Proximal Humeral Fractures: Open Reduction Internal Fixation
John T. Gorczyca
INTRODUCTION
Fractures of the proximal humerus are common injuries and comprise approximately 4% of fractures seen in clinical practice. They are the third most common extremity fracture in the elderly after the hip and distal radius. The majority of these fractures are the result of lower-energy injuries in older patients, which occur following a ground-level fall. Fortunately, most fractures are minimally displaced and are best treated nonoperatively. However, with higher-energy mechanisms such as motor vehicle collisions, athletic injuries, or falls from a height, the fracture is commonly multifragmentary, displaced or unstable, and surgery is often indicated. Displaced proximal humeral fractures can present complex technical challenges, especially in elderly patients with compromised bone. Over the past decade, there has been a dramatic increase in the number of patients with proximal humerus fractures treated surgically. This is due to an aging population who are living longer and have an increased expectation of improved shoulder outcome as well as significant improvement in the implants used to treat these fractures. Traditionally, hemiarthroplasty was the most common procedure in the geriatric patient with a displaced three- or four-part proximal humeral fracture. However, this procedure is associated with unpredictable outcomes even in the hands of experienced shoulder surgeons. With the recent development and widespread availability of periarticular locking plates for the proximal humerus, there has been a renewed interest in internal fixation as an alternative treatment. While the early reports with locked plating were promising, the technique is not a panacea and numerous problems have been described.
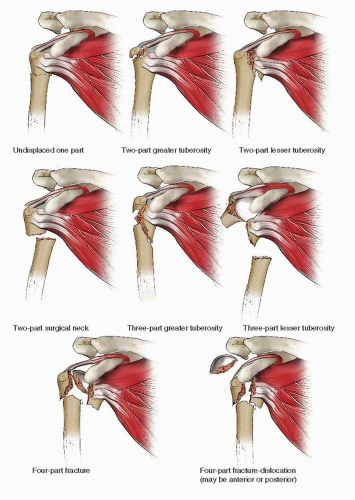
The most common classification of proximal humeral fractures was described by Neer (Fig. 3.1). Although inter- and intraobserver reliability of this classification system is imperfect, its popularity stems from its relative simplicity and its utility in guiding treatment.
INDICATIONS AND CONTRAINDICATIONS FOR SURGERY
Regardless of the method of treatment, the great majority of proximal humerus fractures will heal. Nonoperative treatment is indicated for all nondisplaced and most minimally displaced fractures in virtually all age groups. Following injury, fracture healing takes 6 to 10 weeks, but functional recovery of shoulder motion and strength takes much longer, and even fully compliant and motivated patients may fail to regain preinjury levels of function and activity. Surgery is indicated for most patients with significantly displaced three- and four-part fractures and dislocations of the proximal humerus. The nonoperative management of widely displaced fractures often leads to symptomatic malunion, with painful loss of shoulder motion frequently due to impingement, muscle weakness, and rotator cuff pathology. The goal of surgery is to restore the head shaft relationship and tuberosities with stable fixation to allow early range of shoulder motion. This permits many patients to lift their arm above their shoulder for activities of daily living. In many patients, the inability to perform this task may compromise a geriatric patient’s ability to live independently. However, many elderly and frail patients with multiple medical comorbidities should be treated nonoperatively accepting some loss of function. Likewise, preexisting neuropathy or stroke that compromises the expectation for functional benefit after surgery are strong indications for nonoperative treatment.
Less common indications for surgery include bilateral fractures, ipsilateral upper extremity injury (“floating elbow” or “floating shoulder”), open fractures, fracture dislocations, polytrauma, and fractures with associated vascular injury. Displaced fractures in adult patients should be reduced and stabilized. More than 40 years ago, Neer recommended surgery for fractures of the proximal humerus with displacement of the head or either of the tuberosities by 1 cm, or angulation >45 degrees, which we still follow today. Isolated fractures of the greater tuberosity should be reduced and stabilized when displacement is >5 mm in any direction.
Not all proximal humeral fractures that require surgery are amenable to internal fixation. Strong indications for hemiarthroplasty include head-splitting fractures (with the exception of some young patients with healthy bone) anatomic neck fractures, and displaced three- and four-part fractures in patients with either comminution or osteoporosis that would not support internal fixation. Preexisting chronic rotator cuff deficiency with arthropathy is better treated nonoperatively or with shoulder arthroplasty.
PREOPERATIVE PLANNING
History and Physical Examination
Seriously injured patients should undergo initial evaluation according to Advanced Trauma Life Support (ATLS) protocols to ensure a thorough evaluation and to prevent missed injuries.
In the multiply injured patient with a shoulder fracture, injuries to the head, neck, chest wall, and upper extremity commonly occur. Proximal humeral fractures that occur in elderly patients following lower energy falls may be associated with injuries to the head, face, or wrist. When possible, a careful history may reveal substantial medical comorbidities such as hypertension, coronary artery disease, or diabetes. The patient’s medication record should be scrutinized with particular reference to anticoagulation medication. Other important factors include hand dominance, occupation, and living status, which may play an important role in decision making.
All patients should have a complete physical examination. The extremity should be examined for swelling, ecchymosis, peripheral pulses, and neurologic impairment. Any questions regarding the vascular integrity warrant further evaluation, with an ankle-brachial index, Doppler evaluation, or angiography. If any abnormality is identified, vascular surgical consultation should be obtained. A thorough neurologic examination of the entire upper extremity must be performed and documented. Evaluation of the axillary nerve can be difficult in a swollen painful shoulder, but should be tested by asking the patient to contract the deltoid muscle whenever possible. Range of motion of the shoulder is typically limited due to pain. It is also important to evaluate the elbow, forearm, wrist, and hand performed in order to avoid missing a more distal injury.
Radiographic Evaluation
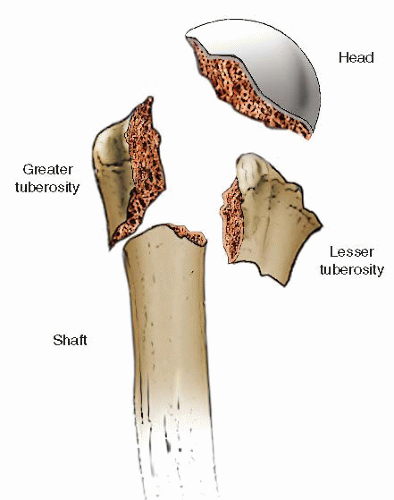
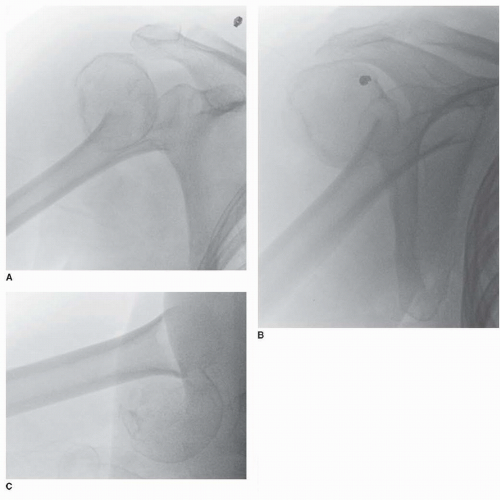
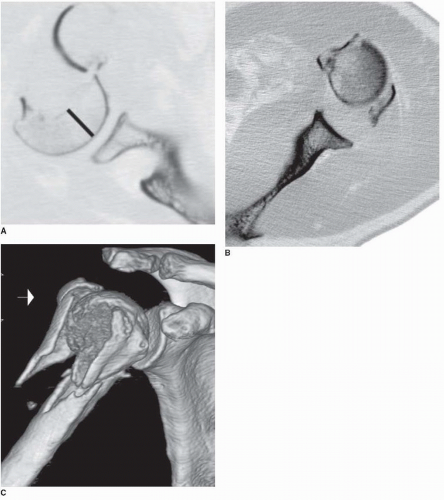
The proximal humerus consists of four parts: The humeral head, the greater and lesser tuberosities, and the humeral shaft (Fig. 3.2). In order to optimally visualize these four parts, all patients with a shoulder injury should have an anteroposterior view, a transscapular lateral (“Y”) view, and an axillary lateral view (Fig. 3.3A-C). The axillary lateral, while challenging to obtain in the trauma setting, often provides crucial information. It is frequently the best view to rule out a coronal plane head-splitting fracture, a glenoid rim fracture, as well as a glenohumeral joint subluxation or dislocation. It is important to remember that if the x-ray beam is not orthogonal to the axis of the humeral shaft (which is often the case), then any measurement of fracture angulation will be exaggerated. Thus, the transscapular lateral radiograph provides a better view for accurately measuring fracture angulation. In patients with complex fracture patterns, a computed tomographic (CT) scan can be helpful to evaluate fragment size and displacement and can reveal nondisplaced fracture lines (Fig. 3.4A,B). The thickness of the humeral head seen on the CT scan should be carefully assessed when considering internal fixation. If the head is too small or thin, stable fixation may not be achieved and cut out of the screws is more likely. In addition to the axial, sagittal, and coronal
reconstructions, 3D imaging provides detailed topographic views which may allow a clearer appreciation of the fracture geometry (Fig. 3.4C). In some cases, the scapula can be “subtracted” giving even more information about the fracture morphology. Based on the physical exam, x-rays of the cervical spine, clavicle, ribs, elbow, or forearm may be indicated.
reconstructions, 3D imaging provides detailed topographic views which may allow a clearer appreciation of the fracture geometry (Fig. 3.4C). In some cases, the scapula can be “subtracted” giving even more information about the fracture morphology. Based on the physical exam, x-rays of the cervical spine, clavicle, ribs, elbow, or forearm may be indicated.
Timing of Surgery
The majority of displaced proximal humerus fractures can be managed in a semielective fashion without compromising the quality of the outcome. A patient with an isolated closed, proximal humeral fracture seen in the emergency room can be discharged to home or to a suitable location if the pain is controlled and their social circumstances permit. These patients are seen in the office or clinic several days later and scheduled for surgery if indicated. On the other hand, if the pain is poorly controlled, the social circumstances are not optimal, or the patient has other injuries, patients are typically admitted to the hospital for earlier surgery.
Fortunately, there are relatively few indications for emergent surgery. However, an open fracture, a fracture with a vascular injury, an irreducible fracture with impending skin compromise, or an irreducible fracture dislocation require immediate intervention. In these cases, surgery should be performed as soon as an operating room becomes available and a surgical team can be assembled.
Surgical Tactic
The most important step in preoperative planning is for the surgeon to carefully evaluate the x-rays and CT scan and answer two questions. First, does this fracture require surgery, and second, what is the optimal implant if surgery is required. Despite good preoperative planning, there is a small group of patients where the final decision between internal fixation and arthroplasty cannot be made until the time of surgery. If any doubt exists, the patient should be consented for both types of surgery, and the equipment and implants must be in the operating room at the beginning of the case.
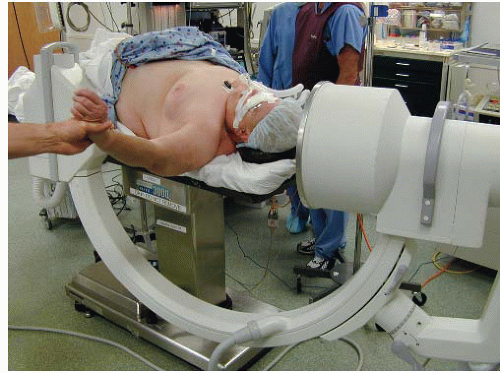
Surgery can be performed with the patient in either the beach chair position or supine on a flat-top radiolucent table. There are advantages and disadvantages with each technique. In the supine position, the patient should be
positioned at the edge of the table with the arm supported on a hand board or a Mayo stand to allow shoulder abduction. Properly positioned, this setup will not interfere with the use of the C-arm. The patient’s head is supported on a gel “donut” or a rolled-up stockinet, and the patient’s eyes should be protected during the case (Fig. 3.5).
positioned at the edge of the table with the arm supported on a hand board or a Mayo stand to allow shoulder abduction. Properly positioned, this setup will not interfere with the use of the C-arm. The patient’s head is supported on a gel “donut” or a rolled-up stockinet, and the patient’s eyes should be protected during the case (Fig. 3.5).
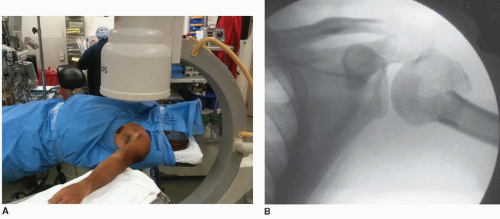
Prior to prepping and draping, the C-arm should be moved into position to ensure high quality anteroposterior and axillary lateral images can be obtained (Fig. 3.6A-D). In most operating rooms, this is easiest if the surgical table is rotated 90 degrees. I prefer the C-arm to come in from the cranial side, slightly oblique to allow visualization of the entire humeral head and the edge of the glenoid when an axillary lateral view is obtained. It is wise to rehearse these moves so that the radiology technician can change from an AP to an axillary lateral views easily without the need to move the arm or shoulder. The spot for the C-arm is marked with tape on the floor in order to re-create the intraoperative position of the fluoroscopy unit during surgery (Fig. 3.7).
Surgery
Surgery is most commonly performed under general anesthesia, which allows optimum control of the patient’s blood pressure and muscle paralysis. Regional nerve blocks are most useful for postoperative pain control. A helpful technique is to position and tape the endotracheal tube on the side opposite the fracture. Maintaining the mean arterial pressure close to 70 mm Hg helps minimize bleeding, and muscle paralysis or relaxation is helpful to lessen the forces required for muscle retraction and fracture reduction. A cepholsoporin antibiotic is given for
prophylaxis within 1 hour of surgery. A Foley catheter, arterial line, central venous pressure (CVP) monitoring, or Swan-Ganz catheters are used when the patient’s medical comorbidities or physiologic status dictates.
prophylaxis within 1 hour of surgery. A Foley catheter, arterial line, central venous pressure (CVP) monitoring, or Swan-Ganz catheters are used when the patient’s medical comorbidities or physiologic status dictates.
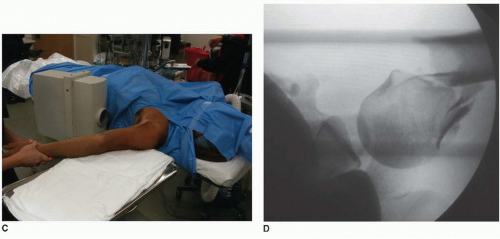 FIGURE 3.6 (Continued) C. The C-arm is rotated to obtain an axillary lateral view with abduction and mild traction. D. An axillary lateral must show the entire head and the glenoid. |
The entire upper extremity, shoulder, chest wall, and neck are prepped and draped in the usual orthopedic fashion. A surgical time-out is called, and all members of the surgical, nursing, and anesthesia teams must agree on the patient’s name, medical record number, and correct side and site of surgery.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree