Fig. 25.1
Surgical classification system of limb-sparing resections of the shoulder girdle
Restoration of shoulder function after proximal humeral resection for oncological reasons is still a challenge. In most oncological cases, resection of the rotator cuff is necessary to obtain eradication of the tumor. An optimal functional result is often difficult to obtain after a thorough radical resection. The functional outcome relates to whether a reattachment of the rotator cuff can be achieved and the functionality of the deltoid. Because the reversed shoulder prosthesis has been used with success in the rotator cuff-deficient shoulders in a population with severe arthritis of the shoulder and chronic rheumatoid arthritis [6–8], the use of the reverse polarity to treat this pathology was introduced [9].
Biomechanics
In patients whose periarticular shoulder muscles are insufficient or have been resected, with exception of the deltoid, the active shoulder function is mainly generated by the deltoid. The moment arms of this muscle are dependent on the location of the joint center [10], length of the lever arm [11], and the force generated by the deltoid muscle. The latter itself is dependent on the cross section, pennation angle [12], and fiber length [13]. Without a functional rotator cuff, the moment of the deltoid muscle should increase to obtain an active shoulder function. A ‘medialization’ and an ‘inferiorization’ of the center of rotation and a lengthening of the humeral lever arm by a ‘lateralization’ of the humeral stem [10] will enhance the deltoid moment. An increase in the wrapping angle [11], scapular rotation [14], and lengthening of the deltoid muscle [13] will also increase the deltoid moment. Those biomechanical rationales are the main reasons to introduce the reverse prosthesis for reconstructing the proximal humerus after tumor resection [12] with the ultimate goal of achieving a good functional result.
One characteristic feature of patients with a tumor in the proximal humerus is the loss of bone, sometimes leaving only a very short segment distally. The greater the resection is, the longer the lever arm effect on the relatively shorter prosthesis is in the distal humerus, causing an increased load and the risk of loosening [15].
The same problem can be seen in patients with proximal humeral fractures with substantial metaphyseal comminution. To investigate the primary stability of cemented short- and long-stem prostheses with different intramedullary fracture, Spross et al. defined a bypass index (distance from fracture level to stem tip divided by outer cortical diameter at fracture level) [16]. He described that a bypass index of 1.7 is sufficient for primary stability tested by torque to failure in their biomechanical setting. This can also be assumed applicable in reversed shoulder arthroplasty after tumor resection.
Indication
Meticulous patient selection is imperative for a successful restoration of shoulder function through an inverse shoulder prosthesis after tumor resection. A thorough work-up regarding tumoral spread should be performed, including radiography and dynamic contrast MRI.
First of all, limb salvage surgery should be a priority. The extent of tumor invasion determines whether an inverse prosthesis can be used for the reconstruction (parts 1 and 2) (Fig. 25.2). In cases of extramedullary tumor extension that compromises the deltoid muscle (part 3), axillary nerve involvement, or a bone resection extending below the deltoid muscle attachment (part 4), deltoid muscle function cannot be preserved and thus prohibits the use of an inverse shoulder prosthesis. In cases of only endomedullary extension of the tumor at the level or distal of the deltoid attachment, this reconstruction technique is still an option.
Fig. 25.2
Part 1 Proximal humerus, Part 2 attachment of latissimus dorsi, teres major, and pectoralis major, Part 3 attachment of deltoid, Part 4 distal to attachment of deltoid, Part 5 distal humerus
The major indication for reconstruction with an inverse shoulder prosthesis is, according to Malawer, a resection type IA without joint involvement. A second indication is a type VA resection with joint invasion by the tumor or a skip metastasis present in the glenoid, providing no more than 1 cm of the glenoid needs to be resected in order to avoid excessive weakness of the scapula [4] (Fig. 25.3).
Fig. 25.3
Extra-articular resection
Biopsy of the Proximal Humerus
In order to not contaminate the extracompartmental space and not to compromise the future resection, a biopsy of the proximal humerus should be carried out by an experienced oncological surgeon. The incision is oriented in a longitudinal way. The biopsy tract should traverse the anterior part of the deltoid muscle, parallel to the deltopectoral groove, avoiding the groove itself and the pectoral muscle [17]. The direction of the incision of the resection should be borne in mind as during the final surgery, the biopsy tract has to be excised. A portion of the anterior part of the deltoid is thus resected which does not impair the function of the reverse polarity [18]. A bone window is created using a high-speed drill at a predetermined level. A sufficient amount of representative material is curetted and sent for pathological examination. A hemostatic sponge is placed in the bone window, and the skin is closed after careful hemostasis (Fig. 25.4).
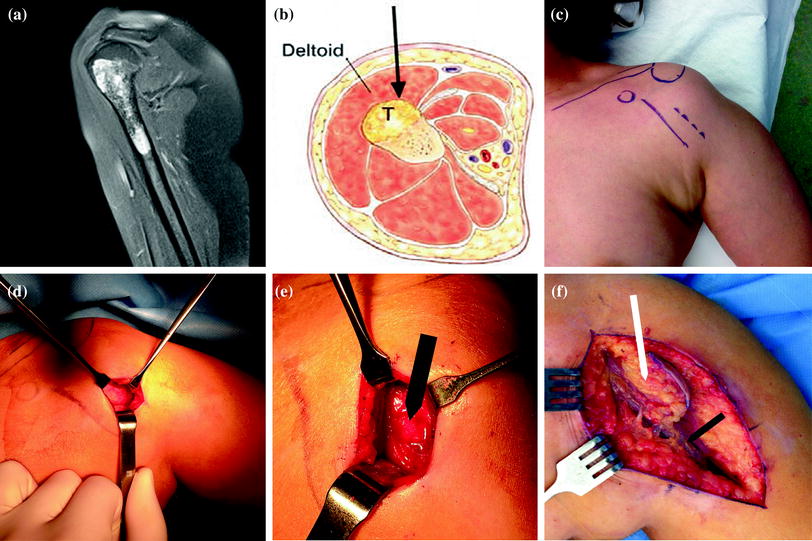
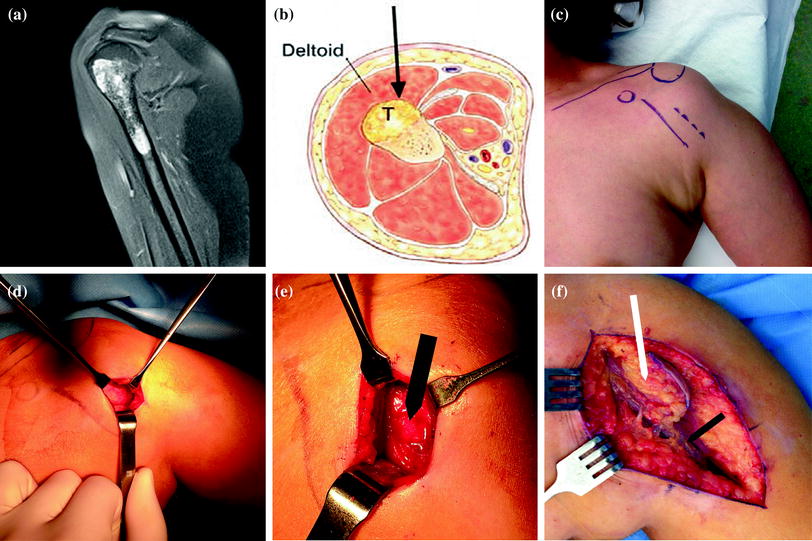
Fig. 25.4
a Preoperative MRI of the shoulder showing a cartilage tumor of the proximal humerus. b, c The biopsy trajectory should transverse the anterior part of the deltoid muscle, lateral to the deltopectoral groove. d The biopsy is oriented straight down to the bone; the bony surface can be seen at the bottom of the wound. e After taking the biopsy using a trephine burr, the hole is sealed with a hemostatic sponge (black arrow). f During final resection, the biopsy trajectory is left attached to the resection piece (white arrow), along with part of the anterior deltoid lateral to the cephalic vein (black arrow)
Operative Technique
Resection
All patients are operated under general anesthesia. The patient is positioned supine but in a very steep (‘beach chair’ position) on the operating table. The operative field and ample surrounding area of the skin are disinfected and draped. The arm is draped free and rested upon an independent mobile arm board. A large transparent plastic adhesive drape is wrapped around the shoulder. During the skin incision, the biopsy scar is excised and remains attached to the biopsy tract.
The preferred approach is the extended deltopectoral approach (with superior extension by anterior osteotomy of lateral 1/3 of clavicle and deltoid reflection as described by Redfern, Wallace, and Beddow [19]).
Further approach is between the deltoid and pectoralis major, lateral to the cephalic vein. At the medial side, the approach should avoid entering the biopsy tract. As mentioned before, a portion of the anterior deltoid is left attached to the capsule. The external border the coracoid process is identified for Malawer type VA or for type IA’s, and all ligamentous (rotator cuff interval) and bursal tissue is released. Then, the superior rotator cuff (supraspinatus) is sectioned at the level of the musculotendinous transition until the superior tubercle of the glenoid is identified for type IA tumors. For type VA, an osteotomy is done just lateral from the coracoid process parallel with the articular surface. For type IA, once the superior tubercle is identified, the long head of the biceps tendon is disinserted from it. Care is taken to resect the complete subacromial bursa together with the whole proximal humerus. A careful dissection of the deltoid is performed, leaving the axillary nerve intact. Then, the subscapularis (anteriorly) as well as the infraspinatus and teres minor (posteriorly) is sectioned at the level of the glenoid rim. For type VA tumors, the osteotomy is extended because of possibility for joint invasion or pathological intra-articular fracture, and the shoulder capsule should be left intact. For type IA tumors, the inferior glenohumeral ligament is released and partially resected from the inferior border of the glenoid. We always visualize the axillary nerve, taking care not to harm it. A disinsertion or transsection of the long head of the triceps tendon is performed to free the inferior part of the glenoid. Depending on the preoperatively determined level of resection, a section in the tendinous part of the pectoralis major, latissimus dorsi, teres major and long head triceps are performed. Care should be taken to avoid inadvertent entering of the extraosseous portion of the tumor by leaving a soft tissue envelope on the bone. The level of resection of the humerus is determined, leaving a margin of 3 cm distal to the tumor. Then, the osteotomy of the humerus is performed by an oscillating saw primarily in a horizontal way. The whole proximal humerus is sent for pathological analysis.
In case of distal endomedullary extension of the tumor, the deltoid muscle should be disinserted in one sleeve along with the brachioradialis muscle, keeping the periosteum intact. Here, a step-cut osteotomy is preferred for rotational stability of the graft (Fig. 25.5).
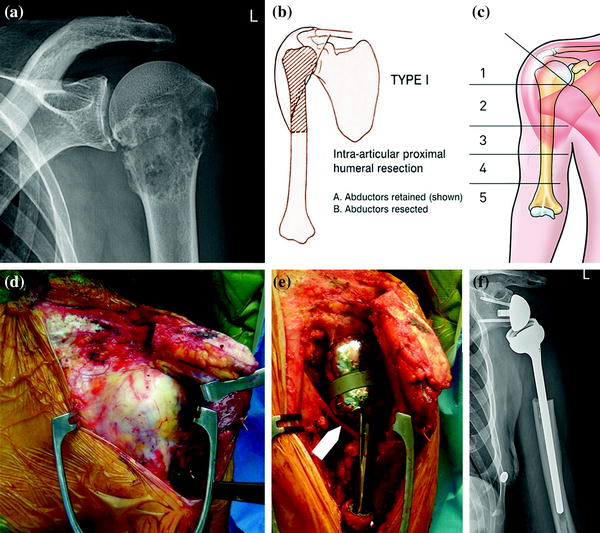
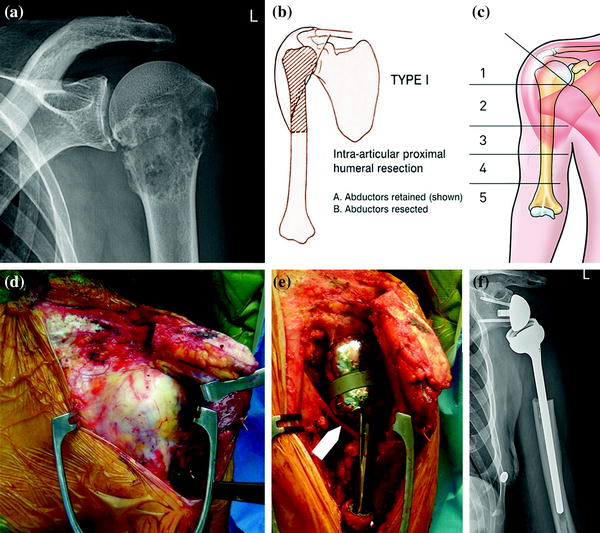
Fig. 25.5
a Radiograph showing a pathological fracture of the proximal humerus due to metastatic renal cell tumor. b A resection type B is planned: intra-articular proximal humeral resection. c The tumor extends the insertion of the pectoral muscle, zone 2. The deltoid insertion is not affected. d Approach: the clavicle is transected, leaving the anterior part of the deltoid attached to the distal part. e The prosthesis is in place, note the axillary nerve traversing deep to the prosthetic stem (arrow). f Postoperative radiograph
Reconstruction
The humeral diaphysis is prepared by reaming. We ream to the largest possible diameter in order to ensure a stable distal fixation. If an allograft of the proximal humerus is preferred by the surgeon, we advise to use the technique as described by Cuff et al. to overcome the ‘hornblower’s sign’ [20]. This surgical act is only indicated if the tendons of the latissimus dorsi and teres major are not resected by more than 1.5 cm and can be reinserted firmly to the allograft.
Then, we focus on the scapula. First, we resect all the remaining tissue underneath the acromion, thereby creating room for the delta prosthesis to move. In case of an intra-articular resection, we remove the glenoid cartilage and resect all the surrounding synovial tissue. The lateral scapular pillar is always identified by dissection. Subsequently, the glenoid is reamed with the conventional baseplate reamer at the most inferior part of the glenoid. A convex reamer is used to retain the subchondral bone as much as possible, to enhance primary bony fixation and to ensure a complete bony coverage of the baseplate. If an extra-articular allograft is necessary, a long pegged baseplate is used to lateralize the center of rotation of the reverse polarity similar to the technique of the Bio-RSA [19], in an effort to enhance the prosthetic stability by increasing the wrapping angle [3]. If no allograft is available, the surgeon can lateralize the center of rotation with an autograft from the iliac crest as described by Norris [16]. Care should be taken to position the baseplate in line with the scapular plane. Because the baseplate is implanted as distally as possible to the glenoid, a prosthetic overhang of the glenosphere to this inferior glenoid bony rim is created, which is the best way to prevent inferior scapular notching [21]. The glenoid baseplate is implanted in neutral inclination, knowing that some varus (downward) angulation is preferable compared to an upward angulation. The glenoid reconstruction is finalized with a glenosphere containing an interposition of a gentamicin-impregnated fleece (Duracol® or Septocoll) in order to minimize the risk of infection. If possible, we always implant the biggest glenosphere (42 mm) after a trial reduction.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








