Fig. 13.1.
Preoperative AP (a), lateral (b), and Merchant view (c) radiographs demonstrating component positioning after index TKA procedure.
13.3 Diagnosis/Assessment
13.3.1 History
The evaluation of ligamentous instability after total knee arthroplasty continues to be challenging, particularly in cases when radiographic and/or physical exam findings are not inherently obvious. As always, a detailed history both before and after the index procedure is vital. Patients with subtle instability patterns complain of catching, giving way, or anterior knee pain. Anterior knee pain often occurs as the patient tries to stabilize their knee by firing the quadriceps muscle on a chronic basis. While not always available, preoperative radiographs, exam findings, and indication for the initial procedure can be helpful in these circumstances. Important considerations also include type of implant, a detailed postoperative course including physical therapy reports, pain chronology, operative technique including ligamentous releases, and pertinent patient factors including history of neuromuscular or connective tissue disease [2, 3]. Additional risk factors that have been described include obesity as well as planovalgus foot deformities [3]. Other historical clues in subtle cases include recurrent effusion, difficulty with ascending/descending stairs, soft tissue tenderness, and anterior knee pain [4]. Implant migration and failure, neuromotor dysfunction, and extensor mechanism failure are other potential rare causes of global instability. Symptoms include giving way, recurvatum, and poor quad function.
13.3.2 Physical Exam
While physical exam findings such as varus or valgus thrust during gait or gross sagittal subluxation on exam may be easier to detect, subtle findings may be more difficult to identify, particularly if the patient is guarding [5]. In full extension the knee may feel stable to varus and valgus stress; however a tight posterior capsule can act as a coronal stabilizer. The knee should also be examined at 30° to isolate the collateral ligaments and at 90° to assess anterior-posterior translation. This is best done with the patient sitting over the edge of the bed with the knee hanging from the table. Patellar tracking abnormalities should also be noted as these can be suggestive of component malrotation.
13.3.3 Radiographs
Careful radiographic analysis can also help identify potential contributing factors. If initial preoperative radiographs are available, they should be examined for significant mechanical axis abnormalities and anatomic deformity as well as increased posterior condylar offset that may have been resected during surgery. Postoperative radiographs including AP, lateral, merchant, and 3 ft standing views should be examined for joint space asymmetry, polyethylene insert size, implant-bone over or undercoverage, patellar tilt, and mechanical axis correction. Stress views are also helpful in delineating varus-valgus instability (AP view) or anterior/posterior instability (lateral view).
13.3.4 Other Tests
Infection should be ruled out in this patient population, oftentimes presenting pain, warmth, and recurrent effusions. It is not unusual that numerous aspirations of the joint due to recurrent effusions have been performed. Multiple aseptic aspirations of recurrent bloody effusions should be an additional clinical insight into possible ligamentous instability etiology of the patient’s complaints [6]. Routine inflammatory markers should be assessed in conjunction with aspiration results. If there is suspicion for component malrotation resulting in ligamentous instability, CT scans have been shown to be helpful to identify such abnormalities; however the intra- and interobserver reliability has been variable [7]. CT scan should include the hip joint to assess rotational alignment of the implant in relation to the femoral axis. Full-length standing films can also help diagnose mechanical alignment abnormalities or unrecognized femoral or tibial deformities at the index procedure that may have led to incorrect implant positioning.
13.4 Management
After consideration of both clinical history and physical exam at presentation, a working diagnosis of medial flexion coronal instability in flexion and AP flexion instability (sagittal) was made. Preoperative planning included insurance of implant availability which included constrained components with associated augments compatible with the current implant. Canal reamers and appropriate equipment for component removal including a microsagittal saw, osteotomes, and an available burr were also available.
