Fig. 12.1.
(a–d) Preoperative X-rays reveal a cemented right and left total knee arthroplasties with radiographic signs of loosening. The right TKA tibial component has subsided into varus.
12.1.1 Diagnosis/Assessment
The patient presented with a chronically painful right TKA and late instability in the setting of elevated serum metal ion levels, and hence was presumed to have full-thickness polyethylene wear and resultant osteolysis. The index of suspicion for this was high on the left knee as well, but our work-up and treatment focused on his symptomatic right TKA. Chronic, indolent periprosthetic infection could not be ruled out either, but his history, physical exam, and laboratory results suggested an aseptic etiology; hence, a preoperative knee aspiration for synovial analysis was deferred in lieu of an intraoperative assessment. Historically, polyethylene wear and its sequelae (aseptic loosening, osteolysis, late instability) are common causes for revision total knee arthroplasty, particularly with the use of modular tibial components. In fact, osteolysis induced by wear debris of ultra-high-molecular-weight polyethylene emerged as a significant problem, presumably related to backside polyethylene wear as well as poor quality polyethylene (i.e., gamma irradiated in air). While a rare cause of failure after total knee arthroplasty, metallosis was also considered in this case given the significant osteolysis, joint space narrowing, and radiographic densification of the periarticular soft tissue seen radiographically [2]. Metallosis has only previously been reported when there has been abnormal metal-on-metal contact, and we suspected this phenomenon here, prompting our preoperative interest in serum metal ion levels.
12.1.2 Management
In a patient with presumed metallosis, osteolysis, and aseptic loosening due to full-thickness polyethylene wear, revision TKA involving all components must be discussed. In particular, the method of reconstruction depends on the remaining bone stock, ligamentous integrity, and the ability to balance flexion/extension gaps. The Anderson Orthopedic Research Institute (AORI) classification grades bone loss associated with revision TKA based on defect size and the degree of metaphyseal involvement [3]. This provides a useful guide for predicting the options for reconstruction. Cement, morselized allograft, or metal augments can be individually used to fill smaller, confined defects (<1 cm). As the defect size or degree of metaphyseal involvement increases, reconstruction may require impaction grafting, structural allograft, metaphyseal sleeves, porous metal cones, composite allograft, megaprostheses, or some combination of any of these modalities (Fig. 12.2). While preoperative radiographs can predict the anticipated bone loss, they often underestimate the actual bone loss encountered intraoperatively [4]. Hence, adequate preoperative planning means anticipating the use of any combination of the aforementioned defect-filling modalities.
Fig. 12.2.
Matrix of bone loss filling options in revision TKA. X-axis represents the relative defect size, while the y-axis represents the defect type, according to the Anderson Orthopedic Research Institute (AORI) classification.
12.1.3 Outcome
The patient underwent elective revision TKA after thorough discussion about the potential bone loss and the spectrum of possible treatment options; while less likely, the potentials for underlying periprosthetic infection and two-stage revision were also discussed. At the time of surgery, there was extensive metallosis and metallic debris, but intraoperative frozen sections were unremarkable for acute inflammation. On gross examination, the all-polyethylene patellar button was frankly loose, and there was significant femoral component burnishing. There was full-thickness wear of the polyethylene insert, most prominently on the posterolateral corner, and a corresponding completely worn corner of the tibial base plate beneath it (Fig. 12.3). Removal of all hardware revealed significant osteolysis of both the distal femur and proximal tibia with type III bone defects, as classified by the AORI scale. On the femoral side, only a shell of bone remained medially, with a significant osteolytic defect on the lateral side as well (Fig. 12.4a). On the tibial side, there was a significant osteolytic defect centrally (Fig. 12.4b). The femoral defect was filled with a trabecular metal distal femoral cone and a press-fit stem, along with bilateral distal femoral and posterior augments (Fig. 12.5a). Likewise, the tibial defect was addressed with a trabecular metal cone with a press-fit stem and bilateral tibial augments (Fig. 12.5b). A total stabilized insert was used to address ligamentous instability. Postoperatively, the patient was restricted to 20 lbs-weight bearing for 6 weeks in a hinged knee brace, locked from 0° to 90°. At his 8-week postoperative follow-up visit, he was already weight bearing as tolerated without a brace and demonstrated an active range of motion from 0° to 130°. He did complain of some new-onset, mid-shaft tibial pain, which was mild in nature and unrelated to any injury or other symptoms. His radiographs demonstrated stemmed femoral and tibial components in good overall alignment (Fig. 12.6). There was no evidence of fracture or loosening, and we attributed this pain to modulus mismatch with the press-fit tibial stem.
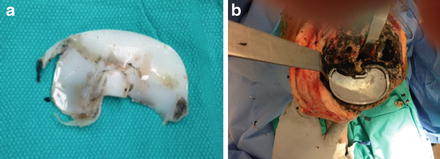
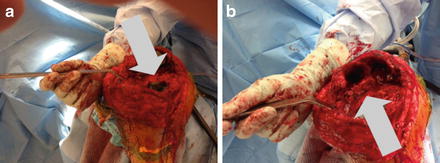


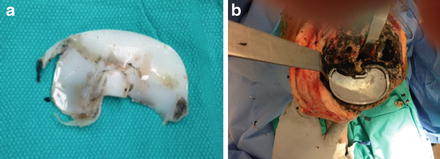
Fig. 12.3.
There is full-thickness wear of the polyethylene insert, most prominently on the posterolateral corner (a), and a corresponding completely worn corner of the tibial base plate beneath it (b).
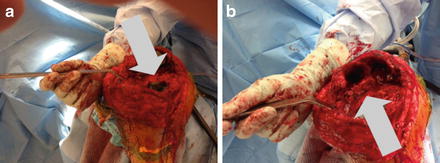
Fig. 12.4.
In the femur, there is only a shell of bone remaining on the medial side and a significant osteolytic defect laterally (a). There is a significant osteolytic defect centrally seen in the tibia (b).

Fig. 12.5.
Trabecular metal cones are seen filling defects in the distal femur (a) and proximal tibia (b).

Fig. 12.6.




Postoperative week 8 AP (a) and lateral (b) radiographs demonstrate stemmed femoral and tibial components in good overall alignment.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








