Fig. 3.1.
Lateral picture of the patient’s right knee after surgical prep depicting 20° flexion contracture.
Weight-bearing AP, lateral, and sunrise radiographs of the patient’s right knee showed advanced joint space narrowing, subchondral sclerosis, and abundant osteophyte formation, all consistent with a diagnosis of osteoarthritis (Fig. 3.2). As the patient had previously undergone exhaustive nonsurgical treatment and was substantially limited by his pain and stiffness, he was interested in pursuing total knee arthroplasty surgery.


Fig. 3.2.
Preoperative standing AP, lateral, and sunrise views. (a) Standing AP radiograph showing joint space obliteration, peripheral osteophytosis, and medial tibial bone loss. (b) Lateral radiograph showing substantial patellar and posterior femoral osteophyte formation, along with posterior translation of the femur on the tibia. (c) Sunrise radiographs showing patellofemoral osteoarthritis with severe peripheral patellar osteophytosis, but appropriate patellar tracking.
3.2 Diagnosis/Assessment
The patient’s history, physical and radiographic findings are consistent with the diagnosis of advanced osteoarthritis with a fixed varus deformity and flexion contracture. While the presence of coronal plane deformity is common in most knees requiring total knee arthroplasty, the presence of substantial (greater than 15°) flexion contractures is not as common and deserves special consideration for operative planning. Such flexion contractures need to be addressed during TKA surgery to ensure optimal postoperative range of motion, normal gait mechanics, and good patient satisfaction.
In general, flexion contractures during TKA surgery can be managed by utilizing one or a combination of the following techniques: (1) Coronal plane balancing with collateral ligament releases as needed; (2) Complete resection of posterior osteophytes and subsequent posterior capsular releasing as needed; (3) Resection of additional distal femoral bone; and (4) Hamstring muscle tenotomy. While many of these techniques are used in combination with one another, each case must be taken on an individual basis, as subtle radiographic and physical examination findings can help direct the surgeon through the ideal sequence of releases and bone resection that result and a well-balanced fully extended knee.
3.3 Management
An initial medial parapatellar arthrotomy was performed for exposure, with severe osteoarthritic findings being confirmed upon inspection of the joint (Fig. 3.3). The extensive patellar osteophytes were resected to help enhance patellar mobilization, and an extramedullary guide was used to resect approximately 10 mm of tibial bone referencing the more intact lateral tibial plateau (Fig. 3.4). A distal femoral resection of 10 mm was performed (standard resection is 8 mm) (Fig. 3.5), and the knee balance was assessed in full extension (Fig. 3.6a). A 9 mm equivalent spacer block (minimal composite implant/polyethylene thickness) was inserted which revealed tight medial space (Fig. 3.6b), and relative lateral laxity that would accommodate a 13 mm equivalent polyethylene (Fig. 3.6c).
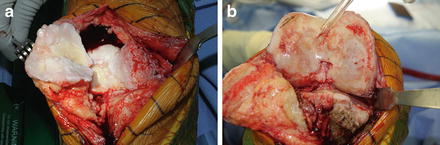



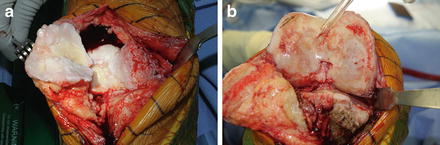
Fig. 3.3.
Intraoperative photos. (a) Intraoperative photo showing hyper-osteophytic knee with extensive peripatellar, tibial, and femoral osteophytes. (b) After resection of patellar osteophytes the patella was everted, the knee flexed, and the remainder of the joint exposed. Posterior medial tibial bone loss is evident and consistent with the patient’s preoperative clinical findings of fixed varus deformity.

Fig. 3.4.
Intraoperative photograph after tibial resection of 10 mm referencing the intact lateral plateau using an extramedullary tibial guide.

Fig. 3.5.
Intraoperative photograph showing initial distal femoral resection of 10 mm, which is 2 mm greater than the thickness of implant on distal femur (8 mm).

Fig. 3.6.




Intraoperative assessment of extension space with spacer block. (a) Full extension was achieved with the minimal thickness spacer block, which represents the composite thickness of the implants and the smallest 9 mm polyethylene insert. (b) In extension, the knee was tight medially with no gapping when a valgus force was applied. (c) The lateral compartment, however, was loose and would eventually require a thicker polyethylene to accommodate the laxity in this location.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