The previous midline incision was used and extended proximally into native tissue to establish a recognizable tissue dissection plane. A midline parapatellar arthrotomy was carried out and the joint fluid that was encountered was sent for culture. Tissue specimens that were taken from multiple sites and sent to pathology returned intraoperatively with <5 PMNs per high power field in all samples. Intra-articular scar formation was meticulously excised from the medial and lateral gutters and the patellar inversion technique [8] was used for exposure. This technique is our preferred initial exposure and has been shown to provide adequate exposure in >95 % of cases in one study of 420 knee revisions. This involves early lateral retinacular release followed by subperiosteal elevation of the medial ligamentous sleeve while gradually externally rotating the tibia, extending to the posteromedial corner. The rotating platform polyethylene insert was removed with an osteotome after anterior dislocation of the tibia and was inspected for asymmetric as well as backside wear. Attention was then turned to the tibial component which was well fixed and noted to be in appropriate external rotation with regard to the tibial tubercle. At this point the flexion and extension gaps were examined with a tensioning device. The extension gaps were noted to be symmetric; however the flexion gap revealed excessive lateral opening upon tensioning (Fig. 13.2). Based on the tibial component, which was measured to be neutral to the mechanical/anatomic axis of the tibia, the femoral component was noted to be in approximately 8° of internal rotation while under tension (Fig. 13.3). At this point the decision was made to proceed with femoral revision.
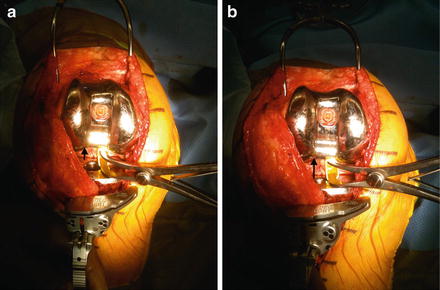
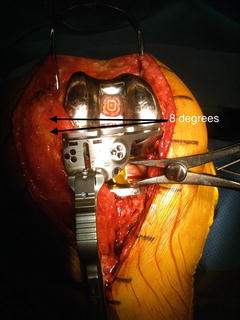
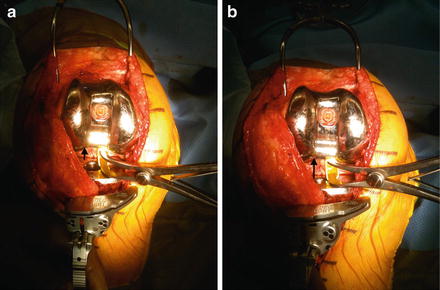
Fig. 13.2.
Intraoperative demonstration of ligamentous instability with (a) having no tension followed by (b) exhibiting lateral opening upon tensioning of the medial and lateral soft tissues.
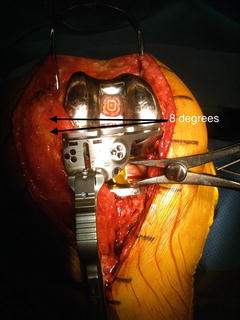
Fig. 13.3.
Intraoperative demonstration of improper rotational alignment of the femoral component with internal rotation of approximately 8°.
A microsagittal saw was used to disrupt the implant-cement interface in order to conserve as much native bone as possible. A combination of a thin ¼ inch osteotome and the microsagittal saw was used at the chamfer cuts and the distal femur followed by disimpaction of the femur with relatively minimal bone loss. The femoral canal was then reamed sequentially and a 5° distal femoral cut was carried out. At this point a 4 in 1 cutting guide was placed and rotation was set based on the epicondyles and our flexion gap. We noted bone loss both posteriorly and distally and determined the need for corresponding augments to maximize bone-implant contact. Larger augments were placed posterolaterally in order to increase external rotation of the femoral component. The flexion and extension gaps were noted to be equal, eliminating the need to posteriorize the femur and a 12.5 mm polyethylene trial was inserted. The knee was stressed at 0, 30, and 90° and deemed stable both in the coronal and sagittal planes. There was noted to be less than 5 mm anterior-posterior shuck at 90° of flexion and there was no gapping with varus/valgus stress in full extension. The synovial scar tissue surrounding the patella was completely debrided and there was no significant wear noted. An osteotome was placed between the bone-implant interface and there was no loosening noted. At 90° of flexion there was mild residual lateral tilt noted and a lateral release was performed, after which the patella tracked well with a no thumbs technique. Antibiotic impregnated cement was mixed on the back table and the femoral implant was cemented in place using a third generation cementing technique. The trial polyethylene was placed and axial pressure was placed on the leg until the cement was dry. The flexion and extension gaps were once again verified and a 12.5 mm polyethylene was seated. Two medium Hemovac drains were placed and the arthrotomy was closed followed by skin closure.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








