Proximal Humerus Fractures: Hemiarthroplasty
William H. Paterson
Sumant G. Krishnan
INTRODUCTION
Proximal humeral fractures are common injuries representing 4% to 5% of all fractures in clinical practice, but they account for nearly half of all shoulder girdle injuries (1). After the hip and distal radius, fractures of the proximal humerus are the third most common fracture in the elderly, with a strong female predominance (2). In this age group, mechanical ground-level falls are the most common cause of fragility fractures of proximal humerus, and there is a strong correlation with the presence of osteoporosis.
Early evaluation and management of these injuries is important in optimizing treatment and functional outcomes. There are a bewildering number of treatment alternatives for managing proximal humeral fractures. Nevertheless, there is universal agreement that nondisplaced and minimally displaced fractures are best managed nonoperatively. Percutaneous fixation, plate osteosynthesis, intramedullary nailing, and arthroplasty are the most common methods of treatment for displaced and unstable fractures in adults. A recent Cochrane database review of interventions for treating proximal humeral fractures in adults showed that no single method of treatment was preferable (3). This may be due to the limited number of patients stratified to individual techniques as well as the wide variety of injury patterns and treatments.
Arthroplasty is most commonly advocated for the primary treatment of displaced three- and four-part fractures in osteoporotic bone in the elderly. However, it is technically demanding, and numerous studies have documented unpredictable outcomes (4). Notwithstanding, recent advances in surgical technique and prosthetic designs have led to more successful outcomes (5, 6, 7, 8 and 9). Improved outcomes have been documented when soft-tissue dissection is minimized and there is restoration of the “gothic arch” and anatomic reconstruction of the tuberosities (5).
INDICATIONS AND CONTRAINDICATIONS
Age, bone quality, fracture pattern, and timing of surgery are important factors that influence the surgical procedure, implant selection, and the functional and radiographic outcome. Utilizing these specific variables, we have devised an “evidence-based” treatment algorithm (Table 4.1) (10).
Age
One of the most important considerations in selecting a method of treatment in proximal humeral fractures is the chronological and physiologic age of the patient. Most female patients when they reach the sixth decade of life have some degree of osteoporosis, and many have impaired neuromuscular control as well. These factors may compromise osteosynthesis by increasing the risk of fixation failure, postoperative fracture displacement, nonunion, and/or avascular necrosis (11). Fractures in patients aged 65 years or less appear to be more amenable to humeral head preservation techniques.
TABLE 4.1 Factors Affecting Treatment Choice | ||||||||
|---|---|---|---|---|---|---|---|---|
|
Bone Quality
Similar to age, a patient’s bone quality can affect the success of humeral head preserving fixation techniques. Despite improved fixation strength in osteoporotic bone afforded by locking plate technology, complications continue to be higher in these patients after open reduction and internal fixation (12).
Fracture Pattern
Hertel et al. (13) investigating perfusion of the humeral head after an intracapsular fracture was able to prospectively correlate radiographic fracture morphology with intraoperative humeral head vascularity. Radiographic criteria predictive of humeral head ischemia included a posteromedial metaphyseal fragment extending <8 mm below the articular surface and disruption of the medial hinge defined as displacement of the humeral shaft >2 mm. When these two preoperative radiographic findings were present in conjunction with an anatomic neck fracture, there was a 97% positive predictive value for humeral head ischemia.
Even when the humeral head is vascular and amenable to preservation, the ability to maintain adequate fracture stability is necessary for successful fracture healing. The medial calcar of the humerus must be intact or restored at the time of surgery for a “stable” reduction. Comminution in this region increases the risk of a varus fracture reduction.
Timing of Surgery
The delay between injury and definitive surgery is the final variable that may affect functional outcomes following surgical management of proximal humeral fractures. For example, a fracture amenable to percutaneous fixation techniques may become impossible to reduce closed and pin percutaneously after 7 to 10 days or when early callus forms that prevents closed reduction. It is also clear that the outcomes following early arthroplasty for proximal humeral fractures are significantly improved compared to arthroplasty more than 4 weeks after injury (14). We believe that optimal surgical timing for shoulder fracture arthroplasty is 6 to 14 days after injury to allow for partial resolution of the soft-tissue swelling (assuming no acute neurovascular injury or other situation necessitating an earlier intervention) (15).
Very rarely, glenohumeral arthritis may preexist in a patient with a displaced proximal humerus fracture. If the degenerative changes are mild or moderate, conventional hemiarthroplasty is still indicated. If end-stage glenoid arthrosis is present, a total shoulder arthroplasty with insertion of a glenoid component should be strongly considered. As experience with reverse shoulder arthroplasty increases, the indications for utilizing this prosthesis in the initial treatment of proximal humerus fractures have become better defined. We typically use a reversed prosthesis when the patient is older than 75 years, when the greater or lesser tuberosity cannot be reconstructed, or the patient has ipsilateral lower extremity fractures that require crutches or a walker. In the infrequent situation in which a patient with a proximal humerus fracture has a concomitant irreparable rotator cuff tear or cuff tear arthropathy, a reversed prosthesis should be considered.
Contraindications to shoulder fracture arthroplasty are typically related to severe medical comorbidities that prevent surgical management in general. Nonoperative treatment may be a better treatment alternative for geriatric patients with complex medical comorbidities, extremely low functional demands, and minimal pain at the time of presentation. Other contraindications for arthroplasty are a history of infection, severe contracture of the shoulder girdle, open epiphysis, or fractures amenable to other fixation techniques.
PREOPERATIVE PLANNING
Clinical Evaluation
Marked edema and ecchymosis, which can extend down the arm and into the chest, are often seen in patients with proximal humeral fractures. Many elderly patients with these injuries are on anticoagulation therapy. Evaluation for concomitant injuries or associated medical conditions is important in these elderly patients. A cardiac or neurologic event may be the predisposing cause of the fall. Most of these patients require a careful medical evaluation by an appropriate specialist particularly if surgery is contemplated.
Subtle neurologic injury occurs in a large number of patients with proximal humeral fractures (15). Utilizing electromyography, Visser et al. (15) documented neuropraxia of the axillary and/or suprascapular nerves in 50% of patients. Clinical appreciation and documentation of this finding is important for both prognostic evaluation and preoperative counseling, as eventual recovery may take up to 12 to 18 months after surgery (6). These may be very difficult to identify clinically in a patient with a painful swollen shoulder following fracture.
Radiographic Evaluation
Radiographs should include anteroposterior, scapular “Y,” and/or axillary views. As part of our protocol, we obtain full-length scaled radiographs of both humeri using a ruler of defined length for preoperative planning (Fig. 4.1). If plain radiographs do not allow a clear understanding of the fracture morphology, a computed tomography scan with three-dimensional reconstructions may be a helpful.
Neer’s classic four-part description of proximal humerus fractures has endured by virtue of its simplicity. Despite this, interobserver reliability and intraobserver reproducibility have been reported to be only poor to fair (16). A “comprehensive binary” description of these fractures based upon Codman’s original concept of fracture planes has also been described (Fig. 4.2) (13). In this classification, there are 12 possible fracture patterns: 6 patterns resulting in 2 fracture fragments, 5 patterns resulting in 3 fracture fragments, and 1 pattern resulting in 4 fracture fragments. In the original study by Hertel et al., ischemia was observed only in types 2, 7, 8, 9, 10, and 12. This system has demonstrated improved interobserver reliability as well as better intraobserver reproducibility.
Restoring the “Gothic Arch”
Anatomic restoration of humeral height, correct prosthetic version, and tuberosity reconstruction play critical roles in determining functional outcome (5). Many studies have shown that poor functional results correlate closely with prosthesis and/or tuberosity malposition. Boileau et al. (4) described the “unhappy triad,” in which the prosthesis is cemented “proud” and retroverted and the greater tuberosity has been positioned too low. This
combination is associated with persistent pain and stiffness and poor function. Careful attention to the restoration of the proximal humeral anatomy is crucial in obtaining good results following shoulder fracture arthroplasty.
combination is associated with persistent pain and stiffness and poor function. Careful attention to the restoration of the proximal humeral anatomy is crucial in obtaining good results following shoulder fracture arthroplasty.
 FIGURE 4.1 A scaled ruler is placed on the patient’s arm during the radiograph to calculate magnification. |
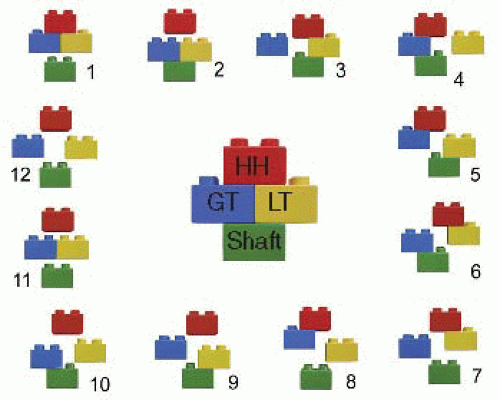 FIGURE 4.2 Hertel’s binary (LEGO) proximal humerus fracture description system. HH, humeral head; GT, greater tuberosity; LT, lesser tuberosity. (Modified from Hertel R, Hempfing A, Stiehler M, et al. Predictors of humeral head ischemia after intracapsular fracture of the proximal humerus. J Shoulder Elbow Surg 2004;13(4):427-433.) |
We use the term “gothic arch” to describe the architectural anatomy of the proximal shoulder girdle as seen on an anteroposterior radiograph (5). The arch is formed by tracing a line along the medial border of the proximal humeral calcar to the articular surface and joining this with a line along the lateral border of the scapula to the articular surface. The result is a classical “vaulted” or “gothic” arch shape seen in medieval period architecture (Fig. 4.3). This simple concept allows for a highly reproducible surgical technique for restoration of proper humeral height, which improves the potential for anatomic tuberosity reconstruction.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








