72
Rheumatoid Arthritis: Proximal Interphalangeal Joint Arthrodesis
R. John Naranja, Jr. and Kevin D. Plancher
History and Clinical Presentation
A 50-year-old right hand dominant man was originally diagnosed with rheumatoid arthritis 16 years ago. Medical management of his disease process has included chronic oral prednisone. His primary complaint includes pain and deformity of his hands and decreased function secondary to lack of mobility and strength.
Physical Examination
The patient has ∼ 25 degrees of ulnar drift at the index through small finger metacarpophalangeal (MP) joints. An extension deficit at the MP measures ∼ 45 degrees. The arc of motion of the digits at the MP is 20 degrees. The proximal interphalangeal (PIP) joint of the index and long fingers demonstrates a 30-degree flexion contracture with pain and crepitus with range of motion. Key pinch strength is 30 N and grip strength is 70 N at position II using the Jamar dynamometer.
PEARLS
- The position of the joint fusion should allow for the best function, which includes grasp function and the ability to put on a glove.
- The goal of the procedure is to provide complete pain relief and maximize function.
- Fixation can be assessed with intraoperative radiographs.
PITFALLS
- Bone quality and soft tissue coverage may be a technical limitation that may not be assessed until surgery and may alter the treatment plan.
- The number of passes of the K wires through bone and soft tissue should be limited.
- Stretching of the skin by K wires should be avoided.
Diagnostic Studies
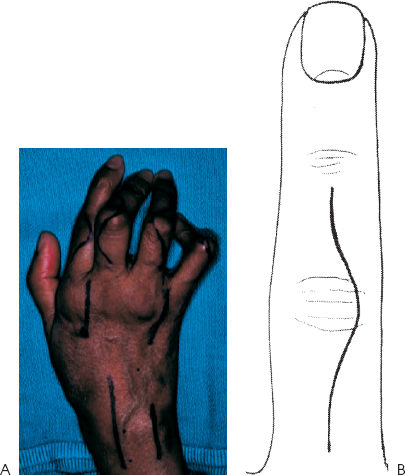
Radiographs, including posteroanterior (PA) (Fig. 72–1), lateral, and oblique views, demonstrated degenerative changes with associated subluxation at the MP joints and the PIP joints.
Differential Diagnosis
Degenerative joint disease
Rheumatoid arthritis
Septic joint
Diagnosis
Rheumatoid destruction and deformity of the index through small finger MP joints with associated severe degenerative arthritis of the PIP joints of the index and long fingers
Surgical Management
As initial conservative management has failed and the patient is having progressive disability secondary to the pain, operative options were discussed. In this situation, fusion of the PIP joint can provide good pain relief with maintenance of sufficient function in the context of MP joint arthroplasty.
Figure 72–1 Posteroanterior (PA) radiographs of degenerative changes in the index proximal interphalangeal (PIP) and associated subluxation of the metacarpophalangeal joint.
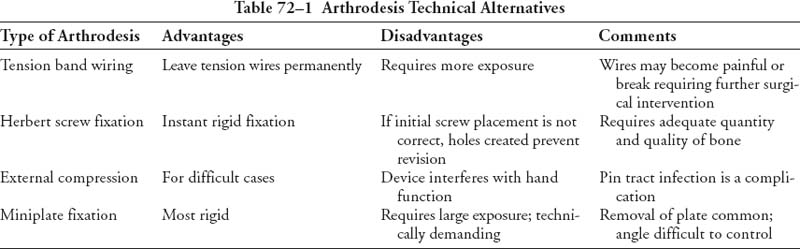
Several techniques have been described for arthrodesis of the PIP joint (Table 72–1). These include Kirschner wires (K wires), tension band wiring, intraosseous wiring, screw fixation, compression devices, and miniplates. Bone quality may limit the choices of treatment. The technique of choice should limit the rate of nonunion and provide a low complication rate.
Indications for PIP joint arthrodesis include pain relief, improved stability and deformity, and prevention of disease progression. In cases of finger deformity due to deficient tendon function, arthrodesis is preferred. Arthrodesis also provides alignment correction in addition to joint stabilization. In addition to bone quality, soft tissue coverage must also be adequate for successful arthrodesis.