Fig. 27.1
Influence of the humeral cut on arm length. a Preoperative status with a lack of deltoid tension. b–c An aggressive humeral cut results in a low implantation of the stem with a lack of deltoid tension. d–e A minimal humeral cut leads to a high implantation of the prosthetic stem with adequate deltoid tension. From: Lädermann et al. [12]. Used with permission
The acromiohumeral distance or the acromioprosthesis distance is the distance between the inferior border of the acromion and the superior aspect of the prosthesis. This distance is primarily affected by prosthesis design but can also be influenced by component positioning and acromion status (e.g., decrease with postoperative acromion fracture). This distance increases with a shallower neck-shaft angle of the prosthesis (Fig. 27.2), the use of a spacer, a thicker polyethylene, inferior position of the glenosphere in the coronal plane (Fig. 27.3), a larger glenosphere, and the use of an eccentric or inferiorly tilted glenosphere [12, 13]. The neck-shaft angle is one of the biggest variabilities between different prosthesis designs. For every 10° decrease, the acromiohumeral distance shortens by approximately 3 mm (personal data). In other words, between a 155° and a 135° configuration arm, lengthening varies by about 6 mm (Fig. 27.2). New curved stem design, on the other hand, has almost no influence not only on acromiohumeral distance but only on humeral lateralization.
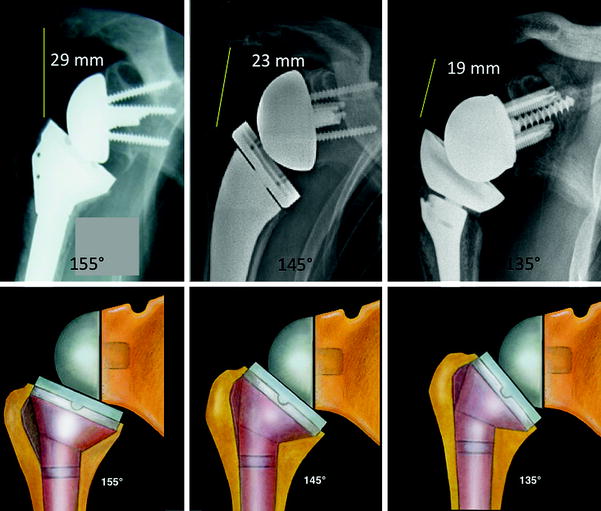
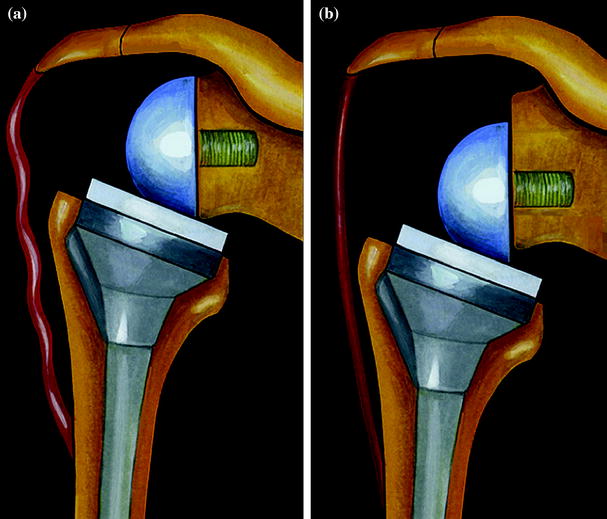
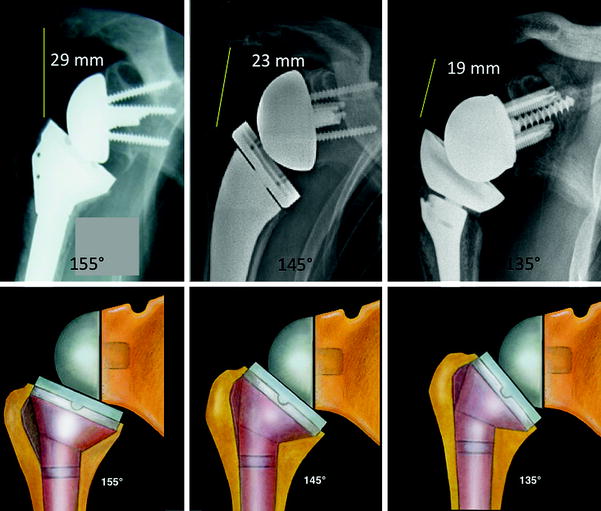
Fig. 27.2
Relationship between neck-shaft angle and acromiohumeral distance. A steeper or more anatomic neck-shaft angle (Grammont-type 155° vs. 145° and 135° curved design in this example) leads to a decrease in the acromiohumeral distance
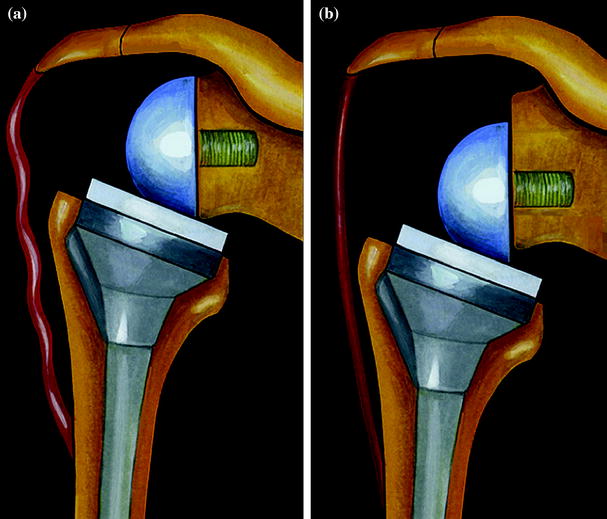
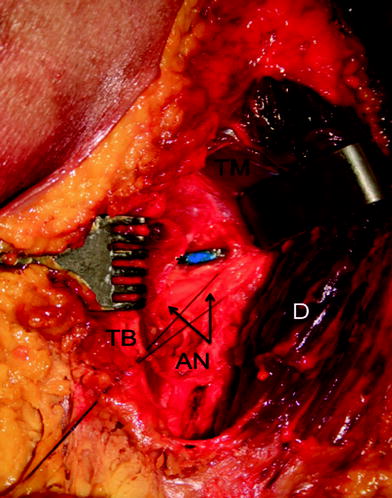
Fig. 27.3
Influence of position of glenosphere in vertical plane. a A rather high implantation of the baseplate or the use of a non-eccentric glenosphere does not allow proper deltoid re-tensioning. b The use of an eccentric glenosphere or a low position of the glenosphere in the vertical plane allows satisfactory deltoid re-tensioning. From: Lädermann et al. [12]. Used with permission
Arm length is defined as the length from the acromion to the epicondylar axis and therefore represents the combined humeral length and acromiohumeral distance.
The position of the glenosphere is theoretically fixed, as it should be implanted on the lower part of the glenoid to avoid notching [14–18]. The type of glenosphere (size, eccentricity) allows adjustment of arm length by only several millimeters (about 1 % of arm length). Consequently, the key factors for arm length are the height of the stem, type of stem, polyethylene thickness, and the use of an augment or spacer. Collectively, these factors allow arm lengthening by up to several centimeters (about 10 % of arm length).
Biomechanical Changes Induced by the Implant
RSA, often used in multiple operated patients with distorted anatomy, imparts physiological and biomechanical changes that may increase the potential for complications [3]. First, medialization in the center of rotation doubles the lever arm of the deltoid muscle, allowing recruitment of more anterior and posterior deltoid fibers and therefore increasing deltoid abduction efficiency. These phenomena are also responsible for impingement of the medial border of the humeral component on the scapular neck. Repetitive contact between polyethylene and bone may result in polyethylene wear debris, chronic inflammation and osteolysis [18, 19], radiolucency around the glenoid component [20], loosening of the glenoid component [21], presence of an inferior bone spur, and ossification in the glenohumeral space [7, 16, 22]. Second, the fixed nature of the glenosphere places torsional forces on the humerus that may affect humeral component instability [23]. Third, the semi-constrained nature of the prosthesis restores glenohumeral stability which provides the stable fulcrum which is essential for active anterior elevation. Finally and most relevant to this chapter is lengthening of the arm which provides space for range of motion of the proximal humerus, enhances stability, and re-tensions the deltoid. The latter factor is critical due to the semi-constrained design of the prosthesis. The increase in compressive force between the humeral and glenoid components has a stabilizing effect [9]. Under such tension, the reverse glenoid component provides the stable fulcrum essential for shoulder anterior elevation and prosthesis stability [8]. This tension is determined by arm length.
Techniques to Measure Humeral and Arm Lengthening
Few techniques of lengthening with RSA have been validated. Measurement techniques can be either radiographic or clinical. Measurements can focus on the length of the arm, humerus, or acromiohumeral distance. Renaud et al. [24] were the first to propose the determination of a “radio-anatomic index.” They measured acromiohumeral distances on anteroposterior radiographs (Fig. 27.4) but did not control for magnification. In cases of superior escape of the contralateral humeral head, the normal position of the humeral epiphysis was estimated using a horizontal line that passed perpendicular to the center of the glenoid. However, the presence of superior glenoid erosion [25] renders this technique inaccurate.
Fig. 27.4
Technique of Renaud et al.: a Two main lines are placed for measurement: an acromial line that represents the superior cortex of the acromion and a tangent line to the center of the prosthetic epiphysis or to the center of rotation of the humeral head perpendicular to the first line. b The two latter lines represent the acromio–epiphyseal distance and are compared to provide a ratio of lengthening. From: Renaud et al. [24]. Used with permission
Lädermann et al. [13] recommended a technique to determine arm and humeral length using bilateral plain anterior–posterior radiographs taken under magnification and fluoroscopic control (Fig. 27.5).
Fig. 27.5
Technique of Lädermann et al. Preoperative and postoperative true anteroposterior, bilateral, magnification controlled radiographs of the humeri with neutral rotation and the patient standing. An epicondylar line (EL) defined as being between the most lateral part of the medial and lateral epicondyle. The diaphyseal axis (DI) is determined by a line drawn in the center of the proximal humeral medullary canal. The intersection between the epicondylar line and the diaphyseal axis represents the point C. The intersection between the diaphyseal axis and top of the humeral head is named H. The point A is located at the intersection between the diaphyseal axis and a perpendicular line passing through the most lateral and inferior point of the acromion. A, C, and H are represented by small white points; large white points correspond to the magnification control marker adhered on the skin of the arm. A acromion; C condyles; H head; EL epicondylar line; DI diaphyseal axis; pre-op preoperative; contro controlateral; EF enlargement factor
A similar technique to assess the amount of lengthening of the humerus was subsequently reported by Greiner et al. [26]. Lädermann et al. [13] compared the lengths of the affected and contralateral humeral shafts to determine whether the contralateral humerus may be reliably used to determine prosthetic height in complex cases with humeral bone loss, or to perform a postoperative assessment in revision cases where preoperative scaled radiographs of the humerus are unavailable. One disadvantage of this technique is the need to perform magnification controlled radiographs of the entire humerus. As the X-ray beam is centered at the middle third of humerus, these radiographs do not provide an accurate depiction of the acromiohumeral interval. Consequently, this technique of measurement accurately reflects humeral length, but accuracy of the acromiohumeral interval measurement is compromised. Moreover, this technique requires drawing an epicondylar reference line that can be difficult if the humerus is not in neutral rotation.
Jobin et al. [27] proposed another technique to evaluate subacromial and deltoid length postoperatively. In their study, complete preoperative and postoperative true anteroposterior radiographs of the glenohumeral joint in neutral rotation were collected. Subacromial length (acromion to greater tuberosity distance) was measured as the distance from the inferolateral acromial tip to the most prominent superolateral aspect of the greater tuberosity (Fig. 27.6). Middle deltoid length was defined as the distance between the inferolateral tip of the acromion and the midpoint of the deltoid tuberosity with the arm in neutral rotation and 0° abduction, as proposed initially by De Wilde et al. [28]. Length was calibrated by the known diameter of the glenosphere and the fixed bony distances of the humeral shaft width (h), as well as the fixed bony distance from the greater tuberosity to the deltoid tuberosity. Since the technique of Jobin et al. calibrates each radiograph to the glenosphere diameter, it is impossible to determine humeral and subacromial length preoperatively. This technique is therefore not useful in preoperative planning of difficult cases such as those with proximal bone loss. Furthermore, the greater tuberosity was selected for the proximal reference point. This anatomic landmark may be absent preoperatively, malunited, or be difficult to visualize because of arm rotation. Moreover, humeral radiolucencies, stem subsidence, radiological signs of stress shielding, and resorption of the tuberosities are common complications after RSA [16] that can compromise the anatomic landmarks used in this technique.
Fig. 27.6
Technique of Jobin et al.: Radiographic measurement of the deltoid length from the inferolateral acromion tip to the midpoint of the deltoid tuberosity is shown (left) preoperatively (d) and (right) postoperatively (d′). From: Jobin et al. [27]. Used with permission
Lastly, Boileau et al. [8] clinically measured the length of the arm postoperatively relative to the opposite side using a specially designed external caliper (Fig. 27.7). This technique is noninvasive and easy to apply clinically but does not differentiate between humeral and arm length and is therefore not useful for preoperative planning.


Fig. 27.7
The distance between the acromion and olecranon with the elbow flexed is determined on non-operated (a) and operated (b) sides. From: Boileau et al. [8], with permission
Results for Arm, Humerus, and Subacromial Lengthening
The typical postoperative lengthening of the arm, humerus, and subacromial space (acromiohumeral) with a Grammont-style prosthesis is summarized in Table 27.1. Mean arm lengthening varies from 15 to 27 mm, and mean humeral lengthening varies from −5 to 5 mm. The humeral cut is typically more aggressive when a transdeltoid surgical approach is performed, but this is compensated for by an increase in thickness of the polyethylene liner.
Table 27.1
Mean postoperative arm, humerus, and subacromial space lengthening in mm
Study | Arm (deltoid lengthening) | Humerus | Subacromial space (acromiohumeral distance) |
|---|---|---|---|
Renaud et al. [24] | NA | NA | NA |
Boileau et al. [8] | 15 ± 11 (5–40)a | NA | NA |
Lädermann et al. [13] | 23 ± 12 (4–47)b 20 ± 11 (−2–48)a | 2 ± 6 (−10–16)a | 23 ± 9 (5–41)b |
Greiner et al. [26] | 17 ± 13 (−10–45) | NA | NA |
Lädermann et al. [51] | 27 ± 18 (0–59)a | NA | NA |
Lädermann et al. [55] | DP 17 ± 17, TD 12 ± 1.4a | DP 5 ± 13, TD −5 ± 10a | NA |
Lädermann et al. [12] | 16 ± 19 (−51–54)a | 2 ± 14 (−47–52)a | NA |
Jobin et al. [27] | 21 ± 10b | NA | 23 ± 9b |
Risks Related to Lengthening
Relationship Between Lengthening and Postoperative Function
Range of motion has varied for RSA in different series [10, 29–31]. Poor postoperative anterior elevation can be attributed to improper use, poor patient selection, and preoperative as well as postoperative problems such as acromion fracture, dislocation, or neurological impairment [31, 32]. Renaud et al. [24] demonstrated a correlation between subacromial space lengthening of 33–50 % and (1) a Constant score [33] equal or above 65.5 points (p = 0.024), (2) an anterior elevation equal or above 120° (p = 0.001), and (3) a gain in abduction equal or above 60° (p = 0.016). Lädermann et al. [12] compared patients with lengthening of the arm and those with shortening and found that the postoperative active anterior elevation was significantly greater (145° vs. 122°) for patients with arm lengthening (p < 0.001). In primary cases, Jobin et al. [27] also confirmed that deltoid lengthening correlated significantly (p = 0.002) with active anterior elevation. In their study, deltoid lengthening that achieved an acromion to greater tuberosity distance exceeding 38 mm had a 90 % positive predictive value of obtaining 135° of active anterior elevation. These clinical findings confirm biomechanical studies that have demonstrated the crucial role of the deltoid in postoperative function [1, 34]. However, arm lengthening showed no relationship functional outcome scores including the Constant score [33], DASH score [35], ASES [36], or SST [26, 27].
Relationship Between Lengthening and Postoperative Complications
Dislocation
Dislocation is one of the most common complications after RSA, with rates as high as 14 % which account for almost half of the complications in some series [7, 20, 31, 37–42]. Most cases of dislocation occur during the first few months after implantation and are a result of a technical error [3]. The etiology of dislocation is multifactorial. It can occur due to (1) deltoid insufficiency [31, 32]; (2) lack of anterior restraints including subscapularis insufficiency, conjoint tendon weakness [43], and pectoralis major insufficiency; (3) malpositioning of the components; (4) impingement; and (5) infection. Instability is more frequent in cases of revision arthroplasty [44]. Deltoid insufficiency can be caused by preoperative factors [31, 32] or can result from a postoperative lack of deltoid tension, acromion fracture (Fig. 27.8), polyethylene wear, stem subsidence, or postoperative neurological palsy. Interestingly, there does not appear to be an increased rate of dislocation after postoperative acromion fractures [45, 46]. Lädermann et al. noted a strong correlation (p < 0.0001) between preoperative humeral length and dislocation. Postoperative shortening of the humerus, as compared to preoperative or contralateral humeral length, was observed in all cases of dislocation (Fig. 27.9).
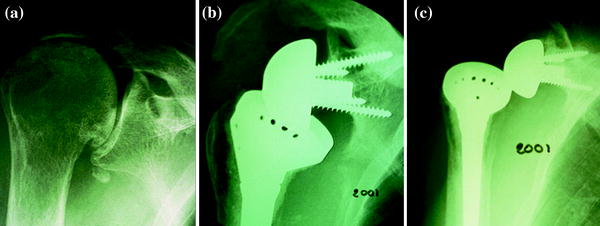
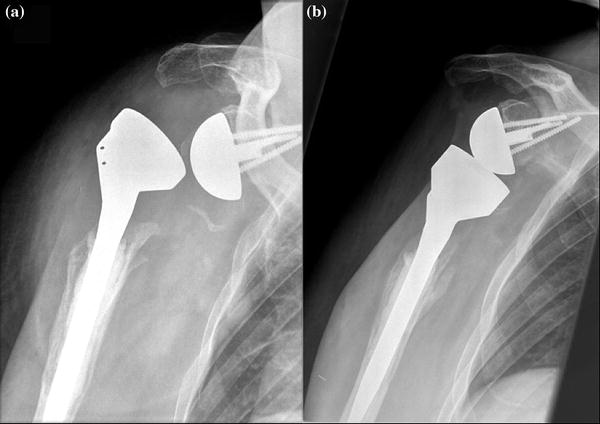
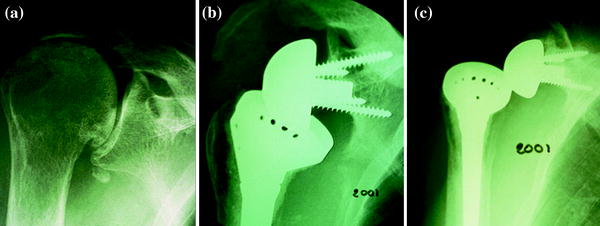
Fig. 27.8
a Preoperative anteroposterior X-ray of a right shoulder with an acromial fatigue fracture. b At two-year follow-up, a postoperative tilt of the acromion and a grade 4 scapular notch are noted. c The prosthetic dislocation could be related to the lack of deltoid tension
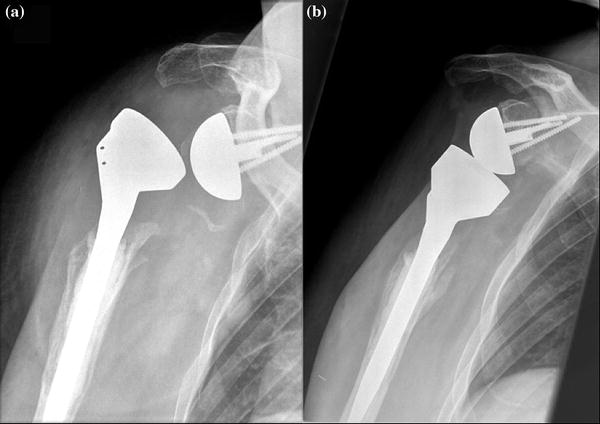
Fig. 27.9
a Dislocation of a right RSA that requires open revision and humeral lengthening with a spacer. b At 47-month follow-up, the patient had no recurrence of instability. From: Lädermann A, Walch G. Reverse shoulder arthroplasty with deltoid insufficiency. Swiss Med Wkly 2012; 142:25S
Neurological Lesions
Lengthening of the arm during RSA, because of its non-anatomic design and/or maneuver of glenohumeral reduction, may be a major factor responsible for the increased prevalence of neurologic injury. Clinically relevant neurological complications involving the brachial plexus or the axillary nerve, however, are rare following RSA [7, 47–50]. A prospective study determined the electrodiagnostic occurrence of peripheral nerve lesions following RSA [51]. If one also takes into account subclinical deterioration of preoperative lesions, 63 % of patients in this study had postoperative neurologic lesions. However, only 5 % of patients had a lesion that was present beyond 6 months postoperative. The prevalence of peripheral nerve lesions following primary RSA is thus common, but most lesions are subclinical and most clinically apparent lesions are temporary. A cadaveric study examined the relationship of the axillary nerve to the prosthesis following RSA. The axillary nerve is not in close proximity to the glenosphere [52], with a distance between the nerve and the glenosphere that was systematically greater than 15 mm. Inferior glenosphere overhang did not appear to decrease the distance to the axillary nerve. Rather, it seems that lengthening of the arm after a RSA leads to a lowering and lateralization of the nerve and protects it from impingement with the glenosphere component. Therefore, the position of the glenosphere in the vertical plane is probably not related to the development of a neurological lesion due to direct contact [52], but it rather related to the proximity of the axillary nerve to the posterior metaphysis or humeral implants (Fig. 27.10).