Indications
– Physiologic age > 70
– 4 part fractures
– 3 part fractures with severe greater tuberosity comminution
– Articular head-split fractures
Contraindications
– Dementia patients or patients with non-functional deltoid prior to fracture
The fracture pattern also plays a critical role in the decision to proceed with and RSA as the treatment of choice. Four-part fractures, in accordance with Neer’s description, where the greater tuberosity, lesser tuberosity, humeral head, and humeral shaft are separate pieces remains our most common indication for the use of RSA in the elderly patient (Fig. 16.1). However, we will also utilize RSA for complex three-part proximal humeral fractures involving the surgical neck in conjunction with a comminuted greater tuberosity, which we define as a greater tuberosity fractured into three or more fragments (Figs. 16.2 and 16.3). Our concern in this situation is that in a three-part fracture treated with open reduction and internal fixation, or with a hemiarthroplasty, the healing of the greater tuberosity is critical to allow for functional forward elevation and external rotation of the shoulder. Thus, if the greater tuberosity is comminuted into three or more fragments, the likelihood of these multiple fragments healing in an acceptable position in an elderly patient is diminished. For elderly patients with this fracture pattern, use of a RSA warranted, in that, if the greater tuberosity does not heal due to this comminution, the patient still has the chance to regain a good functional outcome with overhead elevation due to the deltoid acting as the prime mover of the shoulder.

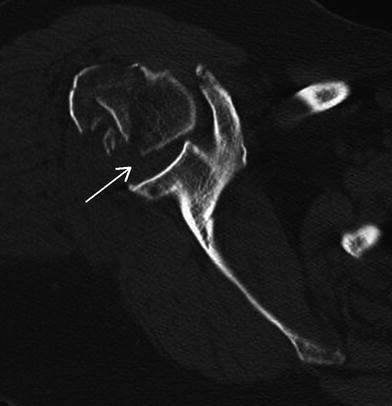
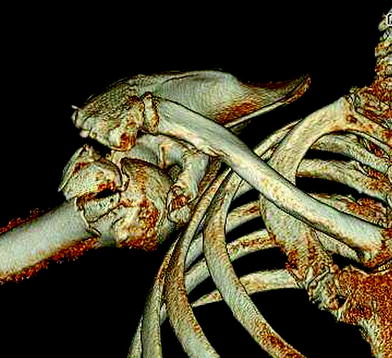

Fig. 16.1
X-ray demonstrating a four-part proximal humerus fracture in a 75-year-old male
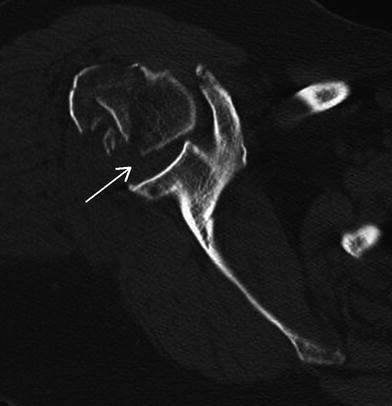
Fig. 16.2
Axial cut of a CT scan demonstrating a three-part fracture dislocation of the proximal humerus involving the surgical neck and greater tuberosity. The greater tuberosity is comminuted in more than two pieces as indicated by the arrow
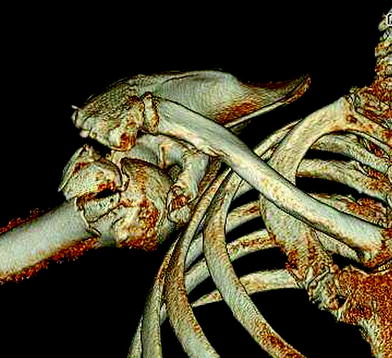
Fig. 16.3
3D reconstruction demonstrating that the greater tuberosity is in 3 pieces
There are contraindications to RSA in the elderly patient population. A functional deltoid muscle is required to power the shoulder after RSA and if prior to their fracture the patients had a poor or a non-functional deltoid due to previous surgeries and deltoid dehiscence, then RSA should not be utilized. If the patient has a past medical history of a prior axillary nerve injury resulting in a non-functional deltoid, then RSA is not indicated. It is critical to differentiate a pre-existing axillary nerve injury from an axillary nerve neuropraxia that may have occurred due to the trauma at the time of the patient’s proximal humeral fracture. Subtle injury to the axillary nerve is common finding after proximal humerus fractures and electromyographic studies done acutely after proximal humeral fractures have demonstrated that 58 % of patients may have altered conduction in the axillary nerve as a result of the injury [14]. Fortunately, follow-up EMG studies demonstrate the nerve recovers in virtually all of these patients, thus even if a patient demonstrates signs of an axillary nerve neuropraxia as a result of their traumatic injury, we still proceed with RSA in this clinical scenario.
The patient’s mental status can serve as a contraindication as well. There is a strict postoperative protocol that patients must follow after their arthroplasty procedure in terms of restrictions with respect to use of the arm. Elderly patients with advanced dementia may not be able to adhere to these restrictions, thus placing themselves at risk for postoperative complications. Patients with a history of advanced dementia are not candidates for RSA in our opinion. Lastly, the patient’s medical comorbidities may serve as a contraindication. Elderly patients may have advanced cardiac or pulmonary issues that preclude them from undergoing a surgical procedure due to the risk involved.
History and Physical
A well-done history and physical is a critical part of the preoperative evaluation. It is important to focus on understanding the mechanism of the injury and what led to the trauma. One must be aware that the elderly patient’s medical co-morbidities could play a role in the injury. A syncopal event or an episode of ischemia is not uncommon in this patient population and could signal underlying medical issues that led to the fracture. Internal medicine consultation is obtained on all patients for whom we are considering surgery in order to determine if they are fit for the procedure, and medically optimized prior to undergoing surgery. The pre-injury function of the shoulder and history of prior shoulder surgery can be helpful to identify rotator cuff tears, deltoid dehiscence, axillary nerve injuries, and arthritis that may influence the choice of procedure.
The physical exam is often limited given the traumatic nature of the patient’s shoulder injury. As stated earlier in this chapter, concomitant neurologic injuries may accompany proximal humeral fractures, therefore, and a careful examination of axillary, musculocutaneous, radial, median, and ulnar nerves of the injured extremity is performed. Axillary nerve function is best assessed by evaluation of the patient’s sensation on the superior-lateral aspect of the upper arm as the nerve supplies cutaneous branches to this area. An axillary nerve neuropraxia does not preclude us from proceeding with surgery; however, it is noted as it may slow the patients’ recovery and restoration of motion given that the deltoid will be the prime mover of the shoulder after surgery. Arterial injuries at the time of proximal humeral fractures are rare but have been reported [15]. A strong radial pulse and normal capillary refill in the injured extremity must be present to proceed with surgery. Lastly, careful palpation the distal humerus, forearm, wrist, and hand to note any other crepitus or tenderness that could indicate a polytraumatized extremity with additional fractures.
Imaging Studies
Our requested radiographic series after suspected proximal humerus fracture consists of a Grashey view (true anteroposterior X-ray of the shoulder), a Y-view, and an attempt at an axillary lateral view. External and internal rotation views of the shoulder are not obtained in a suspected fracture as these maneuvers simply rotate the humeral diaphysis through the surgical neck fracture site causing the patient more pain and adding very little to the radiographic findings. Radiographs of the humerus and elbow are obtained to evaluate for any fractures distal to the proximal humerus. Often times it is difficult to accurately assess the number of fragments and their relative positions with standard two-dimensional radiographs of the shoulder. A computed tomography (CT) scan with three-dimensional reconstructions (Fig. 16.4) is frequently obtained to better elucidate the fracture pattern, and aide in preoperative planning. In our experience, the use of three-dimensional CT scans gives us a better understanding of the severity of the fracture, the position of all fracture fragments, and any potential anterior or posterior dislocation of the humeral head that may have occurred compared to conventional CT scans.
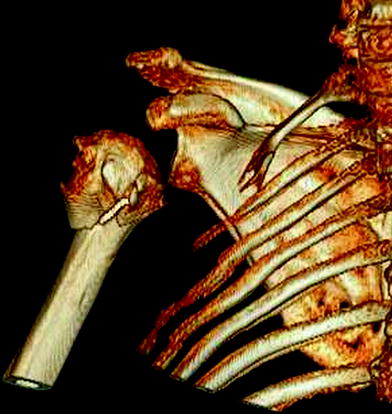
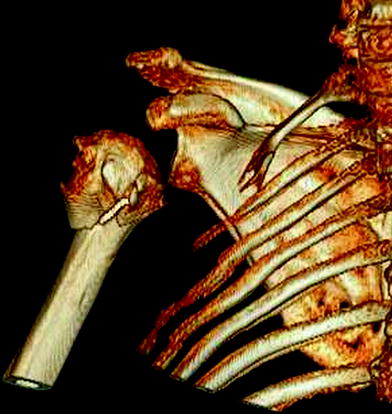
Fig. 16.4
3D reconstruction of a valgus impacted four-part proximal humerus fracture
Surgical Technique
Patient Positioning
The surgery is performed with the patient in the beach chair position with the head of bed at roughly a 60° angle. The entire operative extremity is prepped and draped free. A padded Mayo stand is used to support the forearm. We find that fluoroscopy aids judging the position of our tuberosities at the completion of the surgery and ensuring that they are repaired in a good position with respect to the implant. The fluoroscopy C-arm machine is placed on the ipsilateral side of the table in a rainbow position over the shoulder, fully draped, and included in the surgical field.
Surgical Approach
We utilize a standard deltopectoral approach when performing a RSA for fracture. There typically is significant bleeding and swelling that occurs in conjunction with these fractures and it can be difficult to visualize the interval between the deltoid and pectoralis major. At the superior aspect of the surgical incision, there exists a proximal fat triangle that delineates the interval between the deltoid and pectoralis and is a useful landmark to start the dissection. The interval is split taking the deltoid in a lateral direction and pectoralis major and cephalic vein in a medial direction. Coagulation of the veins feeding into the cephalic vein from the deltoid decreases intraoperative blood loss and facilitates exposure. Care is taken to bluntly release any subdeltoid or subacromial adhesions to fully mobilize these spaces.
The clavipectoral fascia is opened just lateral to the conjoined tendon. The sub-coracoid space is bluntly dissected to fully release this space as well. Next, the long head of the biceps is identified in the bicipital groove. The long head of the biceps serves an important landmark as the fractured greater tuberosity typically lies posterior to the biceps, and if the lesser tuberosity is involved, this lies medial to the long head. The long head of the biceps is exposed proximally to the rotator interval. The biceps tendon is then tenodesed to the upper border of the pectoralis major and the proximal portion resected. With the rotator interval now opened, the humeral head can be grasped with a clamp and removed, typically, as a single fragment.
At this point, the greater tuberosity and the rotator cuff muscles are tagged with four #5 ticron sutures spaced a few millimeters apart and passed at the bone–tendon junction. These will later be used for the tuberosity repair. The lesser tuberosity and attached subscapularis is mobilized and tagged at the bone–tendon junction with another #5 ticron suture. The glenoid is then exposed with retractors place along the anterior, superior, and posterior aspects and due to the absence of the humeral head the glenoid easily visualized in these fracture cases.
Component Placement
The glenosphere component is the first to be placed. We prefer to implant the glenoid in roughly 15° of inferior tilt. In these fracture cases, the glenoid typically has very little wear and the glenoid face often has no significant erosion. The system we utilize has a drill guide that sits on the glenoid face and is angled inferiorly at 15° to produce our desired tilt. The guide is centered on the glenoid and a pilot hole is drilled in a bi-cortical fashion straight down the glenoid vault. The glenoid is then reamed and the glenoid baseplate is implanted. Locking screws further secure the baseplate and then the glenosphere is then impacted on to the glenoid baseplate.
Attention is then turned to the humerus for preparation. The humerus is reamed and broached to estimate the size of the humeral component. Placing the humeral component in the proper height is a key technical point as this effects the soft tissue tension and stability of the implant. The medial calcar is utilized as our reference point and the inferior-medial aspect of the humeral socket should rest directly above the medial calcar (Fig. 16.5) to ensure the proper height of the component. A monoblock humeral component that has proximal suture holes and a porous surface around the humeral socket may aid in tuberosity repair and healing. With respect to version of the humeral component, we typically implant the stem in 30° of retroversion; however, the version that will provided the best results has yet to be studied rigorously. Once trialing is complete, two holes are drilled in the lateral shaft of the humerus to assist in tuberosity repair (see below). The humeral component is then cemented into position.










