FIGURE 31-1 A: Hip radiograph of an elderly patient with malpositioned acetabular component and recurrent instability. B: Hip radiographs after revision. Note the acetabular component was revised to an optimal position, and a constrained liner was added for additional security in this elderly patient with scoliosis and abnormal body mechanics.THA, from 1% at 1 month to 1.9% at 1 year and then a constant additional rate of 1% every 5 years to a 7% rate at 25 years.
EPIDEMIOLOGY
Frequency of Hip Instability The prevalence of dislocation after THA varies widely, from 0.3% to 15%.1–7 In large series, the rate appears to be 2% to 3%.6,8–14 At the Mayo Clinic, Woo and Morrey15 noted 331 dislocations out of 10,500 primary and revision THAs, for a rate of 3.2%. However, the reported dislocation rate was 2.4% for primary THA and 4.8% for revision THA.15 After multiple procedures, the prevalence of dislocation after revision THA is much greater, with some series reporting rates from 10% to 28%.16,17 In an excellent review by Morrey, which combined the data in several large series, the dislocation rate was found to be 2% of 4,753 primary THAs and 6% of 1,290 revision THAs.3 Several presumed factors lead to an elevated risk for dislocation after revision surgery, including (i) poorer soft tissues, (ii) altered abductor muscle attachments, (iii) use of extensile surgical exposures at revision, and (iv) nonanatomic component positioning necessitated by bone loss. Regardless, the true prevalence of this problem is not known and varies due to heterogeneity of patient cohorts, different surgical techniques, and variable clinical follow-up.7,18,19
In addition, the prevalence of hip instability differs with time. Dislocations can be categorized as early (within 6 months), intermediate (6 months to 5 years), or late (>5 years).20 In most series, 60% to 70% of initial dislocations occur with the first 6 weeks after the index surgical procedure.7,8,11,14,21,22 The reduced risk over time is likely due to healing of soft tissues, improved muscle tone, and formation of a pseudocapsule around the joint.3,23 Berry et al.24 found that the cumulative rate of dislocation increased over time for Charnley
Hip Instability as Reason for Revision In a recent epidemiologic study by Bozic et al.,25 one of the most common causes of revision THA in the United States was instability, accounting for 22.5% of revisions. In another study by Jafari et al.,26 instability was the second most common indication for revision THA, accounting for 15% of the cases. Interestingly, instability was the second most common cause of failure for the revision procedures as well at 25.1%. The prevalence of recurrent dislocation necessitating operative treatment has been reported to range from 13% to 42%.2,7,27 Morrey noted that 22% of 142 hips that had recurrent dislocations required operative treatment.3
TREATMENT OPTIONS
The choice between surgical or nonsurgical treatment of hip dislocation is dependent on three factors: (i) whether the dislocation is recurrent (greater than two episodes), (ii) the chronology of the dislocation (i.e., early, intermediate, or late), and (iii) patientspecific factors.
Closed Treatment The majority of dislocations that occur early (within 3 months of the procedure) and are the first or second dislocation(s) can be treated effectively with closed reduction.9 Certainly, there are exceptions, including those with failed implants, significant component malposition, and dislocations that cannot be reduced or closed. After reduction, the hip is immobilized for 6 to 12 weeks with either a hip abduction brace or hip spica cast. The brace limits hip abduction and flexion, whereas the cast provides even more constraint for those with very unstable hips. Patients treated nonoperatively have a >60% chance of avoiding future recurrence.8,12,15,21 At the Mayo Clinic, limiting flexion and internal rotation with a hip abduction brace for 6 weeks is the preferred means of treating first-time posterior dislocations.
Operative Treatment As previously noted, surgical treatment of hip instability is one of the most common causes of revision THA. Furthermore, the redislocation rate after reoperation for hip instability has been reported to be as high as 40%.6,9,28 As such, surgeons must understand the (i) direction of the dislocation (anterior, posterior, or directly lateral), (ii) etiology of the dislocation, and (iii) techniques and technologies that may aid in rectifying the problem. The etiologies contributing to instability can be placed in one or more of the following categories: component malposition, impingement, unsatisfactory soft tissue tension, and/or abductor deficiency/trochanteric nonunion.
Diagnoses
COMPONENT MALPOSITION Component malposition is one of the most common causes of recurrent hip instability (Fig. 31-2). Furthermore, it is one of the factors often avoidable by the surgeon. Malposition can occur with either the acetabular or femoral component, although acetabular malposition is more common. Lewinnek et al.13 found that the safe zone for placement of the acetabular component was in 40 ± 10 degrees of abduction and 15 ± 10 degrees of anteversion.13 Excessive anteversion will predispose to anterior dislocations, whereas retroversion will predispose to posterior dislocations. An overly abducted socket (too vertical) may increase the risk of lateral dislocation when the leg is adduced. Fackler and Poss10 showed that 44% of 34 patients with dislocations had malposition of one or both components, compared with 6% in a control population with stable hips. Ali Khan et al.8 found that half of 142 patients with hip dislocations had unsatisfactory acetabular component anteversion or abduction. Daly and Morrey9 documented similar findings at Mayo.
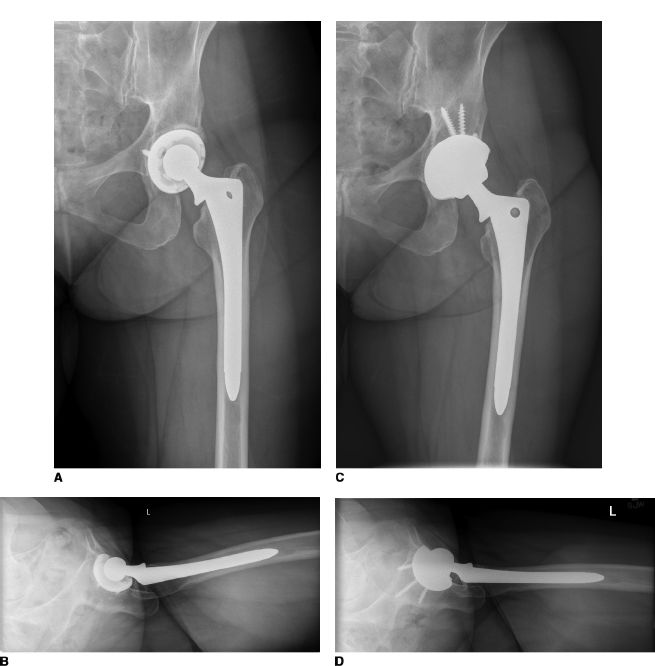
FIGURE 31-2. A,B: Hip radiographs of a 57-year-old woman with recurrent anterior dislocation after primary THA. The acetabular component position is excessively vertical and excessively anteverted. C,D: Hip radiographs after acetabular revision to optimize cup position.
Currently, there is a paucity of literature surrounding femoral component position due to the fact that accurate measurements of femoral component anteversion are difficult to assess on plain radiographs. Furthermore, femoral component malpositioning is easier to avoid intraoperatively. However, most agree that excessive anteversion increases the risk of anterior dislocation, whereas inadequate anteversion results in increased posterior dislocation. Computed tomography may assist in determining the version, particularly if revision surgery is considered, given that removal of a well-fixed stem may result in significant bone loss. Regardless, Daly and Morrey9 reported that improper femoral component version was rarely an isolated cause of instability. However, in the series by Fackler and Poss10 and a study by Herrlin et al.,29 excessive and inadequate anteversion, respectively, were associated with hip instability.
It is important to note that anteversion is additive. While excessive anteversion of either component alone may not always cause a problem, the combination of excessive anteversion in both components has a higher change of leading to dislocation.30 Most experts agree that combined acetabular and femoral anteversion should be approximately 45 degrees when a posterior approach is used and a little less when an anterior approach is utilized.6
IMPINGEMENT Impingement is the process by which bony structures, soft tissues structures, or the prosthesis itself can serve as a fulcrum, allowing the prosthetic head to be levered out of the socket.6 Based upon the position of the hip, various forms of impingement may occur. With the hip flexed and internally rotated, the greater trochanter or anterior proximal femur can impinge on the pelvis. Furthermore, any form of soft tissue can serve as a fulcrum in this position. In extension, adduction, and external rotation, impingement can occur between the femur and ischium, leading to anterior dislocations. Prosthetic impingement may occur secondary to implant malposition, poor head-to-neck ratio, and elevated rims. Low head-to-neck ratios and elevated rims result in decreased range of motion prior to impingement.
Amstutz et al.31 showed that femoral components with an increased head-to-neck ratio had greater range of motion prior to impingement, thus limiting dislocations. Moreover, Krushell et al.32 noted decreased impingement with a modular neck design in which the neck geometry was flattened. In essence, longer modular heads with a skirt result in early impingement since the femoral neck diameter is increased.
UNSATISFACTORY SOFT TISSUE TENSION Inadequate soft tissue tension is truly a spectrum, with the most severe example being abductor insufficiency/trochanteric nonunion (discussed next). While not proven, poor soft tissue tension almost certainly contributes to hip instability.33 There are five main causes of unsatisfactory soft tissue tension: capsulectomy, reduction of femoral offset, limb shortening, extensive soft tissue dissection, and trochanteric nonunion.
Historically, the incised capsule was allowed to form a “pseudocapsule.” However, reconstruction of the posterior capsule and short external rotators after a posterior approach was shown to reduce dislocation from 4.1% to 0% at 1-year follow-up in 395 patients.34 Likewise, Goldstein et al and White et al reported reductions in dislocation after this capsulorrhaphy technique.35,36 As such, it appears that capsulectomy reduces soft tissue tension and/or restraint to motion and is thus a risk factor for dislocation. In regard to femoral offset, Fackler and Poss10 showed that patients who dislocate frequently have a notable loss of femoral offset (average of 5.2 mm) compared to patients with stable hips (average of 0.02 mm) (Fig. 31-3). On the other hand, the data surrounding limb lengths and stability are ambiguous. Fackler and Poss10 found no statistical correlation between postoperative limb lengths and the incidence of dislocation. Furthermore, Coventry33 found that the operated limb was shorter than the opposite limb in only 25% of patients with late dislocations. Woo and Morrey15 noted that patients with unstable hips had limb lengths that were 1.6 mm longer than the contralateral limb.
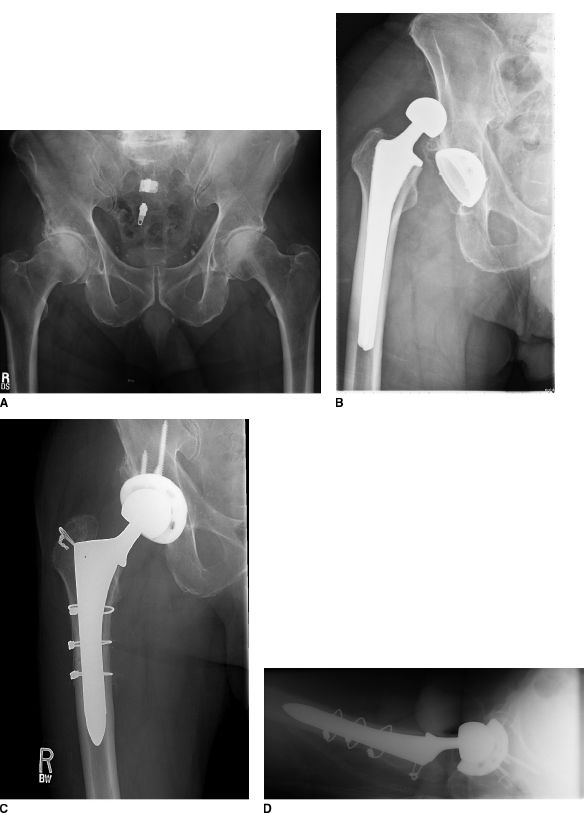
FIGURE 31-3. A,B: Hip radiograph of a patient with recurrent hip instability after primary THA. Note the acetabular component position is not optimal, and also note the femoral component does not provide nearly as much offset as the patient’ s “native” hip. C,D: Hip radiographs after acetabular and femoral component revision. Implant position and femoral offset were optimized, and a larger diameter femoral head was added to further optimize hip stability.
ABDUCTOR INSUFFICIENCY/TROCHANTERIC NONUNION Abductor insufficiency is one the most difficult causes of hip instability to solve. The abductors may be deficient or dysfunctional secondary to trauma, failure of abductor or greater trochanteric healing after previous operations, or superior gluteal nerve dysfunction.6 The adverse effects of trochanteric nonunion, especially if associated with proximal migration, have been observed by many investigators.15,37,38 Woo and Morrey reported a 17.6% dislocation rate when trochanteric nonunion occurred with 1-cm proximal trochanteric migration.15 However, the incidence of dislocation was drastically lower at 2.8% in THAs in which an osseous or a stable fibrous union of the greater trochanter was obtained. Nevertheless, the cumulative risk of dislocation is statistically significantly lower with transtrochanteric approaches suggesting that when tro-chanteric healing occurs, the good soft tissue restoration and opportunity to advance the trochanter can provide excellent hip stability.39
Treatment Algorithm
IMPLANT MALPOSITION Implant malpositioning can be considered minor or major. Such a distinction is essential in determining treatment options. Minor adjustment to acetabular position can be accomplished with the use of elevatedrim liners for modular sockets or socket wall additions for nonmodular sockets (Fig. 31-4).40–44 The elevatedrim or face-changing liner can be placed posteriorly to produce more effective cup anteversion, anteriorly to decrease relative anteversion, and directly lateral to reduce the relative cup abduction. In a laboratory simulator, Krushell et al.45 were able to show that elevated rims improved stability when used to compensate for a malpositioned acetabular shell. Likewise, in the initial Charnley design, an acetabular component with an elevated posterior wall decreased the dislocation rate.2 The above advantages must be balanced with the increased risk of polyethylene wear and component loosening.
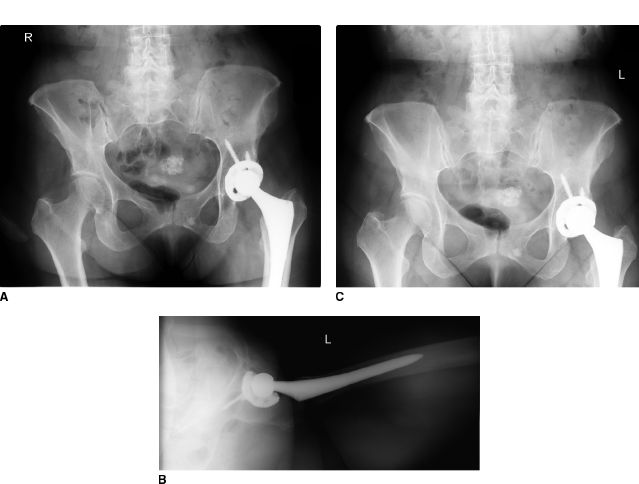
FIGURE 31-4. A,B: Hip radiographs of a woman with recurrent anterior hip instability. C: Hip radiographs after femoral head and liner exchange. A larger diameter head was used to minimize impingement, and a face-changing acetabular liner was placed to reduce effective acetabular anteversion.
Markedly malpositioned implants require component reorientation. The acetabular component is typically revised given that malposition of this component is more frequent, combined with the fact that measurement of the femoral component position on plain radiographs is more difficult.7 As previously stated, the safe zone for the acetabular component is in 40 ± 10 degrees of abduction and 15 ± 10 degrees of anteversion.13 In addition, the surgeon must be aware that patients roll forward during a posterior approach with the patient in a lateral position, leading to an exaggerated sense of acetabular anteversion. This is enhanced during the posterior approach given the fact that the internal rotation of the femur rolls the pelvis forward. As such, bony acetabular landmarks including the ischium posteriorly, the bottom of the fovea inferiorly, the anterior wall, and the lateral acetabulum are essential guides to implant position intraoperatively. Furthermore, an intraoperative radiograph can be very valuable. Medialization of the hip center leads to an increased risk for bony impingement between the femur and pelvis and thus increased risk for instability. As such, medial bone deficiencies should be addressed with extra large cups, extra depth cups, eccentric socket liners, and/or medial bone grafts to avoid medialization and the resultant potential problems of bone-to-bone impingement.
IMPINGEMENT If impingement is contributing to hip instability, then the impingement source must be relieved. Impingement between the greater trochanter and pelvis with hip flexion and internal rotation may be treated either by excising a portion of the anterior greater trochanter or by removing hypertrophic soft tissues in the region of the anterior capsule and reflected head of the rectus femoris.6 Likewise, impingement between the femur and ischium with the leg in extension, adduction, and external rotation can be treated by removing prominent bone of the ischium or removing hypertropic posterior inferior capsule or scar tissue.
When prosthetic impingement is the offending source, it can be relieved by improving the implant position, optimizing the head-to-neck ratio, or removing an elevated acetabular rim liner.6 In revision surgery, medial bone loss may result in placing the cup in a medialized position, increasing the risk of femoral bone–acetabular bone impingement and instability. In this case, a lateralized liner or deep profile acetabular component can help reconstitute the hip center of rotation. The surgeon, however, should be aware that lateralized liners do increase the torque on the acetabular component during weight bearing. Furthermore, the surgeon must be aware that removal of impingement alone is the least successful treatment for instability.3
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








