Chapter 21 Proximal Radial Fractures
Introduction
Radial head fractures are very common. They comprise of up to 5% of all fractures and up to one-third of elbow fractures. Radial head and neck fractures have been estimated to occur in nearly 20% of all elbow trauma.1 The incidence of radial head and neck fractures in the entire population has been shown to be 2.5 per 10 000 per year and they account for 0.2% of all visits to accident and emergency departments.2
Radial head fractures occur more often than radial neck fractures in a ratio of 7 : 1. The average age of patients at the time of fracture is 45 years old. Although male : female ratio is approximately equal, in general men are older at the time of fracture (48 vs 41 years old) and sustain more severe types of injury.3
Clinical Pearl 21.1
Radial head fractures are not always simple fractures and approximately one-third of radial head fractures are complicated by associated injuries to the elbow or ipsilateral extremity. In more severe, comminuted fractures the percentage of clinically important associated lesions can increase to 80%.3
Because of the high incidence of proximal radial fractures it is important for any clinician treating these injuries to have a good knowledge of its function. The role of the proximal radius and its relationship and interaction with other structures at both the elbow and forearm has become increasingly clear in recent years. Anatomically, the proximal radius is formed by the radial neck and radial head. The radial neck is about 13 mm long4 and assures both the position of the radial head onto the capitellum and aligns the radiohumeral joint during forearm rotation. The radial neck is not straight on the radial shaft, but forms an average angle of 16.8°. This angle is variable, ranging from 6° to 28°.4 This plays a role in forearm rotation, as the rotation axis passes through the radial neck and radial head.5 The radial head articulates with the capitellum on the distal humerus, and also with the sigmoid notch (radial notch) on the proximal ulna, forming the radiohumeral and proximal radio-ulnar joints respectively. The radial head is therefore an important anatomical structure for both flexion and extension of the elbow as well as pronation and supination of the forearm. There is also some longitudinal motion between the radius and the ulna during rotation of the forearm. The radius moves about 1 mm proximally relative to the ulna when the forearm is rotated from supination to pronation.5
Besides motion, the proximal radius has biomechanical functions. The radial head plays a key role in load transfer between the forearm and the humerus. It is assumed that up to 60% of the load on the forearm is transferred to the humerus via the radiohumeral joint.6 Both the outer shape of the radial head and the articulating inner dish are elliptical in shape;7 this is an important feature for efficient transfer of forces as different areas of the dish will be in contact with different positions of the elbow and forearm. Load through the proximal radius depends on the position of the elbow and forearm and is greater with the elbow in extension and the forearm pronated.8 Varus or valgus stress also alters the load transfer between the forearm and the humerus; varus stress can decrease the portion of the load through the radiohumeral joint to less than 10%.9
Besides playing a role in mobility and load transfer, the proximal radius also acts as a stabilizing structure. The stabilizing role of the radial head has been studied extensively. The radial head has been shown to be a secondary stabilizer to valgus stress, with the medial collateral ligament as the primary stabilizing structure.10 Together with the lateral ulnar collateral ligament (LUCL) and the coronoid, the radial head has recently also been shown to be important in posterolateral rotatory (in) stability (PLRI).11
Background/aetiology
Proximal radial fractures typically occur from a fall on the outstretched hand, with the forearm in pronation. The impact is transferred through the radiocapitellar joint and the radial head and/or neck when it impacts onto the capitellum. There is also palmar translation of the radius in pronation. This is why most commonly the radial head fracture fragment is located on the anterolateral side of the radial head. Concomitant displaced capitellar fractures only occur in about 2%;3 however, smaller osteochondral lesions of the capitellum are ten times more common and capitellar bone bruising occurs in almost all patients.12 The radial head has been shown to fracture with the elbow flexed in a range between 0° and 80°.13 Finally, direct impact to the elbow may also cause the proximal radius to fracture, although this occurs much less frequently.
Associated lesions frequently complicate proximal radius fractures. The likelihood of associated lesions increases with the severity of the fracture. This increases from about 10% of patients with a non-displaced fracture, to 50% of patients with a displaced fracture and up to as much as 75% of patients with a comminuted fracture. Generally, approximately one-third of patients have one or more additional lesions adjacent to the proximal radius fracture. Nearly 25% of patients have ligamentous rupture or one or more additional fractures to the elbow. Clinically significant ligamentous lesions that require some form of treatment occur in 10% of fractures, where either the lateral collateral ligament (LCL), medial collateral ligament (MCL) or both are ruptured.3 If an MRI investigation is performed after the fracture, ligamentous injuries are found much more frequently: up to 80% of cases.12 Fortunately only a small percentage of these will need to be addressed surgically.
Associated articular elbow fractures are found in 15% of cases, with coronoid fractures being the most common (10%). In addition, between 15% and 20% of all radial head fractures are associated with a dislocation of the elbow.3,14 Many patients in this group need secondary treatment and will develop chronic problems such as stiffness or residual instability and require further treatment.
Distal radio-ulnar joint dissociation (Essex-Lopresti injury) is diagnosed acutely in only 0.3% of patients following a radial head fracture.3 This may, however, be an underestimation of the number of patients that have an Essex-Lopresti injury, as longitudinal instability can easily be missed at the initial presentation. Despite the small number of patients, it is extremely important to be vigilant for this type of injury as it can result in severe long-term disability if undiagnosed. Nine out of ten patients operated for longitudinal radio-ulnar dissociation at the Mayo Clinic between 1997 and 2002 were treated for chronic lesions as a consequence of failure of previous treatment.3
Radial head fractures are historically classified according to the Mason classification.15 Recently, it has become increasingly clear that the outcome of the treatment of radial head fractures does not depend solely on the type of fracture but also on associated lesions. As was stated above, clinically significant associated lesions occur in a large percentage of patients, and this does depend on the type of fracture. Several changes have therefore been made to the original Mason classification; the most recent adaptation was based on a demographic study of over 300 radial head fractures and their associated lesions.1,16
The proximal radial fracture itself is classified according to the original Mason classification, from types I to III. A type I fracture is non-displaced. The fragments are displaced more than 2 mm in a type II fracture, and a comminuted, non-reconstructible radial head fracture constitutes a type III. The Mayo extended classification then adds a suffix to the fracture type to show any associated lesions.1 A ‘c’ is added for coronoid fractures and an ‘o’ for olecranon fractures. Ligamentous lesions are represented by ‘m’ for medial collateral ligament (MCL) lesions, ‘l’ for the lateral collateral ligament (LCL) complex and ‘d’ for longitudinal distal radio-ulnar joint (DRUJ) dissociation (Fig. 21.1). This classification, as well as guiding treatment, was extended to provide information after treatment. The classification is adapted post surgery depending on the structures that needed surgical care. Capital letters are used if surgery was necessary. For example, ‘type IImL’ means that both the medial and lateral ligaments were ruptured in a displaced fracture, but that only the LCL was repaired. Finally, all options for treatment of the radial head fracture have been included as well; ‘X’ (excision), ‘F’ (fixed), ‘P’ (prosthesis). Results of treatment of radial head fractures can be compared more easily if associated lesions are taken into account using this classification system.
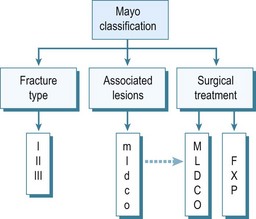
Figure 21.1 van Riet and Morrey,16 Mayo Classification1 of radial head fractures. Type I fractures are non- or minimally displaced fractures that can be treated conservatively. Type II fractures are displaced fractures that probably need surgical reduction and fixation. Type III fractures are non-reconstructible, comminuted radial head fractures. These are best treated with radial head resection or prosthetic replacement. Associated lesions are classified by adding a suffix to the description of the fracture type. m: MCL; l: LCL; d: DRUJ; c: coronoid process; o: olecranon. Upper case is used if the associated lesion needed treatment. A second suffix is added illustrating radial head treatment. X: excision; F: fixation; P: prosthesis.
Adapted with permission from: van Riet RP, Van Glabbeek F, Morrey BF. Radial head fracture. In: Morrey BF, ed. The elbow and its disorders. 4th edn. Philadelphia, PA: Saunders Elsevier; 2009:359–381.
Presentation, investigation and treatment options
Patients with a proximal radial fracture present at the accident and emergency department with a painful elbow. The history will usually reveal a fall on the outstretched hand, but other mechanisms such as direct trauma are possible. The elbow is inspected for bruising or obvious deformity, indeed dislocation of the elbow. A haematoma on the medial side may be a sign of an MCL rupture (Fig. 21.2). A visible and palpable swelling over the lateral ‘soft spot’ is indicative of a haemarthrosis. The elbow capsule can contain nearly 25 mL of fluid.17 Flexion and extension motion decreases nearly 2° per millilitre of intracapsular fluid.18
Rotation of the forearm may be nearly normal in non-displaced fractures, being limited and painful only when the fragments are displaced. Crepitus may also be heard or palpated when the elbow or forearm is moved. The patient may be guarding the elbow. Intra-articular pressure is least at about 70° of elbow flexion17 and, as pressure of the capsule is one of the most important mediators of pain in these patients, this will therefore be the least painful position for the patient.
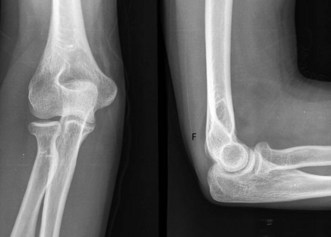
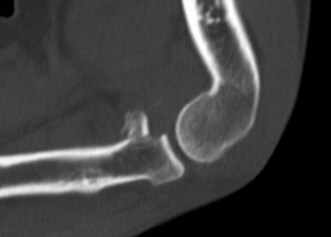
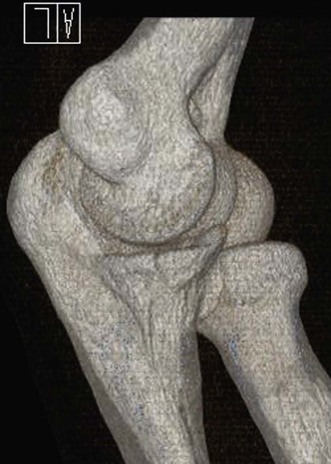
Plain anteroposterior (AP) and lateral radiographs of the elbow are taken and analysed. Specific radial head views may reveal a fracture that is not visible in other views. Care should be taken not to miss subtle associated injuries, such as a small coronoid fragment. Non-displaced radial head fractures may not be visible on plain radiographs. In this case a posterior fat pad sign (Fig. 21.3) is almost pathognomonic for a radial head fracture and treatment should be directed as such. There should be a low threshold for a CT scan of the elbow in cases of minimally displaced fractures, as this may show associated lesions (Fig. 21.4) and displacement of the fracture can be more easily assessed (Fig. 21.5). Fragments can be displaced more than one would suspect from the plain radiographs only. Both associated lesions and a correct measurement of the displacement may change the course of treatment.
Unless there is a contraindication for surgery or an acute infection of the elbow, displaced Mayo type II fractures are treated by surgical reduction and fixation of the fracture fragments. Small displaced fragments that do not block motion may be treated conservatively depending on the patient’s needs. However, it has been shown that it is probably advantageous to fix smaller radial head fragments as well.19
Reduction and fixation of radial head fractures may be undertaken arthroscopically20 or open.21 Fixation can be undertaken using different types of screws. It is important to place these screws in the non-articulating portion of the radial head or to use headless screws that can be buried beneath the articulating cartilage. Bioabsorbable pins or screws have also been shown to be effective, seemingly without any adverse effects from the material.22 The fixation of radial neck fractures is evolving as well. Plate fixation has been the treatment of choice for a long time and still is for specific types of radial neck fracture. Low-profile plates have been developed in response to the bulk of earlier, bigger plates which resulted in problems, especially rotation of the forearm. Other low-profile techniques have been described and more recently screw fixation of the radial head onto the neck has been shown to achieve reasonably stable fixation.23
Mayo type III fractures are, by definition, comminuted fractures and treatment is somewhat controversial. Reduction and fixation of type III proximal radius fractures can be technically challenging and results reported in clinical follow-up studies show that it may not be in the best interest of the patient to do everything possible to fix these fractures, if there are more than three fragments.24,25 As a consequence, it may be necessary to alter treatment during surgery from reduction and internal fixation to resection or radial head replacement.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree