Fig. 17.1
Radiographs of a postoperative acromial fracture (a) and scapular spine fracture (b)
Acromial wear is often seen in patients with cuff tear arthropathy, and this may have a deleterious effect on the acromion. The acromial insertion of the deltoid is important for deltoid tensioning, and a weakened acromion from wear or previous surgery may increase the risk of fracture or fragmentation.
Literature Review and Outcomes
Preoperative Acromial Insufficiency
Many patients undergoing RSA present with massive rotator cuff tears, and superior humeral head migration, with or without glenohumeral arthritis. In 1990, Hamada described a radiographic classification of massive cuff tears divided into 5 stages [18]. Stage I has minimal radiographic changes. Stage II has narrowing of the subacromial space to 5 millimeters (mm) or less. In stage III, there is erosion and acetabularization of the acromion secondary to proximal migration of the humeral head. Stage IV is associated with glenohumeral arthritis with or without acetabularization (stage IVA and IVB, respectively). Stage V shows the onset of humeral head osteonecrosis.
Patients presenting with acetabularization often have thinning, fragmentation, or fracture of the acromion. Walch et al. [17] evaluated a series of 457 consecutive patients undergoing RSA and identified 41 patients with a preoperative lesion of the acromion or scapular spine. Twenty-three patients had an os acromiale, while 17 patients had fracture or fragmentation of the acromion, and one patient had a pseudarthrosis of the scapular spine. In their study, preoperative acromial pathology did not affect the postoperative functional outcomes, and the authors suggested that preoperative acromial lesions are not a contraindication to RSA.
Postoperative Scapula Fractures
Postoperative acromial or scapular spine fractures after RSA have been found to have adverse effects on the patient’s overall functional outcome. The cause of these fractures is unknown, but some etiologies may include overtensioning the deltoid, acromial thinning or wear, relative osteopenia or osteoporosis of the scapula, and abnormal contact from the tuberosity with abduction, which can be seen if the glenosphere is placed too high on the glenoid.
While the management of these fractures has been debated, it is important to properly evaluate the patient at the presence of pain after a RSA in order to rule out a scapula fracture.
Clinical Presentation
It has been reported that scapula fractures may occur between 1 and 94 months postoperatively, with most occurring within the first year [12, 15]. Patients typically present with an acute onset of pain in the shoulder, and many give a history of pain with therapy exercises, overuse of the arm, or a fall. Clinically, the patients will have point tenderness over the acromion or scapular spine, and they will have decreased function and ability to raise the arm.
At the initial presentation of pain, it is important to rest the patient in a sling or a brace and to evaluate them with plain radiographs. While many fractures may be visible on plain radiographs, it has been reported that up to 30 % may not have a fracture visible on initial radiographs [12]. In addition, Otto et al. reported that only 78.8 % of known fractures were accurately diagnosed by independent observers using plain radiographs alone [12]. Therefore, it is suggested that if there is a suspicion of a fracture, advanced imaging such as a computed tomography (CT) may be necessary to make an accurate diagnosis.
It is also important to evaluate the patient’s comorbidities for possible risk factors for fracture. It was found that patients with osteoporosis as diagnosed by a dual-energy X-ray absorptiometry (DEXA) have a significantly increased risk of fracture occurrence [12]. Smoking and prolonged corticosteroid use was associated with a higher rate of fracture occurrence but neither reached statistical significance. It is important to take a thorough history and counsel these patients on the potential risk of these fractures occurring.
Radiographic Evaluation
When evaluating initial plain radiographs, it is important to obtain a complete series of radiographs, including an anteroposterior, true anteroposterior in the plane of the scapula (Grashey), axillary lateral, and scapular Y view. There are several radiographic parameters that have been identified that may improve the accuracy of making the diagnosis of a fracture.
In addition to trying to localize the fracture on the acromial body or scapular spine, it is important to evaluate the relationships of the bony anatomy and the prosthesis. Acromial thickness, which is noted to decrease with a high riding humeral head and associated acromial wear, does not have a significant effect on the risk of fracture. Surgical technique has been evaluated to determine whether the amount of lateralization and/or lengthening of the humerus increased the risk of fracture by overtensioning the deltoid [12]. Neither the amount of medialization or lateralization [as measured by the glenoid to greater tuberosity (GT) distance], nor the amount of lengthening [as measured by the acromion to greater tuberosity (AT) distance] had an effect of the risk of fracture [12]. Nonetheless, it is important not to overtension the deltoid by placing the baseplate too low. In addition, it has been shown that the observation of a decreasing AT distance and an increasing acromial tilt angle (as measured by the angle of the scapular spine and acromial body) on consecutive radiographs may improve the detection of fracture on plain radiographs [9, 12] (Fig. 17.2a–d).
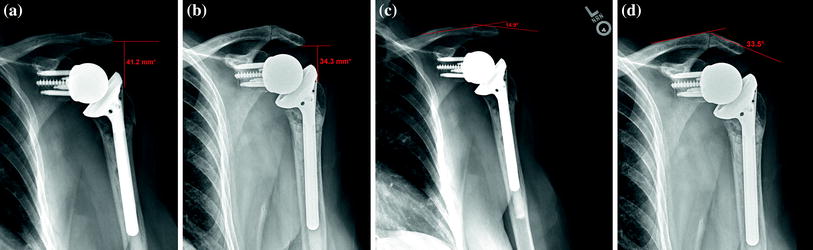
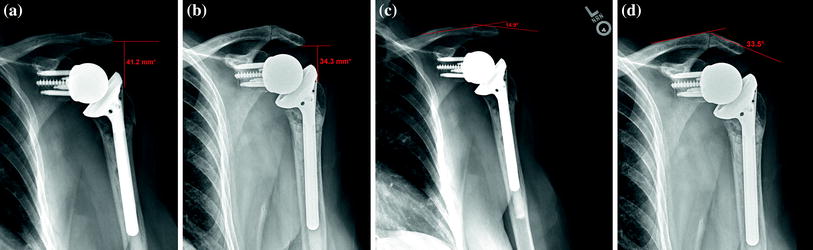
Fig. 17.2
Radiograph showing the pre-fracture acromial to greater tuberosity (AT) distance (a) and post-fracture AT distance (b) with a decreased distance seen on the post-fracture radiograph. Also shown are radiographs with the pre-fracture acromial tilt angle (c) and the post-fracture acromial tilt angle (d) showing an increased angle as the fracture displaced
Crosby et al. identified 4 patients with scapular spine fractures, which were evaluated with three-dimensional CT and suggested that these fractures might be the result of a stress riser from the superior baseplate screw tip [4]. The authors have since recommended against the use of a superior baseplate fixation screw, although this was a small group which was underpowered. In a subgroup analysis of scapular spine patients, Otto et al. [12] identified 14 of 16 scapula spine fractures that were associated with the tip of a screw. However, surgical technique, including baseplate orientation, screw length, and distance from the screw tip to the edge of bone, did not affect the risk of fracture occurrence. The authors did not recommend an alteration of surgical technique to eliminate baseplate peripheral screws.
Despite the improvements of fracture detection with the use of these parameters, if the fracture is not visualized in the presence of pain and tenderness over the acromion, a CT scan is recommended to confirm the diagnosis.
Classification Schemes
The classification of scapular fractures after RSA has been described based on the anatomic relationships. Crosby et al. described fractures in relation to the acromioclavicular (AC) joint [4]. Type I fractures were small fractures of the anterior acromion near to or including the footprint of the coracoacromial ligament. Type II fractures occurred through the anterior acromion just posterior to the AC joint. Type III fractures were fractures of the posterior acromion or scapular spine. The authors made recommendations for treatment based on the type of fracture; however, the classification was not validated. In an independent evaluation, Otto et al. reported that the classification only had moderate inter-rater reliability, suggesting that an alternative classification method is needed [12].
Levy et al. [10] identified and described fractures into 3 subtypes based on the deltoid muscle origin (Fig. 17.3). Type I fractures occurred through the mid-portion of the acromion, involving a portion of the anterior and middle deltoid origin. Type II fractures involved at least the entire middle deltoid origin with a portion but not all of the posterior deltoid origin. Type III fractures involved the entire middle and posterior deltoid origins. The classification had excellent interclass correlation, but all fractures were treated conservatively with no attempt to suggest surgical intervention.
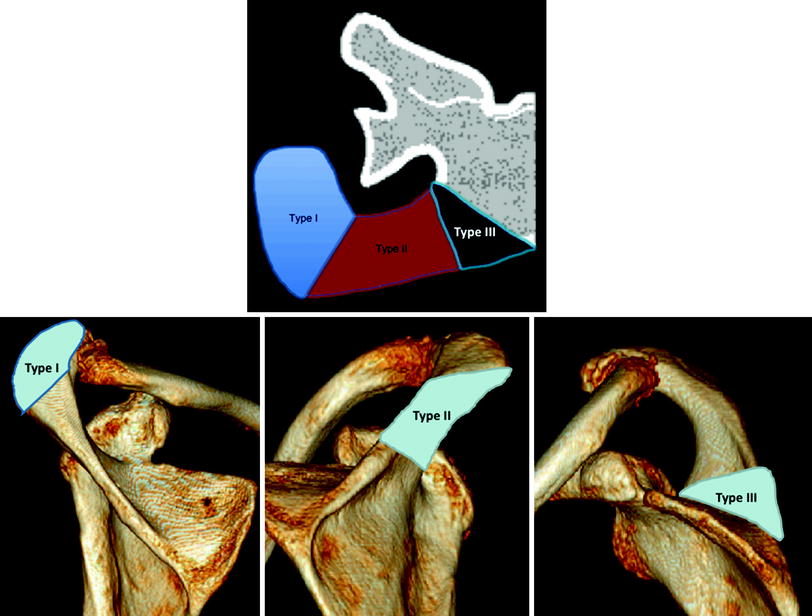
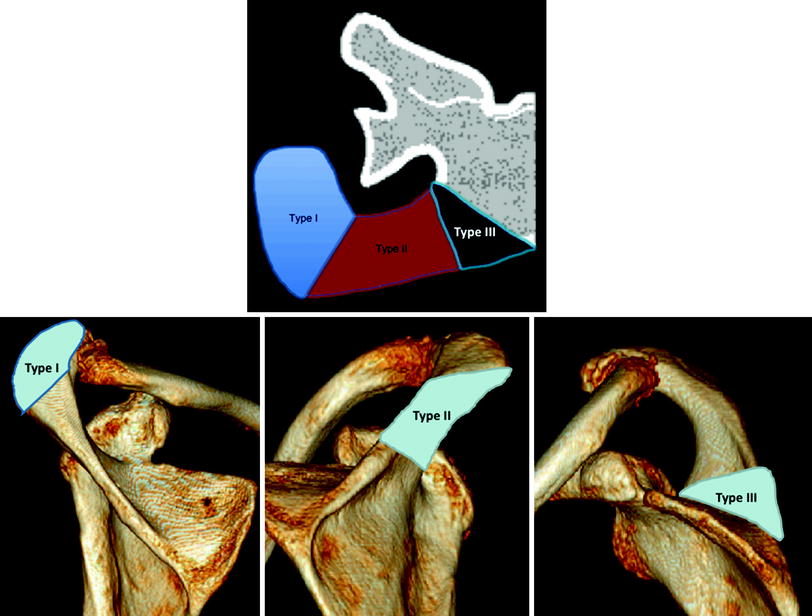
Fig. 17.3
Classification of scapula fractures after reverse shoulder arthroplasty according to Levy et al. [10]. Used by permission
Treatment Options and Outcomes
While these fractures can be difficult to detect clinically, the optimal management of them also remains unknown. Postoperative scapular fractures following RSA were first described in 2005 by Boileau et al. [1]. There were 2 postoperative acromial fractures noted at the 3-month follow-up visit, which were managed nonoperatively with no apparent effect on outcome. Since that time, other authors have also reported on their outcomes in managing this complication. However, no consensus regarding management exists at this time.
Both operative and nonoperative treatment has been proposed. Most authors have managed this complication nonoperatively do to an early high complication rate with operative management of scapula fracture in the setting of RSA (Fig. 17.4a, b). Rittmeister et al. originally showed a 100 % rate of acromial nonunion following RSA utilizing a transacromial approach [13]. Difficulty in achieving union in these fractures is believed to be increased stress at the fracture site due to elongation of the deltoid in the setting of osteoporotic bone.
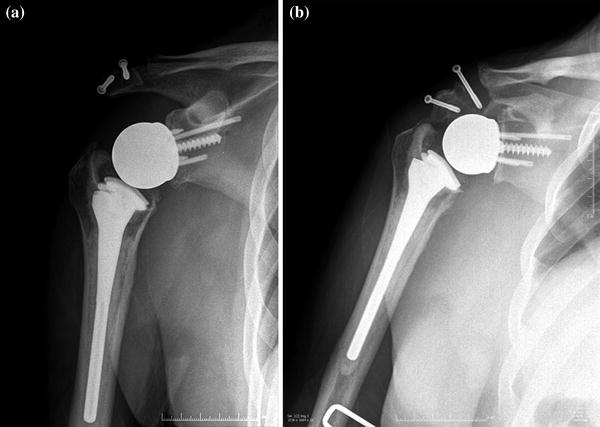
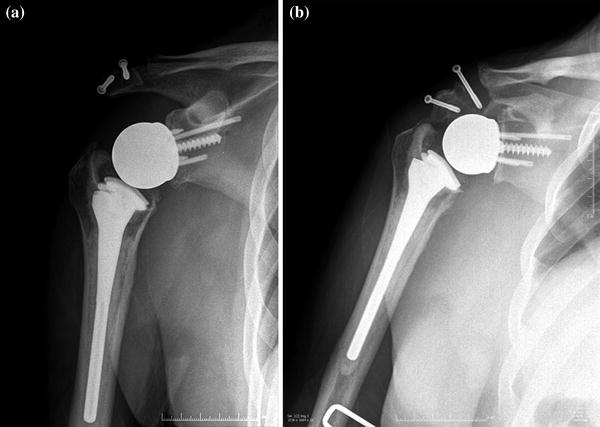
Fig. 17.4
Radiograph showing an acromial fracture treated with screw fixation (a) and follow-up radiographs showing loss of fixation with screw pull out (b)
Similarly, Frankle et al. [6] reported on 3 postoperative scapula fractures in his initial series. Two of those were treated nonoperatively and the third one was treated with open reduction and internal fixation (ORIF). All of these healed uneventfully with “excellent” outcomes. In that series, a patient with preoperative acromial fracture treated with ORIF had hardware failure and infection at 5 months post-op and was treated with revision ORIF and irrigation and debridement with satisfactory outcome. Walch et al. [17] also reported a case of postoperative fracture treated with tension band wiring which went to nonunion and required hardware removal.
In spite of these poor results with operative management, some authors have recommended operative treatment to improve pain from the fracture and restore deltoid tensioning [4, 14, 16]. Operative treatment has mostly included ORIF with tension band wiring or plate and screw fixation. In the largest series of operative fixation of postoperative scapula fractures following RSA (11 cases), Crosby et al. demonstrated operative treatment to provide good short-term pain relief at mean follow-up of 10 months; however, further details regarding validated outcome scores or functional metrics are not reported [4]. Wahlquist et al. also reported on 5 cases of acromial base fractures following RSA, three of which were treated with ORIF with plate and screw fixation [14]. They found no difference between operatively treated cases and nonoperatively treated cases with regard to functional outcomes, but showed improved range of motion in operatively treated cases. Outcomes of operative treatment of postoperative scapula fracture are shown in Table 17.1.
Table 17.1
Operative treatment of postoperative scapula fractures following RSA
Author | Fracture type
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|
|---|





