Proximal Humerus Fractures
EPIDEMIOLOGY
Proximal humerus fractures comprise 4% to 5% of all fractures and represent the most common humerus fracture (45%).
The incidence is 300,000 per year (more common than hip fracture).
Most (85%) are nondisplaced.
Older individuals have a higher incidence secondary to osteoporosis.
Proximal humerus fracture in an older individual after a simple fall is considered a fragility fracture.
The 2:1 female-to-male ratio is also related to osteoporosis.
ANATOMY
The shoulder has the greatest range of motion of any joint in the body, secondary to the shallow glenoid fossa that is only 25% the size of the humeral head. The major contributor to stability is not bone, but the soft tissue envelope composed of muscle, capsule, and ligaments.
The proximal humerus is retroverted 35 to 40 degrees relative to the epicondylar axis.
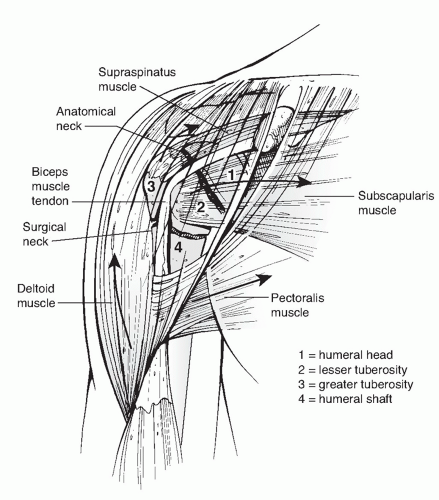
The four osseous segments (Neer) (Fig. 15.1) are the:
1. Humeral head
2. Lesser tuberosity
3. Greater tuberosity
4. Humeral shaft
The deforming muscular forces on the proximal humerus include (Fig. 15.1):
1. The supraspinatus and external rotators displace the greater tuberosity superior and posterior.
2. The subscapularis displaces the lesser tuberosity medially.
3. The pectoralis major displaces the humeral shaft medially.
4. The deltoid abducts the proximal fragment.
Neurovascular supply:
1. The major blood supply is from the anterior and posterior humeral circumflex arteries.
2. The arcuate artery is a continuation of the ascending branch of the anterior humeral circumflex. It enters the bicipital groove and supplies most of the humeral head. Small contributions to the humeral head blood supply arise from the posterior humeral circumflex, reaching the humeral head via tendo-osseous anastomoses through the rotator cuff. Fractures of the anatomic neck are uncommon, but they tend to have a poorer prognosis because of the precarious vascular supply to the humeral head.
3. The axillary nerve courses just anteroinferior to the glenohumeral joint, traversing the quadrangular space. It is at particular risk for traction injury owing to its relative rigid fixation at the posterior
cord and deltoid as well as its proximity to the inferior capsule where it is susceptible to injury during anterior dislocation and anterior fracture-dislocation.
MECHANISM OF INJURY
The most common mechanism is a fall onto an outstretched upper extremity from a standing height, typically in an older woman.
Younger patients typically sustain a proximal humeral fracture following high-energy trauma, such as a motor vehicle accident. These usually represent more severe fractures and dislocations, with significant associated soft tissue disruption and multiple injuries.
Less common mechanisms include:
1. Excessive shoulder abduction in an individual with osteoporosis, in which the greater tuberosity prevents further rotation
2. Direct trauma, usually associated with greater tuberosity fractures
3. Electrical shock or seizure
4. Pathologic processes: malignant or benign processes in the proximal humerus
CLINICAL EVALUATION
Patients typically present with the arm held closely to the chest by the contralateral hand, with shoulder pain, swelling, tenderness, painful range of motion, and variable crepitus.
Ecchymosis about the proximal humerus may not be apparent immediately after injury. Chest wall and flank ecchymosis may be present and should be differentiated from thoracic injury.
A careful neurovascular examination is essential, with particular attention to axillary nerve function. This may be assessed by the presence of sensation on the lateral aspect of the proximal arm overlying the deltoid. Motor testing is usually not possible at this stage secondary to pain. Inferior translation of the distal fragment may result from deltoid atony and is not a true glenohumeral dislocation; this usually resolves by 4 weeks after fracture, but if it persists, it may represent a true axillary nerve injury.
RADIOGRAPHIC EVALUATION
A shoulder series, consisting of an anteroposterior and lateral (“Y”) views in the scapular plane as well as an axillary, is standard.
The axillary is the best view for evaluation of glenoid articular fractures and reduction of the glenohumeral articulation, but it may be difficult to obtain because of pain. This view does not accurately predict fracture angulation in the trauma setting.
Velpeau axillary: If a standard axillary cannot be obtained because of pain or fear of fracture displacement, the patient may be left in the sling and leaned obliquely backward 45 degrees over the cassette. The beam is directed caudally, orthogonal to the cassette, resulting in an axillary view with magnification (Fig. 15.2).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree