually found at biopsy or autopsy, and rarely does it lead to congestive heart failure. More often, it presents with cardiac conduction abnormalities, as does the presence of rheumatoid nodules when localized to the conduction system, leading to first-degree, second-degree, and in some patients, third-degree heart block. Rheumatoid nodules involving the valves have been reported.16,23 Coronary vasculitis has been observed in rare cases.
Vasculitis
Necrotizing vasculitis of the medium-sized vessels occurs in patients who have progressive uncontrolled disease. These patients have polyarticular, nodular, erosive disease, with fever, recurrent pericarditis, cutaneous ulcerations, scleritis, and digital infarcts (Figs. 74-6 and 74-7). Laboratory studies show that these patients are anemic, and have leukocytosis, eosinophilia, and high titers of RF. The manifestations of vasculitis depend on the organ system involved. Cutaneous infarcts, ulcerations, neuropathy, bowel infarcts, digital infarcts, and, gangrene of the gallbladder, brain, heart, and peripheral nerves all can be observed.67,82 These patients are not good candidates for surgery, and it is best to delay any surgical procedures.
LABORATORY STUDIES
Laboratory studies are done to aid in diagnosis, monitor the progress and complications of disease, and assess the side effects of drugs. These tests include measuring hemoglobin, white blood cell count, differential white blood cell counts, platelet counts, erythrocyte sedimentation rate, rheumatoid factor, anticyclic citrullinatedpeptide antibody, antinuclear antibodies, liver enzymes, and renal function. Special circumstances may require specific tests, depending on the patient’s condition. Radiologic changes (Fig. 74-8) are an important measure of disease progression, and plain radiographs and magnetic resonance imaging are necessary.50 Although RF tests are positive in about 80% of patients with RA, 20% of patients with this disease are rheumatoid factor negative. Anti-IgG antibodies can also be seen in several other connective tissue diseases, with infections and malignancies, and in other states (Box 74-3); thus, one needs to interpret the results with some caution.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree