Reverse Shoulder Arthroplasty for Acute Proximal Humerus Fractures
Pascal Boileau
Adam P. Rumian
Xavier Ohl
INTRODUCTION
Although Neer reported favorable results following hemiarthroplasty for proximal humeral fractures in 1951, a large number of subsequent studies have been unable to duplicate his functional and radiological outcomes. In fact, most reports of shoulder hemiarthroplasty for fractures of the proximal humerus in the United States document a high incidence of shoulder pain and stiffness (1,2). Many authors have documented that the results of hemiarthroplasty are closely related to the accuracy of reduction and healing of the tuberosities, particularly the greater tuberosity (3). If the greater tuberosity heals in a malunited position or migrates because of fixation failure, a poor outcome is predictable. The critical role of the greater tuberosity is explained by the fact that three of the four rotator cuff muscles insert directly onto it: the supraspinatus, infraspinatus, and teres minor. If the greater tuberosity does not heal properly, then the function of these muscles will be compromised, leading to shoulder dysfunction. Furthermore, malunion or nonunion of the tuberosity can lead to bony impingement with decreased range of shoulder motion, pain, and stiffness.
In reverse shoulder arthroplasty (RSA), the center of rotation of the shoulder joint is medialized and the humerus is lowered, resulting in an increased lever arm with improved function of the deltoid for abduction. The prosthesis is designed to compensate for deficiencies of the rotator cuff, particularly the supraspinatus (4). A RSA is a semiconstrained prosthesis, and insufficiency of the greater or lesser tuberosity will not cause instability of a properly positioned prosthesis. This makes it an attractive option for arthroplasty in fracture cases where successful reconstruction and osteosynthesis of the proximal humerus and tuberosities are problematic. However, its use should be restricted to more elderly patients (i.e., over 70 years of age) as long-term results with this implant are not available, and preliminary studies report deterioration of function after a few years (5). Although RSA can compensate for cuff deficiency as described above, the surgical goal should include reduction, fixation, and healing of the greater tuberosity to preserve the external rotation function of the shoulder whenever possible (6).
INDICATIONS AND CONTRAINDICATIONS
RSA for fracture is reserved for comminuted osteoporotic fractures in elderly patients that are unsuitable for osteosynthesis or conventional hemiarthroplasty. These include four-part fractures and fracture dislocations of the proximal humerus, head-splitting fractures, some three-part fracture dislocations, and three-part fractures without valgus impaction of the humeral head (7,8). Factors that would favor the use of a RSA rather than hemiarthroplasty include age over 70 years, severe osteopenic bone or metabolic bone disease, marked comminution of the fracture, preexisting rotator cuff disease, inflammatory arthritis, heavy smoking, and the use of systemic steroid medication. Contraindications to RSA include age under 70 years, active infection, a complete axillary
nerve deficit, inadequate glenoid bone stock to support a glenoid implant, and inability or unwillingness of the patient to comply with postoperative rehabilatation. RSA for fractures is a technically demanding procedure and should not be performed by inexperienced surgeons without specialized training.
nerve deficit, inadequate glenoid bone stock to support a glenoid implant, and inability or unwillingness of the patient to comply with postoperative rehabilatation. RSA for fractures is a technically demanding procedure and should not be performed by inexperienced surgeons without specialized training.
PREOPERATIVE PLANNING
Preoperative planning is essential to obtain a successful outcome after RSA for fracture and to prevent avoidable complications. A detailed history should be obtained, and a careful physical examination should be performed. The motor and sensory function of the axillary nerve must be accurately assessed because a significant number of patients with proximal humeral fractures have subtle injuries to the nerve. While neurological dysfunction tends to recover slowly, it may delay recovery and rehabilitation. This is especially important since RSA relies on the deltoid muscle to be the prime driver of shoulder movement. In our opinion, RSA should not be performed in a patient with a complete axillary nerve palsy. Radiographic evaluation should include anteroposterior (AP), scapular Y, and axillary lateral views as well as a CT scan to classify the fracture, and determine fracture displacement and evaluate the status of the tuberosities. The CT also allows some evaluation of the rotator cuff as to the degree of fatty infiltration and muscular atrophy as well as the ability to assess the glenoid bone stock to support a glenoid component (9).
We believe that the ideal timing of surgery is at 3 to 7 days after injury, which avoids operating through acutely injured and edematous soft tissues and lessens the risk of wound complications. Surgery after a delay of more than 3 weeks becomes technically difficult due to fracture callus that results in difficulty mobilizing the tuberosity fragments and requires a more extensive soft-tissue dissection.
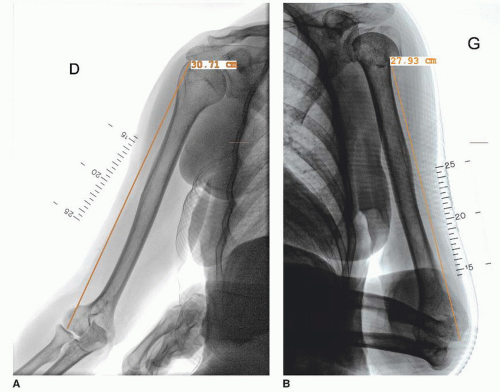
Preoperative radiographic planning is very important if successful outcome is to be consistently achieved. The normal anatomical landmarks that are used as reference points to position the humeral prosthesis are displaced or compromised as a result of the fracture. Correct positioning of the humeral prosthesis, especially in terms of vertical height, is crucial as implanting the prosthesis too deep or too proud in the humeral canal can lead to a poor result (10). In our opinion, it is not acceptable to rely on “eyeballing” the height of the prosthesis at the time of surgery as this leads to unpredictable, unreproducible, and often unacceptable results. Scaled AP radiographs of both humeri should be obtained. The length of the normal humerus is measured along the prosthetic axis as shown in Figure 5.1. On the fractured side, the length of the remaining distal humeral shaft
fragment is measured from the lateral edge of the fracture (Fig. 5.1). The difference between these two measurements, adjusted for the magnification factor, gives the distance above the lateral edge of the distal humeral shaft fragment that the top of the prosthesis needs to be implanted to achieve the correct humeral length.
fragment is measured from the lateral edge of the fracture (Fig. 5.1). The difference between these two measurements, adjusted for the magnification factor, gives the distance above the lateral edge of the distal humeral shaft fragment that the top of the prosthesis needs to be implanted to achieve the correct humeral length.
Patient Setup
Surgery can be performed under a general or regional anesthesia.
Antibiotic prophylaxis should be administered at the time of anesthetic induction according to local protocols. We perform surgery in a laminar airflow room. A beach-chair position is used with the arm draped free. We routinely perform a prescrub with diluted antiseptic scrub lotion before definitively prepping the arm as the patient has often had their arm immobilized for a few days and has been unable to perform adequate hygiene in the axillary region due to pain. The arm must be draped free to allow for intraoperative manipulation to aid in exposure and prosthesis implantation. A sterile adhesive antimicrobial incise drape (Ioban, 3M) is applied to the surgical field after marking the incision to lessen the risk of wound contamination.
We use the Aequalis Reversed Fracture Prosthesis (Aequalis RSAFx, Tornier, Inc.) system. This specifically designed reverse fracture stem has a low-profile monobloc design, proximal hydroxyapatite coating to promote bone healing, a fenestration to accept proximal bone graft, and a smooth polished neck to prevent abrasion of sutures used for tuberosity osteosynthesis (Fig. 5.2). It is also modular as it can accept either a 36 or a 42 polyethylene cup.
Approach
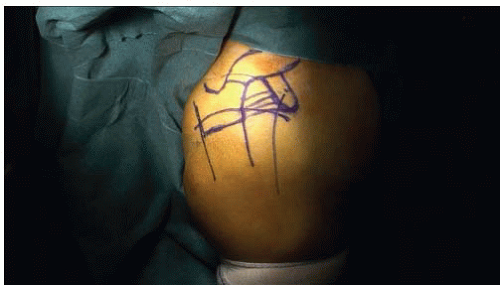
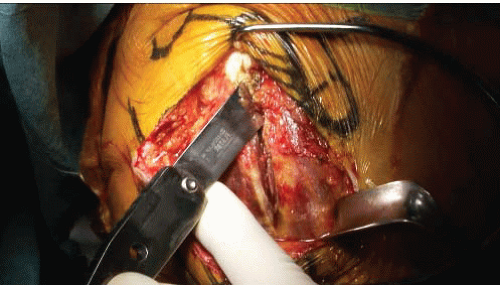
Although we routinely use the deltopectoral approach for elective RSA, we utilise the superolateral deltoid-splitting approach for fracture cases as it allows better access to the greater tuberosity fragments and improves glenoid exposure. A vertical incision centered at the anterior edge of the acromion is made in Langer’s lines, 1 cm medial to its lateral border (Fig. 5.3). Full-thickness skin flaps are raised, exposing the underlying deltoid muscle and anterolateral acromion (Fig. 5.4). The deltoid is split in the avascular tendinous raphe between the anterior and middle portions of the deltoid. This split should not extend more than 5 cm distally to avoid damaging the axillary nerve. Proximally, the split is extended up over the superior surface of the anterior acromion, and we detach 2 cm of the anterior deltoid muscle with a thin piece of bone to improve healing of the deltoid after reattachment (Fig. 5.5). A deep self-retaining retractor is used for improved visualization.
