Radius and Ulna Shaft
EPIDEMIOLOGY
Forearm fractures are more common in men than women, secondary to the higher incidence in men of motor vehicle collisions (MVC) and motorcycle accidents (MCA), contact athletic participation, altercations, and falls from a height.
The ratio of open fractures to closed fractures is higher for the forearm than for any other anatomic area except the tibia.
ANATOMY
The forearm acts as a ring; a fracture that shortens either the radius or the ulna results either in a fracture or a dislocation of the other forearm bone at the proximal or distal radioulnar joint. Direct injuries (“nightstick”) are an exception.
The ulna, which is relatively straight, acts as an axis around which the laterally bowed radius rotates in supination and pronation. A loss of supination and pronation may result from radial shaft fractures in which the lateral curvature (“radial bow”) has not been restored.
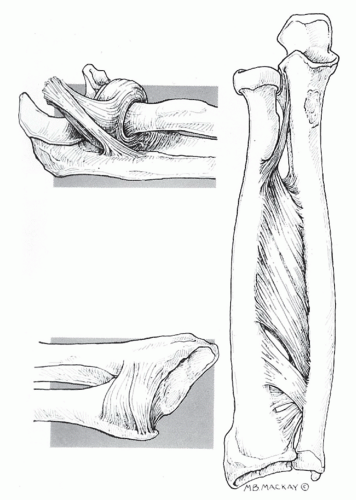
The interosseous membrane occupies the space between the radius and ulna. The central band is approximately 3.5-cm wide running obliquely from its proximal origin on the radius to its distal insertion on the ulna. Sectioning of the central band alone reduces stability by 71% (Fig. 21.1).
Fracture location dictates deforming forces:
Radial fractures distal to the supinator muscle insertion but proximal to the pronator teres insertion tend to result in supination of the proximal fragment owing to unopposed pull of the supinator and biceps brachii muscles.
Radial fractures distal to the supinator and pronator teres muscles tend to result in neutral rotational alignment of the proximal fragment.
FRACTURES OF BOTH THE RADIUS AND ULNA SHAFTS
Mechanism of Injury
These fractures are most commonly associated with high-energy (MVC, MCA) accidents, although they are also commonly caused by direct trauma (while protecting one’s head), gunshot wounds, and falls either from a height or during athletic competition.
Pathologic fractures in this area are uncommon.
Clinical Evaluation
Patients typically present with gross deformity of the involved forearm, pain, swelling, and loss of hand and forearm function.
A careful neurovascular examination is essential, with assessment of radial and ulnar pulses, as well as median, radial, and ulnar nerve function.
One must carefully assess open wounds because the ulna border is subcutaneous, and even superficial wounds can expose the bone.
Excruciating or unremitting pain, tense forearm compartments, or pain on passive stretch of the fingers should raise suspicions of impending or present compartment syndrome. Compartment pressure monitoring should be performed, with urgent fasciotomy indicated for diagnosed compartment syndrome.
Radiographic Evaluation
Anteroposterior (AP) and lateral views of the forearm should be obtained, with oblique views obtained as necessary for further fracture definition.
Radiographic evaluation should include the ipsilateral wrist and elbow to rule out the presence of associated fracture or dislocation (e.g., Monteggia, Galeazzi).
The radial head must be aligned with the capitellum on all views.
Classification
Descriptive
Closed versus open
Location
Comminuted, segmental, multifragmented
Displacement
Angulation
Rotational alignment
Orthopaedic Trauma Association Classification of Fractures of the Radial and Ulna Shaft
See Fracture and Dislocation Compendium at http://ota.org/compendium/index.htm.
Treatment
Nonoperative
Operative
Because the forearm can be considered a “joint,” responsible for motion, open reduction and internal fixation is the procedure of choice for displaced forearm fractures involving the radius and ulna in adults.
Patient positioning is supine with the extremity on a radiolucent hand table.
An anterior (volar, Henry approach) or posterior (dorsal, Thompson) approach may be used for radius shaft fixation. The advantage of a posterior approach is that it allows for the identification of the posterior interosseous nerve (PIN) in the supinator for proximal radius fractures. The anterior approach is advantageous for fractures which extend into the distal metaphysis.
Internal fixation involves use of compression plating (3.5-mm dynamic compression [DC] plate) with or without bone grafting.
Principles of plate fixation:
Restore ulnar and radial length (prevents subluxation of either the proximal or distal radioulnar joint).
Restore rotational alignment.
Restore radial bow (essential for rotational function of the forearm).
The ulna may be plated on either the volar or dorsal aspect, depending on the location of the fragments and contour of the ulna surrounding the fracture site. Using two separate incisions decreases the incidence of radioulnar synostosis.
One should consider acute grafting if substantial comminution or bone loss exists.
Use of bridge plating for comminuted fractures, with minimization of soft tissue disruption, may reduce the need for acute bone grafting.
Open fractures may receive primary open reduction and internal fixation after debridement, except in severe open injuries. This approach restores stability, limits dead space, and improves wound care. The timing of bone grafting of open fractures is controversial; it can be performed at the time of delayed primary closure or at 6 weeks after injury.
External fixation may be used in cases with severe bone or soft tissue loss, gross contamination, infected nonunion, or in cases of open elbow fracture-dislocations with soft tissue loss.
Good results have been reported with locked intramedullary nail fixation. However, the indications for intramedullary nailing over plate and screws have not been clearly defined. This procedure is technically more demanding. Some of the reported indications are segmental fractures, open fractures with bone or soft tissue loss, pathologic fractures, and failed plate fixation.
Complications
Nonunion and malunion: These are uncommon, most often related to infection and errors of surgical technique. Patients may require removal of hardware, bone grafting, and revision internal fixation.