Revision Procedures and Complex Articular Cartilage Surgery
Brian J. Cole
Robert C. Grumet
Nicole A. Friel
The management of traumatic and degenerative articular cartilage injuries is a known challenge given the lack of a pluripotent cell line and poor vascularity, resulting in limited capacity for healing. The surgical management of these cartilage lesions may be further complicated by injuries, which include large and/or deep, multiple lesions, or patients with associated pathology, which may have contributed to failure of previous surgeries. These comorbid conditions may include ligamentous instability, malalignment, and meniscal deficiencies. The appropriate management of a patient with a revision or complex articular cartilage lesion requires a stepwise approach on a case-by-case basis with careful attention to patient and lesion-specific variables and the patient’s expectations for postoperative outcome.
CLINICAL EVALUATION
History
Chondral lesions are often difficult to diagnose due to their variable presentation. Most often, acute injuries to the cartilage are caused by direct trauma with articular cartilage impact or involve a twisting or shearing movement associated with axial loading. This mechanism of injury often causes an injury to the surrounding soft tissues and capsuloligamentous structures. For example, condylar lesions may result from an acute or chronic anterior cruciate ligament (ACL) deficiency. Similarly, trochlear or patellar cartilage lesions may result from patellar instability.
A thorough history should include a discussion of the patient’s pain, swelling, and instability or mechanical symptoms. Pain is the most often the patient’s primary complaint. Pain is usually described at the associated compartment; ipsilateral medial or lateral joint line for condylar injury and anterior for trochlear or patellar lesions. Chondral lesions may be aggravated by certain positions or activities, such as weight-bearing activities for femoral condyle lesions and climbing stairs or squatting for patellofemoral lesions. An effusion usually accompanies the pain in the same location and is noted during activity. Possible concomitant injury to other soft tissue structures of the knee joint requires careful questioning regarding knee stability or meniscal symptoms. Meniscal pain can often be difficult to discern from pain due to an articular cartilage lesion. In this case, a history of previous meniscectomy can help guide the surgeon toward the possibility of meniscal deficiency as a cause for continued pain and disability.
Prior attempts at treatment should be reviewed with the patient. Previous knee surgeries should be discussed, including the type of surgery, when the surgery took place, the type of rehabilitation followed and whether postoperative symptomatic relief occurred initially with subsequent recurrence of symptoms or not at all following the prior intervention. Nonsurgical management, such as oral medications, injections, bracing, physical therapy, and lifestyle modification, should also be discussed as an important part of the patient’s prior treatment.
Physical Exam
Observation of body habitus and the patient’s gait is an important aspect of the physical examination. An antalgic gait as well as evidence of malalignment with a valgus or varus thrust should be noted. Inspection of the lower extremity should include visualization of incisions from previous surgeries, as well as assessment of quadriceps circumference. An effusion can often be appreciated as fullness in the suprapatellar pouch at the anterolateral joint line with knee flexion.
Palpation of the knee joint elicits pain in the involved compartment. Patients with chondral injuries of the condyles often have joint line tenderness at the ipsilateral side of the knee. Meniscal injury also presents as pain at the joint line, but this pain is often more posterior than pain due to chondral injury. Patellofemoral lesions are usually associated with anterior pain and crepitation. Patellar tilt and glide should be assessed to evaluate for tightness of the lateral retinaculum and potential patellar instability.
Range of motion should be evaluated in both knees. Normally patients have full extension to a few degrees of hyperextension. Any evidence of a flexion contracture in
the affected extremity should be noted as it is associated with a poor environment for postoperative rehabilitation.
the affected extremity should be noted as it is associated with a poor environment for postoperative rehabilitation.
Identification of associated pathology is critical to the successful outcome of revision and complex articular cartilage restoration. Persistent instability, malalignment, or meniscal deficiency is often a cause of premature failure of articular cartilage repairs and poor outcomes. Stability of the ACL, posterior cruciate ligament (PCL), medial collateral ligament (MCL) as well as lateral collateral ligament (LCL) and posterolateral complex (PLC) should be a routine part of any knee examination. Notably, a rotational component can be accentuated in the setting of meniscal deficiency.
Imaging
Standard radiographs for cartilage injury include bilateral knees, AP weight bearing, nonweight bearing 45° flexion lateral, and an axial (Merchant) view of the patellofemoral joint. Additional views include 45° flexion posteroanterior(PA) to identify subtle joint space narrowing that may be missed in an extension view and longleg alignment view to assess the mechanical axis. In the case of patellar instability, a CT scan may be helpful to further assess the patellofemoral joint and associated tibal tubercle- trochlear groove (TT-TG) distance (1, 2). An MRI is useful to characterize the size, depth, and location of the cartilage lesion, the quality of subchondral bone or the presence of bony fractures, and associated pathology to ligaments, menisci, and other soft tissues.
Documentation of Previous Procedures
Patient’s that have undergone previous knee procedures should be asked about the details of the chondral lesion and procedure. Documentation, including the operative report, intraoperative photographs, and pre- and postoperative clinic notes, are all important in determining the most appropriate treatment options for the patient.
TREATMENT
Goals
Expectations should always be reviewed with the patient, especially with complex or revision procedures that may not completely resolve the patient’s pain and/or totally restore functional level. Overall, the treatment goals for cartilage restoration are reduction of symptoms, improvement in joint congruency, elimination of instability, and protection of the cartilage repair.
Treatment Options and Decision Making
Several options are available for treatment of cartilage lesions, depending upon the location, size, depth, geometry, and containment of the lesion. In addition, each patient should be considered on a case-by-case basis as age, activity level, response to prior therapies, and comorbidities such as malalignment, instability, and meniscal deficiency weigh heavily in the decision-making process.
Nonoperative Treatment
Despite the complexity of the cartilage injury, all nonoperative options should be fully explored before surgery. Indications for nonoperative treatment include asymptomatic lesions and small, incidental lesions. Several modalities are used to treat these lesions. Oral glucosamine and chondroitin supplementation may reduce knee pain. Acetaminophen, nonsteroidal anti-inflammatory drugs(NSAID) (including selective cyclooxygenase-2 inhibitors), and intra-articular steroid or viscosupplementation injections are also used to reduce symptoms. Physical therapy is another modality to rehabilitate a patient according to their functional activity goals and it must include a comprehensive proximal core-strengthening program in addition to traditional distal strengthening.
Operative Treatment
The surgical management of articular cartilage lesions can be grouped into three categories. Palliative procedures include arthroscopic debridement and lavage to provide symptomatic relief to the patient with little potential for cartilage regeneration. Reparative procedures include marrow-stimulation techniques, which create a pluripotent fibrin clot, ultimately resulting in fibrocartilage replacement. Finally, restorative procedures attempt to restore the natural hyaline surface of articular cartilage through the use of cultured chondrocytes or osteochondral grafts. These procedures may be considered as part of an algorithm for the management of focal cartilage defects from least invasive to more invasive. The goal of surgery is to restore the patient’s function and ameliorate the patient’s symptoms with the least invasive method possible. In the setting of revision or complex articular cartilage surgery, many patients have had a simple microfracture or debridement and the surgeon may need to consider more aggressive management to achieve their goals.
Lesion and patient-specific factors are important determinants of the type of procedure indicated. Lesionspecific variables include size, depth, geometry, and bone quality. Patient specific variables include the patient’s physiologic age, activity level, and previous surgeries.
Perhaps the most important consideration in the setting of revision and complex articular cartilage restoration is a firm understanding of the reason for failure. There is often a comorbid condition such as malalignment, instability, or meniscal deficiency, which has either failed to protect a previous attempt at cartilage restoration or led to premature degradation of the replacement tissue. In addition, the patient’s expectations after the prior surgery must be discussed as a potential cause for dissatisfaction or failure. The timing of return to sport, interval symptom relief after return, change in the character or nature of the symptoms, and the patient’s future activity level and goals should be discussed as well. A thorough preoperative examination should include a standing-limb-alignment radiograph and oftentimes a diagnostic arthroscopy to evaluate the integrity of the
cartilage lesion and potential concomitant pathology such as meniscal or ligamentous deficiency in an effort to appropriately plan or stage the necessary corrective procedures.
cartilage lesion and potential concomitant pathology such as meniscal or ligamentous deficiency in an effort to appropriately plan or stage the necessary corrective procedures.
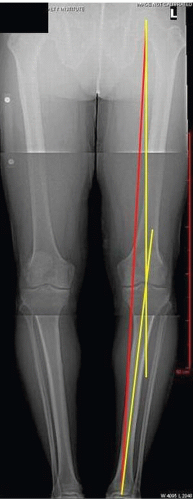
INDICATION
The indication for revision or complex articular cartilage restoration is a symptomatic focal cartilage defect, which has failed to improve with conservative measures or previous palliative or reparative surgical techniques. Additional indications include comorbid conditions such as malalignment and ligament or meniscal deficiency, which have contributed to a premature failure of the surgical procedure and can be appropriately addressed concomitantly or in a staged fashion. Osteotomies should be considered in any patient with varus or valgus alignment whose mechanical axis passes through the affected compartment on a standing-AP-alignment radiograph (Fig. 66.1). The osteotomy should be planned to correct the mechanical axis to neutral in the case of cartilage preservation (Fig. 66.1). However, slight correction beyond neutral alignment should be planned in the setting of pain and arthrosis. Alternatively, in the setting of anterior or posterior cruciate ligament deficiency a sagittal plane osteotomy may be considered to improve joint kinematics and decrease tibial translation. Finally, a tibial tubercle osteotomy should be considered in any patient with patellofemoral lesions. The degree of anteriorization versus medialization can be titrated based on the patient’s history of instability, maltracking (TT-TG distance), or arthrosis.
TIMING
In the setting of complex and revision cartilage surgery, patients may require osteotomies, meniscal transplants, and/or ligament reconstruction in an effort to preserve joint function and protect the cartilage-restorative procedure. The ideal timing of these procedures, whether undertaken simultaneously or in a staged fashion, is an important part of the preoperative planning and affects patient expectations regarding time to recovery and possible need for multiple surgeries.
Cartilage or Meniscus Deficiency and Malalignment
A focal cartilage defect or meniscal deficiency in the medial or lateral tibiofemoral compartment, with varus or valgus alignment, respectively, may be managed either simultaneously or staged. In general, young, active patients can be treated simultaneously with a high-tibial osteotomy or distal femoral osteotomy (DFO) and concomitant cartilage procedure (Fig. 66.2). Older, less active patients may benefit from an osteotomy first, followed by a period of observation. These patients may have satisfactory symptomatic relief from the osteotomy such that an additional cartilage procedure may not be warranted. Patients with previously failed patellofemoral lesions are often treated with a distal realignment procedure of the tibial tubercle to decrease the contact pressure of the patellofemoral joint (Fig. 66.3) along with the cartilage procedure.
Cartilage or Meniscus Deficiency and Ligament Deficiency
Patients with cartilage lesions or meniscal deficiency and instability due to ACL deficiency are managed with an ACL reconstruction and cartilage restoration or meniscal transplantation in an effort to restore joint kinematics and decrease shear across the joint surface. Cartilage lesions in the setting of a previously failed ACL reconstruction are common. Patients requiring a revision ACL
reconstruction with extensive bony tunnel expansion should be managed with a staged bone-grafting procedure followed by ACL reconstruction when the grafted tunnels have matured. We typically use bone-patellar tendon-bone or Achilles tendon allografts for revision treatment to reduce patient morbidity and provide versatility in graft-fixation techniques when combined procedures are performed.
reconstruction with extensive bony tunnel expansion should be managed with a staged bone-grafting procedure followed by ACL reconstruction when the grafted tunnels have matured. We typically use bone-patellar tendon-bone or Achilles tendon allografts for revision treatment to reduce patient morbidity and provide versatility in graft-fixation techniques when combined procedures are performed.
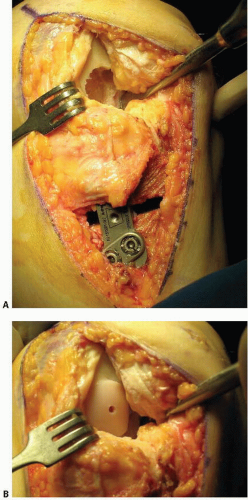 FIGURE 66.2. Cartilage restoration with realignment. This patient is a 36-year-old male with a history of multiple surgeries for a medial femoral condyle (mFC) defect. The initial evaluation revealed a 20-by-20-mm defect and varus deformity. definitively underwent osteochondral allograft (OA) of mFC and hTO. A: high tibial osteotomy done with hardware in place. The socket for the osteochondral allograft on the femoral condyle has been prepared. B: The osteochondral allograft has been placed.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|