Retaining Systems and Compartments
Shahan K. Sarrafian
Armen S. Kelikian
GENERAL ORGANIZATION OF THE COMPARTMENTS
The study of the compartments of the distal leg in continuity with the compartments of the ankle and the foot provides a rational approach to their understanding.
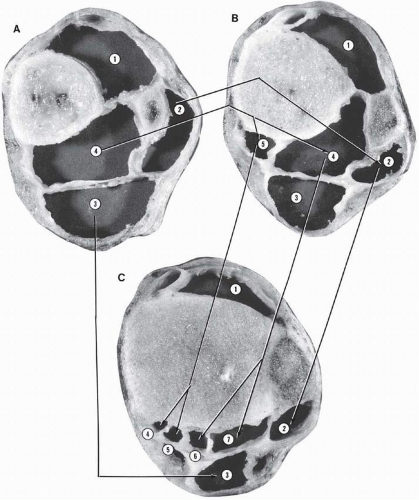
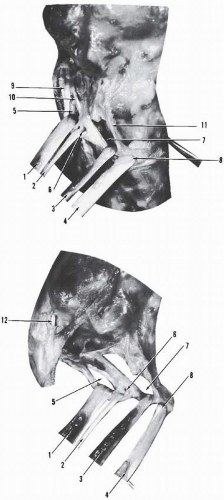
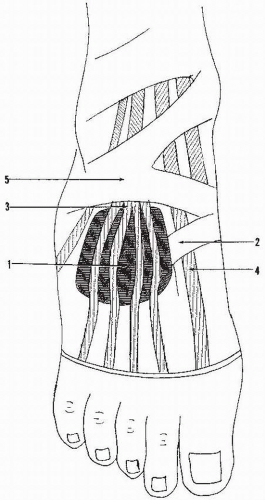
The distal leg has four compartments: anterior, lateral, and posterior, the latter divided into superficial and deep compartments by the deep aponeurosis cruris (Fig. 3.1). The anterior compartment is formed by the anterior surfaces of the tibia and the fibula united by the interosseous membrane, the superficial aponeurosis cruris, and the anterior intermuscular septum. The lateral compartment is formed by the lateral surface of the fibula, the superficial aponeurosis cruris, the anterior intermuscular septum, and the lateral or posterior intermuscular septum. The deep posterior compartment is formed by the posterior surface of the tibia and the posteromedial surface of the fibula united by the interosseous membrane, the lateral intermuscular septum, and the deep aponeurosis cruris posteriorly and the overlapping, adherent segments of the deep and superficial aponeuroses cruris medially. The superficial posterior compartment is formed by the superficial and deep aponeurosis cruris.
Further distally, at 5 cm from the tip of the medial malleolus, the leg is divided into five compartments through the appearance of a subdivision of the deep posterior compartment on the posteromedial aspect.
At the level of the metaphysis and the ankle, the two deep posterior compartments of the leg are in continuity with the four posterior tunnels for the tibialis posterior tendon, the flexor digitorum longus tendon, the posterior tibial neurovascular bundle, and the flexor hallucis longus tendon. The lateral compartment of the leg now forms the tunnel of the peronei tendons and has shifted from a lateral to a posterior position relative to the fibula and the lateral malleolus. The superficial posterior compartment is in continuity with the tunnel of the Achilles tendon, and the anterior compartment of the leg remains as the anterior compartment in front of the distal tibia (see Fig. 3.1).
The anterior compartment is continued distally into the foot as the dorsal compartment of the foot. Posteriorly, the superficial compartment of the Achilles tendon terminates on the posterior aspect of the os calcis. In the deep posterior compartment, there is a diversion: the peroneal tunnel is directed laterally, whereas the tunnels of the tibialis posterior tendon, flexor digitorum longus, posterior tibial neurovascular bundle, and flexor hallucis longus are directed medially into the tibiotalocalcaneal tunnel, which then communicates with the sole of the foot. The tunnel of the peroneus longus tendon penetrates the sole from its lateral border.
Anterior Compartment of the Distal Leg-Ankle and Dorsal Compartment of the Foot
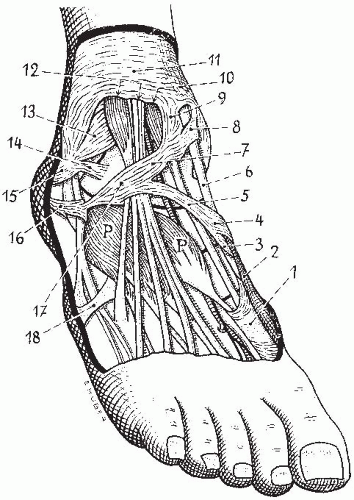
The superficial aponeurosis cruris is reinforced at the level of the distal leg-ankle-tarsus by the superior extensor retinaculum and the inferior extensor retinaculum and continues on the dorsum of the foot as the dorsal aponeurosis reinforced on the dorsomedial aspect of the tarsometatarsal area by a transverse band.
Superior Extensor Retinaculum
The superior extensor retinaculum (ligamentum transversum cruris) is a transverse aponeurotic band formed by the reinforcement of the distal segment of the superficial aponeurosis of the leg (Fig. 3.2). The proximal and distal borders are difficult to delineate and are more or less surgically created. This transverse ligament is attached laterally on the lateral crest of the lower fibula and the lateral surface of the lateral malleolus and medially on the anterior crest of the tibia and the medial malleolus. Laterally, the superior extensor retinaculum is in continuity with the superior peroneal retinaculum, and medially it is in continuity with the apical fibers of the flexor retinaculum.
The long digital extensors, the peroneus tertius tendon and the tibialis anterior tendon, pass under the ligament. In 25% of the cases, there is a separate tunnel for the tibialis anterior tendon, formed by the dissociation of the fibers into a superficial and a deep layer.1 The apical fibers of the flexor retinaculum contribute to the formation of this tunnel by passing superficially and deep to the tibialis anterior tendon before inserting on the deep surface of the transverse ligament. The superomedial band of the inferior extensor retinaculum also provides fibers to the deep layer of the same tunnel.
Inferior Extensor Retinaculum
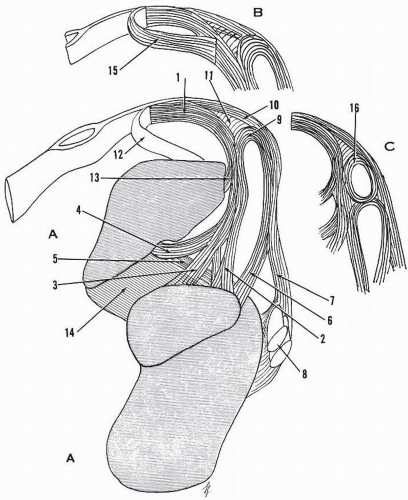
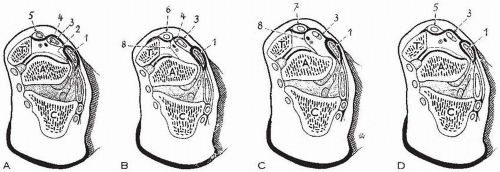
The inferior extensor retinaculum (anterior annular ligament of the tarsus, ligamentum cruciatum of Weitbrecht, frondiform ligament of Retzius, ligamentum lamboideum) is a Y- or X-shaped retaining structure located on the anterior aspect of the tarsus
and the ankle (Figs. 3.23.3, 3.4, 3.5, and 3.6).1, 2, 3, 4, 5, 6 It is a complex structure that has four components: the stem or frondiform ligament, the oblique superomedial band, the oblique inferomedial band, and the oblique superolateral band.
and the ankle (Figs. 3.23.3, 3.4, 3.5, and 3.6).1, 2, 3, 4, 5, 6 It is a complex structure that has four components: the stem or frondiform ligament, the oblique superomedial band, the oblique inferomedial band, and the oblique superolateral band.
Stem or Frondiform Ligament
The stem or frondiform ligament is a sling ligament retaining the tendons of the extensor digitorum longus and peroneus tertius against the talus and the calcaneus. This ligament has three roots: lateral, intermediary, and medial.
The lateral root is superficial, originates in the sinus tarsi lateral to the origin of the extensor digitorum brevis muscle, and blends with the deep fascia and the inferior peroneal retinaculum. The boundaries of this superficial root are difficult to delineate by dissection; tensing of the extensor tendons or inversion of the foot facilitates recognition of its borders.
The intermediary root arises from the sinus tarsi medial to the origin of the extensor digitorum brevis muscle and just posterior to the origin of the cervical ligament. At times, this root is fasciculated, and one large fascicle may divide the origin of the extensor hallucis brevis from that of the lesser toes.
The intermediary root extends upward and unites with the lateral root, forming the superficial component of the stem of the inferior extensor retinaculum. Once formed, the stem courses obliquely upward and inward across the neck of the talus. It passes over the peroneus tertius and extensor digitorum longus tendons and bifurcates into the oblique superomedial and inferomedial bands.
The medial root completes the formation of the retinacular sling for the extensor digitorum longus tendons and the peroneus tertius and forms the deep part of the stem. It has three components: two calcaneal (lateral and medial) and one talar.
The lateral calcaneal component is formed by vertical fibers and inserts in the sinus tarsi just posterior to the intermediary root and establishes connection at this level. The major medial calcaneal component enters the tarsal canal very obliquely and inserts on the floor of the canal along its longitudinal axis, usually anterior to the ligament of the tarsal canal. The fibers of the ligament are oriented downward and laterally, whereas those of the medial calcaneal root are oriented downward and medially, forming an “X.”
The talar component of the medial root attaches to the talus on the roof of the tarsal canal, joining the insertion fibers of the ligament of the tarsal canal. Arcuate fibers with inferior concavity unite the two calcaneal components of the medial root. An oblique band of the medial root originates at the calcaneal attachment of the intermediate root, extends medially upward, and joins the talar insertion of the ligament of the tarsal canal. This ligament has been described by Smith and, more recently, by Cahill, who named it the oblique talocalcaneal band.3, 4
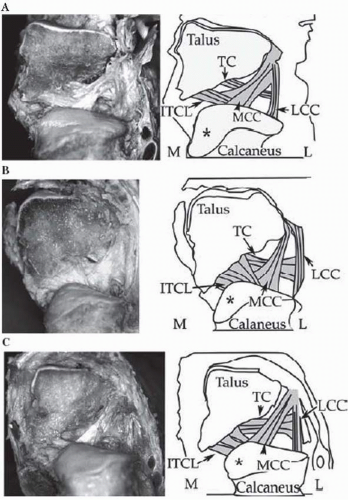
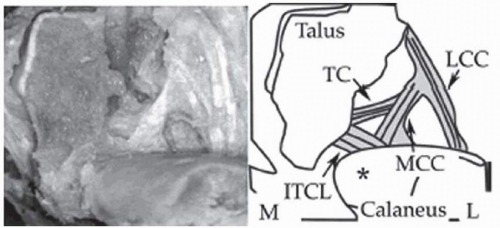
Jotoku et al.,7 in a study of 40 dissected feet, analyzed the variations of the ligaments of the sinus tarsi and canal. The anterior capsular ligament of the posterior talocalcaneal joint is present in 95%. The interosseous talocalcaneal ligament is present in 100%. In 92.5%, the ligament is bandlike: flat and thick. In 5%, the ligament is fanlike: broad at the origin in the tarsal canal and narrower at the insertion at the tarsal canal of the calcaneus. In 2.5%, the ligament is multiple type with three distinct bands (Fig. 3.7). In studying the components of the medial root of the extensor retinaculum, the lateral calcaneal branch is present in 100%, the medial calcaneal component is present in 100%, it is bandlike in 95%, and it is fanlike in 5%. The talar component is defined as the branch of the medial root attaching to the talus and is present in 90%. In type 1 (92%), it originates from the lateral calcaneal root of the inferior extensor retinaculum, and in type 2 (8%), it originates from the medial calcaneal root of the inferior extensor retinaculum. The ligament runs transversely or obliquely and inserts on the talus near the insertion of the interosseous talocalcaneal ligament (Fig. 3.8).
The medial root, ascending upward and medially, is applied against the lateral aspect of the talar neck. It passes anterior to the insertion of the anterior talofibular ligament. A bursa may be interposed between the two structures in 50% to 80% of the cases. Occasionally, instead of the bursa, one finds adipose tissue or even a fibrous band of attachment.
After crossing the superior surface of the talar neck, the medial root forms a loop, joins the deep surface of the stem, and completes the sling for the extensor digitorum longus and peroneus tertius tendons. The internal architecture of the
frondiform ligament and some of its variations are depicted in Figure 3.9.
frondiform ligament and some of its variations are depicted in Figure 3.9.
Oblique Superomedial Band
The oblique superomedial band continues the direction of the stem, passes over the tendon of the extensor hallucis longus and under the tendon of the tibialis anterior, and inserts on the anterior aspect of the medial malleolus. Occasionally, the insertion fans out and reaches the anterior tibial crest and the medial surface of the medial malleolus, interchanging fibers with the superior extensor retinaculum and the flexor retinaculum (Fig. 3.10).
On the medial border of the extensor hallucis longus tendon, the deep fibers of the superomedial band loop around the tendon in a recurrent manner and have a variable insertion (Fig. 3.11). They insert on the apex of the lateral sling or on the deep surface of the medial root in 50% of cases, on the anterior aspect of the talar neck in 25% of cases (Fig. 3.12), or on the lateral sling and the anterior aspect of the talar neck in 25% of cases.1 In the latter cases, the tendon of the extensor hallucis longus and the anterior neurovascular bundle are in the same compartment. Exceptionally, the deep layer of this segment of the retinaculum is absent.
Further medially, at the level of the tibialis anterior tendon, there is a bifurcation of the superomedial band, forming superior and inferior retention systems. The superior tunnel has a thick, deep wall and a very thin or even absent superficial wall. The inferior tunnel is well formed, with insertional fibers reaching the medial malleolus or occasionally blending with the fibers of the inferior arm of the extensor retinaculum.
Oblique Inferomedial Band
The oblique inferomedial band arises from the apex of the lateral sling, advances inferomedially, and reaches the medial border of the foot at the level of the cuneo1-navicular joint. During its course, the 1-cm- to 2-cm-wide band passes over the dorsalis pedis vessels, the deep peroneal nerve, and the extensor hallucis longus tendon. At the level of the tibialis anterior tendon, most of the fibers pass superficial to the tendon, and the remaining fibers slide under the tendon, forming a
tunnel. The terminal segment splits to envelop the abductor hallucis muscle; deep fibers insert on the navicular and the medial cuneiform.
tunnel. The terminal segment splits to envelop the abductor hallucis muscle; deep fibers insert on the navicular and the medial cuneiform.
The level of division of the inferior extensor retinaculum into the oblique superomedial and inferomedial band is variable; it may be lateral to the extensor hallucis longus tendon, medial to the extensor hallucis longus tendon, or medial to the tibialis anterior tendon. The last is the least frequent, and when it occurs, the two division bands are in continuity except for a short distance on the medial aspect of the tibialis anterior tendon.1
Oblique Superolateral Band
The oblique superolateral band, when present, gives a cruciate configuration to the inferior extensor retinaculum, as described by Weitbrecht.2 This band is present in 25% of cases, but the size varies considerably, from 2 to 25 mm.1 It originates from the lateral sling, from the superomedial band, or from both. The band is directed upward and laterally, crosses the anterior tibiofibular ligament, and inserts on the lateral surface of the lateral malleolus and the lateral crest of the lower segment of the fibula. The fibers blend with those of the superior extensor and the superior peroneal retinacula.
DORSAL APONEUROSIS AND DORSAL COMPARTMENTS OF THE FOOT
A comprehensive study of the dorsal aponeurosis of the foot and the dorsal compartment (Fig. 3.13) is presented by Bellocq and Meyer.8
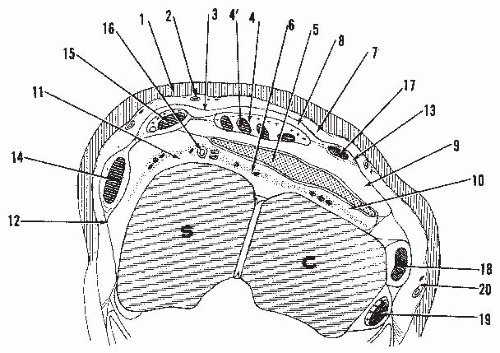
As one dissects the dorsum of the foot and removes the skin, a very thin layer of connective tissue is encountered—fascia superficialis—covering the superficial sensory nerves and veins. Next is a semitransparent, relatively thin fascia located under the superficial nerves and veins, investing all the musculotendinous units of the dorsum of the foot. This layer is the superficial
lamina or superficial dorsal aponeurosis. A true osteofascial space (the spatium dorsalis pedis) is created as this aponeurosis inserts on the foot skeleton at the lateral and medial margins. More precisely, the lateral insertion is on the os calcis, the cuboid, and the tuberosity and lateral border of the fifth metatarsal, and the medial insertion extends from the sustentaculum tali to the tuberosity of the scaphoid and the medial border of the first metatarsal.
lamina or superficial dorsal aponeurosis. A true osteofascial space (the spatium dorsalis pedis) is created as this aponeurosis inserts on the foot skeleton at the lateral and medial margins. More precisely, the lateral insertion is on the os calcis, the cuboid, and the tuberosity and lateral border of the fifth metatarsal, and the medial insertion extends from the sustentaculum tali to the tuberosity of the scaphoid and the medial border of the first metatarsal.
This superficial dorsal aponeurosis extends fibers to the chorion of the skin, thus forming the retinacula cutis, and closes the subcutaneous space of the foot at its margins. Other connective fibers reach the sheath of the abductor of the big toe medially and the abductor of the little toe laterally.
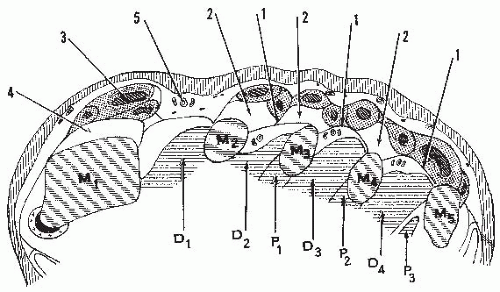
The dorsal osteoaponeurotic space is subdivided into four gliding subspaces by three layers of tissue.
The first layer, located under the superficial dorsal aponeurosis, is formed by the tendons of the tibialis anterior, extensor hallucis longus, extensor digitorum longus, and peroneus tertius, surrounded by synovial sheaths or loose connective tissue united to each other. This superficial tendinoconnective layer unites with the superficial dorsal aponeurosis near the tibialis anterior medially and the outer aspect of the peroneus tertius laterally.
The second layer is formed by the extensor digitorum brevis and its investing fascia, the deep lamina of the dorsal aponeurosis. This aponeurosis attaches medially to the synovial sheath of the extensor hallucis longus. It courses laterally, passes over the dorsalis pedis vessels, and splits into two layers at the medial border of the extensor digitorum brevis. The thick superficial layer and the thin deep layer merge on the lateral border of the muscle and attach laterally on the superficial dorsal aponeurosis and the tarsus.
The third layer is adipoconnective, carrying the dorsalis pedis artery and the accompanying veins and the deep peroneal nerve and its branches. The dorsal interosseous aponeurosis is the last investing layer covering the metatarsals and the interossei muscles.
The four fascial spaces of the dorsal fibro-osseous compartment of the foot located between the previously described three soft-tissue layers and the dorsal aponeurosis are as follows:
Space 1: Located between the superficial dorsal aponeurosis and the superficial tendinoconnective layer
Space 2: Located between the superficial tendinoconnective layer and the extensor digitorum brevis
Space 3: Located between the deep surface of the extensor digitorum brevis with its investing fascia and the neurovascular adipoconnective layer
Space 4: Located between the neurovascular adipoconnective layer and the tarsal osteoarticular layer proximally and the dorsal interosseous aponeurosis distally.
Space 2 has been investigated by Latarjet and Etienne-Martin with injection studies.9 When distended, this space is well delineated, located under the layer formed by the long extensor tendons of the second, third, fourth, and fifth toes and the extensor digitorum brevis. This space is in the form of a trapezoid, with the small base proximal and the large base distal (Fig. 3.14). The proximal border does not reach the inferior extensor retinaculum, but variations are possible. The distal border is located in the middle of the dorsum of the foot and may send extensions under the tendons; this border has a variable location. Medially, the distended bursa reaches the tendon of the extensor hallucis longus but does not lift the latter.
In the distal segment at the level of the base of the metatarsals, the tendons are located in a fibrous sheath, with surrounding loose connective tissue or synovial sheaths. As the tendinoconnective superficial and deep layers are converted into fibrous sheaths, they adhere to the dorsal interosseous aponeurosis or remain separate from it, delineating fibroadipose small spaces (Fig. 3.15).
The superficial dorsal aponeurosis is reinforced along the medial and lateral borders of the foot by two aponeurotic transverse bands: medial and lateral (see Fig. 3.3).1 The medial transverse band originates from the medial cuneiform and metatarsal1 bones and may form a terminal fibrous tunnel for the tibialis anterior tendon. Directed laterally, the fibers pass under the inferior arm of the extensor aponeurosis but over the tendon of the extensor hallucis longus and occasionally over the tendon of the extensor hallucis brevis. The transverse fibers terminate on the cuneiforms and the first metatarsal. Occasionally, the metatarsal insertion may extend up to the level of the metatarsophalangeal joint and form an osteofibrous tunnel for the two extensor tendons.1
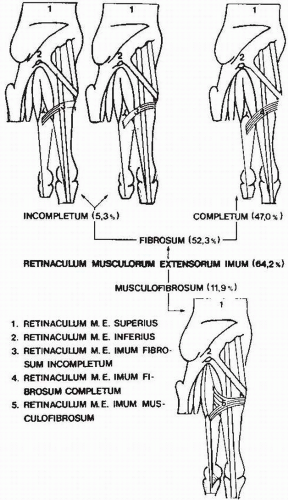
Kaneff and colleagues reported on the occurrence of the retinaculum musculorum imum in man.10 This is a transverse or oblique extensor retinacular band that is present distal to the anteroinferior band of the inferior extensor retinaculum. It originates from the dorsum of the base of the second metatarsal, passes over the tendons of the extensor hallucis longus and brevis, and inserts on the medial side of the first cuneiform. It may also insert on a variant muscle of the first interspace. This retinaculum musculorum extensorium imum was present in 64.2% of 151 dissected specimens. The fibrous forms accounted for 52.3%, and the complete fibrous form accounted for 47%. In 5.3%, there was an incomplete fibrous form with the lateral or medial half missing. The musculofibrosum form—with muscular origin—occurred in 11.9% (Fig. 3.16).
The lateral transverse band is inconstant and located at the level of the base of the fifth metatarsal bone. It originates from the latter, bridges over the metatarsal or digital extensions of the peroneus tertius or the peroneus brevis tendon, and inserts on the fifth or the fourth metatarsal.
Peroneal Tunnels and Retinaculum
Superior Peroneal Tunnel
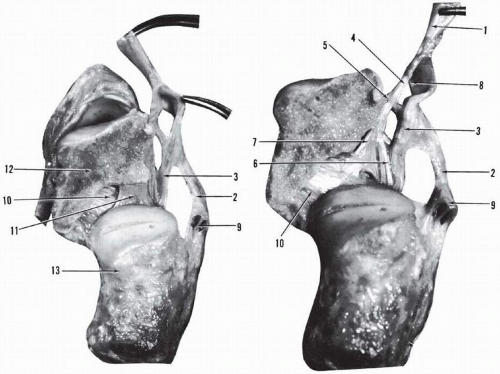
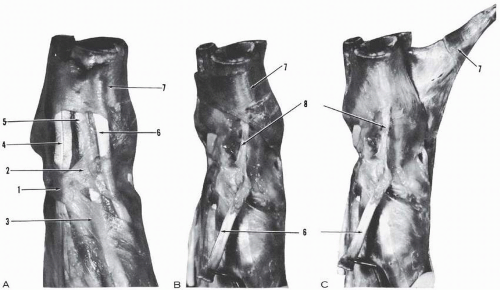
The superior peroneal tunnel is the continuation of the lateral compartment of the leg, which gradually shifts from the lateral position in the distal leg to the posterior aspect of the fibula and remains as a tunnel on the posterior aspect of the lateral malleolus (Figs. 3.1 and 3.17). The covering peroneal aponeurosis takes insertion on the medial and lateral retromalleolar surface or groove and forms a strong retaining aponeurotic ring. The deep aponeurosis of the posterior compartment takes insertion along the medial border of the peroneal tunnel, which may give origin at this junction to the peroneotalocalcaneal ligament of Rouvière and Canela Lazaro. The calcaneal arm of this ligament inserts nearly transversely on the entire width of the superior surface of the calcaneus and may reach the tip of the lateral malleolus and even the insertion of the calcaneofibular ligament.
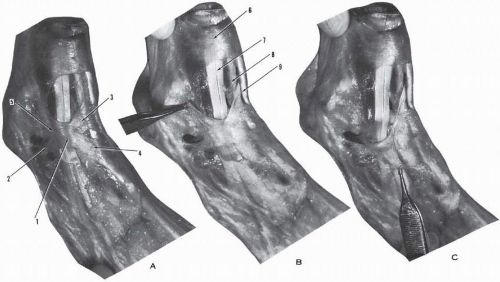
Superior Peroneal Retinaculum
The superior peroneal retinaculum is a reinforcement of the aponeurosis cruris in the form of an obliquely oriented
quadrilateral lamina. It originates from the lateral border of the retromalleolar groove and the tip of the lateral malleolus. It is adherent to the underlying inferior segment of the superior peroneal tunnel and courses obliquely downward and posteriorly. It inserts on the aponeurosis of the Achilles tendon and the posterior aspect of the lateral calcaneal surface.
quadrilateral lamina. It originates from the lateral border of the retromalleolar groove and the tip of the lateral malleolus. It is adherent to the underlying inferior segment of the superior peroneal tunnel and courses obliquely downward and posteriorly. It inserts on the aponeurosis of the Achilles tendon and the posterior aspect of the lateral calcaneal surface.
The sural nerve, the short saphenous vein, and the lateral calcaneal nerve and vessels are located under this superior peroneal retinaculum in their own compartment (see Fig. 3.17).
Intermediary Peroneal Tunnel
Below the tip of the lateral malleolus, the peroneal tunnel obliquely crosses the calcaneofibular ligament and is covered by a thin aponeurosis that is nearly transparent.
Inferior Peroneal Tunnel and Retinaculum
The inferior peroneal retinaculum is in continuity with the lateral root of the inferior extensor retinaculum (Fig. 3.18). It originates from
the posterior segment of the lateral rim of the sinus tarsi. The superficial fibers are oriented downward and posteriorly, cross the trochlear process, and insert on the lateral surface of the os calcis just above the posterolateral tubercle. The deep layer attaches on the apex of the trochlear process. It provides superior and inferior arciform fibers and forms two fibrous tunnels over the superior and inferior surfaces of the trochlear process (Fig. 3.19). The upper tunnel lodges the peroneus brevis tendon, and the lower tunnel lodges the peroneus longus tendon.
Distal to the bony eminence, the inferior peroneal retinaculum forms two nearly circular separate fibrous tunnels for the peronei tendons.
The tunnel of the peroneus longus penetrates the sole of the foot through the lateral border and continues up to its insertion on the base of the first metatarsal and first cuneiform.
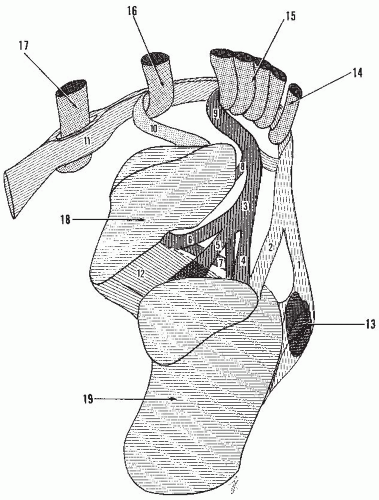
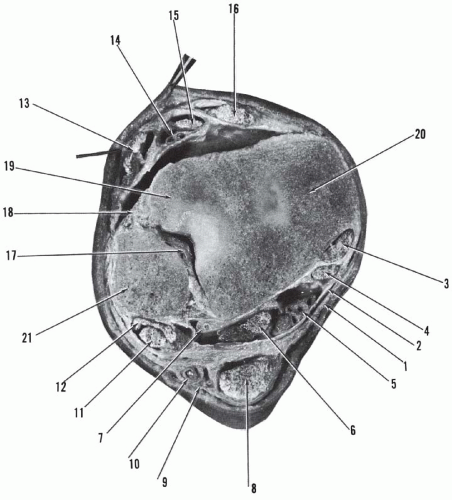
TIBIOTALOCALCANEAL TUNNEL
The tibiotalocalcaneal tunnel (Richet’s tunnel, tarsal tunnel, calcaneal tunnel), a major passageway, extends from the distal end of the tibia to the level of the plantar aspect of the navicular.11, 12, 13, 14 It is posteromedial in location and is concave anteriorly. The tunnel may be divided into two components: upper, tibiotalar, and lower, talocalcaneal.
Upper Tibiotalar Tunnel
The upper tibiotalar tunnel (Figs. 3.203.21, and 3.22




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree