6 Quadriceps Snip
Patient Presentation and Symptoms
Additional exposures may be required on occasion when performing primary knee replacement in patients with advanced degenerative changes or in revision arthroplasty. Adequate exposure for revision or primary knee replacement usually requires 110 degrees of flexion. In a stiff primary knee or in revision surgery, a standard cap-sular incision alone may not be enough for adequate exposure or exchange of implants. After making a standard skin and medial capsular incision, several different extensile approaches are available in the knee that is stiff or has difficult exposure.
Indications
Following a standard medial capsular incision, if exposure is limited, the medial and lateral gutters of the knee are developed by excision of any thickened capsule scar and peripatellar tissue. The patellofemoral ligament release aids in exposure of the lateral retinaculum to create a pouch in which to evert the patella. If inversion of the patella or mobilization of the extensor mechanism is still limited, an extensile approach may be necessary.
Options to increase mobilization of the extensor mechanism can be classified into proximal or distal. Distally a tibial tubercle osteotomy can be performed that provides excellent exposure. This however, has been associated with a high incidence of complications.1,2 Proximally, options include a patellar turndown procedure such as a Coonse-Adams V-Y turn down, a modified patellar turn down, or a more simplified approach such as the quadriceps snip. The rectus or quadriceps snip increases exposure while minimizing further soft tissue dissection.
Contraindications
There are no contraindications to doing a quadriceps snip approach.
Surgical Procedure
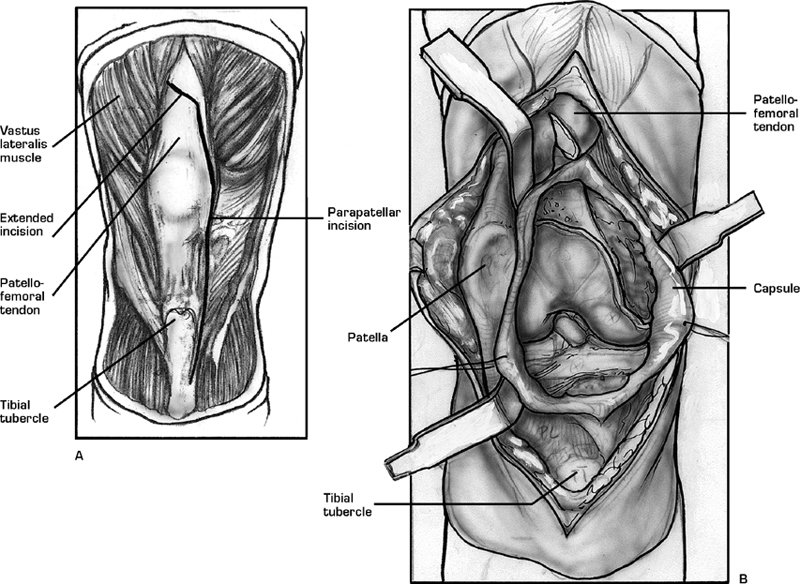
First described in 1995, the quadriceps snip was developed by Insall in 1988.3,4 After a standard skin incision and medial capsular approach, the proximal aspect of the
incision is addressed, The standard incision extends along the medial border of the quadriceps tendon. The snip is performed at approximately a 45-degree angle or directly in line with the fibers of the vastus lateralis muscle fibers (Fig. 6–1). At this level the tendon is of varying widths. No significant dissection of the muscle itself should be necessary. Inversion of the patella should now be easier to perform and the tension of the patellar tendon insertion on the tibial tubercle lessened when the knee is flexed (Fig. 6–2). As the knee is flexed, however, care should still be taken to inspect the patellar tendon insertion on the tubercle. Following implantation the oblique portion of the tendon is carefully repaired just as the vertical aspect of the tendon is repaired.
Tips and Pearls
Results comparing a standard medial parapatellar approach and the quadriceps snip show that patients have similar Knee Society scores. Motion, extensor lag, patellofemoral symptoms, and patient satisfaction are similar.1 The quadriceps snip compares favorably with other extensile procedures. There are several advantages of this straightforward extensile measure over other standard additional exposures. It is technically easier to perform and adds little to the surgical time. It minimizes further subcutaneous dissection in comparison with other options, thereby decreasing the risk of wound healing.
In comparison to a turn procedure, this approach maintains the integrity of the vastus lateralis lateral retinacular bridge, thereby minimizing risk to the integrity of the extensor mechanism. Active knee extension exercises can be initiated directly after surgery. After a patellar turndown procedure, there is typically a 2-week bracing period before active extension exercises are initiated. In addition, there is no extensor lag associated with the quadriceps snip as there is with a patellar turndown pro-cedure.1,3,5 Blood supply to the patella has not been further compromised by this extensile approach. The superior lateral genicular artery, which is cut in a turndown type of procedure, has not been violated.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