Fracture Exposure
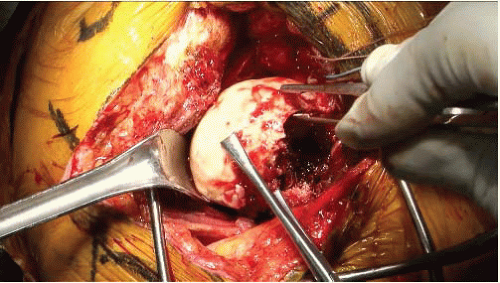
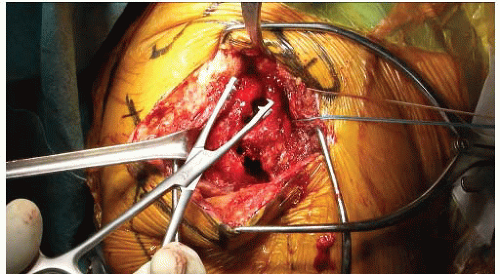
The hemorrhagic subacromial bursa and fracture haematoma are carefully removed, exposing the fracture site. The key to understanding the anatomy is to identify the long head of biceps tendon, which lies between the greater and lesser tuberosities and marks the rotator interval. The rotator cuff interval is opened or extended if torn, and the biceps tendon is identified, tagged, and divided at its origin from the supraglenoid tubercle. We excise its intra-articular portion to aid exposure, facilitate fracture reduction, and remove a source of postoperative pain. A soft-tissue tenodesis below the rotator cuff interval of the remaining tendon is performed. The fractured humeral head is now removed and saved to be used as bone graft in and around the definitive prosthesis (Fig. 5.6).
Tuberosity Mobilization and Preparation
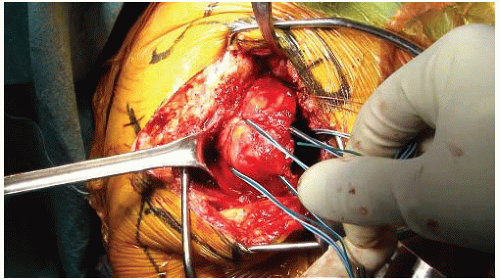
The supraspinatus tendon is identified and mobilized up to the glenoid rim. In many patients, its attachment to the greater tuberosity is already torn, and any adhesions between the rotator cuff muscles and deltoid should be freed. The greater tuberosity fragment is grasped with an atraumatic specifically designed grasping clamp to allow suture placement (Aequalis, Tornier, Inc.; Fig. 5.7). We pass one green and one blue heavy nonabsorbable braided sutures through the infraspinatus tendon and one green and one blue sutures through the teres minor tendon (Fig. 5.8). These four strong nonabsorbable sutures (two green, two blue) will be used as horizontal cerclages for tuberosity fixation and must be placed at the bone-tendon junction of the greater tuberosity. Sutures of different colours are helpful to aid in suture management. We use a combination of Orthocord (Depuy Orthopaedics, Inc.), Fiberwire (Arthrex, Inc.), or Force Fiber (Tornier Inc.). Likewise, two sutures are passed around the lesser tuberosity fragment through the subscapularis tendon.
Using a shuttling suture or a crimping needle, two doubled-over lengths of suture are passed through the superior portion and two of a different color through the inferior portion of the infraspinatus at its junction with the bone. Sutures should not be passed through the bone itself to avoid causing comminution of the tuberosity fragment. Once this step is completed, our attention is turned to the glenoid (Fig. 5.9).
Glenoid Exposure and Implantation
To expose the glenoid, a flat lever forked retractor (Kolbel retractor) is placed over the anterior glenoid neck to retract the subscapularis muscle anteriorly. The anterior and inferior labrum is excised and an anterior juxtaglenoid capsulotomy performed. Similarly, a forked retractor is placed posteriorly and the posterior labrum excised and posterior capsulotomy performed. The glenoid exposure is completed by placing a retractor inferiorly to depress the humeral diaphysis and expose the inferior rim of the glenoid.
The centerpoint of the glenoid is identified by the intersection of the superoinferior and mediolateral bisecting lines. It is desirable to place the glenoid baseplate slightly inferiorly on the glenoid. The circular glenoid guide is placed flush to the inferior rim of the glenoid and used to insert a threaded guide wire. In fracture cases without glenoid wear, it is not necessary to correct glenoid version. The guide wire can be inserted in a neutral position or with 10 degrees of inferior tilt (Fig. 5.10). Any superior tilt of the glenoid implant should be avoided to prevent instability and inferior scapular notching.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree