Patella and Extensor Mechanism Injuries
PATELLAR FRACTURES
Epidemiology
Represent 1% of all skeletal injuries
Male-to-female ratio 2:1
Most common age group 20 to 50 years old
Bilateral injuries uncommon
Anatomy
The patella is the largest sesamoid bone in the body.
The quadriceps tendon inserts on the superior pole and the patellar ligament originates from the inferior pole of the patella.
There are seven articular facets; the lateral facet is the largest (50% of the articular surface).
The articular cartilage may be up to 1-cm thick.
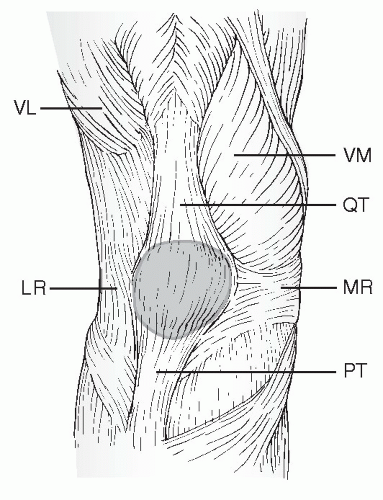
The medial and lateral extensor retinacula are strong longitudinal expansions of the quadriceps and insert directly onto the tibia. If these remain intact in the presence of a patella fracture, then active extension will be preserved (Fig. 35.1).
The function of the patella is to increase the mechanical advantage and leverage of the quadriceps tendon, aid in nourishment of the femoral articular surface, and protect the femoral condyles from direct trauma.
The blood supply arises from the geniculate arteries, which form an anastomosis circumferentially around the patella.
Mechanism of Injury
Direct: Trauma to the patella may produce incomplete, simple, stellate, or comminuted fracture patterns. Displacement is typically minimal owing to preservation of the medial and lateral retinacular expansions. Abrasions over the area or open injuries are common. Active knee extension may be preserved.
Indirect (most common): This is secondary to forcible eccentric quadriceps contraction while the knee is in a semiflexed position (e.g., in a “stumble” or “fall”). The intrinsic strength of the patella is exceeded by the pull of the musculotendinous and ligamentous structures. A transverse fracture pattern is most commonly seen with this mechanism, with variable inferior pole comminution. The degree of displacement of the fragments suggests the degree of retinacular disruption. Active knee extension is usually lost.
Combined direct/indirect mechanisms: These may be caused by trauma in which the patient experiences direct and indirect trauma to the knee, such as in a fall from a height.
Clinical Evaluation
Patients typically present with limited or no ambulatory capacity with pain, swelling, and tenderness of the involved knee. A defect at the patella may be palpable.
It is important to rule out an open fracture because these constitute a surgical urgency; this may require instillation of more than 100 mL of saline into the knee to determine communication with overlying lacerations.
Active knee extension should be evaluated to determine injury to the retinacular expansions. This may be aided by decompression of hemarthrosis or intra-articular lidocaine injection.
Associated lower extremity injuries may be present in the setting of high-energy trauma. The physician must carefully evaluate the ipsilateral hip, femur, tibia, and ankle, with appropriate radiographic evaluation, if indicated.
Radiographic Evaluation
Anteroposterior (AP) and lateral views of the knee should be obtained.
AP view: A bipartite patella (8% of the population) may be mistaken for a fracture; it usually occurs in the superolateral position and has smooth margins; it is bilateral in 50% of individuals.
Lateral view: Displaced fractures usually are obvious.
Axial view (sunrise): This may help identify osteochondral or vertical marginal fractures. This view may be difficult to obtain in the acute setting, however.
Computed tomography scanning may be used to better delineate fracture patterns, marginal fractures, or free osteochondral fragments.
CLASSIFICATION
Descriptive
Open versus closed
Nondisplaced versus displaced
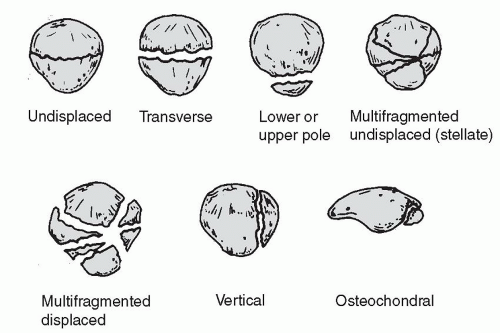
Pattern: stellate, comminuted, transverse, vertical (marginal), polar osteochondral (Fig. 35.2)
Orthopaedic Trauma Association Classification of Patellar Fractures
See Fracture and Dislocation Classification Compendium at http://www.ota.org/compendium/compendium.html.
Treatment
Nonoperative
Indications include nondisplaced or minimally displaced (2 to 3 mm) fractures with minimal articular disruption (1 to 2 mm). This requires an intact extensor mechanism.
A cylinder cast or knee immobilizer is used for 4 to 6 weeks. Early weight bearing in extension is encouraged, advancing to full weight bearing with crutches as tolerated by the patient. Early straight leg raising and isometric quadriceps strengthening exercises should be started within a few days. After radiographic evidence of healing, progressive active flexion and extension strengthening exercises are begun with a hinged knee brace initially locked in extension for ambulation.
Operative
Open Reduction and Internal Fixation
Indications for open reduction and internal fixation include loss of active extension, an extensor lag, >2-mm articular incongruity, >3-mm fragment displacement, or open fracture.
There are multiple methods of operative fixation, including tension banding (using parallel longitudinal Kirschner wires or cannulated screws) (Figs. 35.3A,B) as well as circumferential cerclage wiring. Retinacular disruption should be repaired at the time of surgery. Comminuted fractures may require multiple small fragment or mini-fragment screws or wires.
Postoperatively, the patient should be placed in a splint for 3 to 6 days until skin healing, with early institution of knee motion. The patient should perform active assisted range-of-motion exercises; full weight bearing is allowed in extension but may be protected at the discretion of the surgeon.
Severely comminuted or marginally repaired fractures, particularly in older individuals, may necessitate immobilization for 3 to 6 weeks.
Hinged bracing is not indicated in extensor mechanism injuries.
Patellectomy
Partial patellectomy
Indications for partial patellectomy are limited but include the presence of a large, salvageable fragment in the presence of smaller, comminuted polar fragments in which it is believed impossible to restore the articular surface or to achieve stable fixation. Excision of distal fragments will lead to patella baja.
The patellar tendon may be reattached with nonabsorbable sutures placed longitudinally through drill holes along the long axis.
Total patellectomy
Total patellectomy is reserved for extensive and severely comminuted fractures and is rarely indicated.
Peak torque of the quadriceps is reduced by 50%.
Repair of medial and lateral retinacular injuries at the time of patellectomy is essential.
Following partial or total patellectomy, the knee should be immobilized in a long leg cast at 10 degrees of flexion for 3 to 6 weeks.
Complications
Postoperative infection: This is uncommon and is related to open injuries that may necessitate serial debridements. Relentless infection may require excision of nonviable fragments and repair of the extensor mechanism.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree