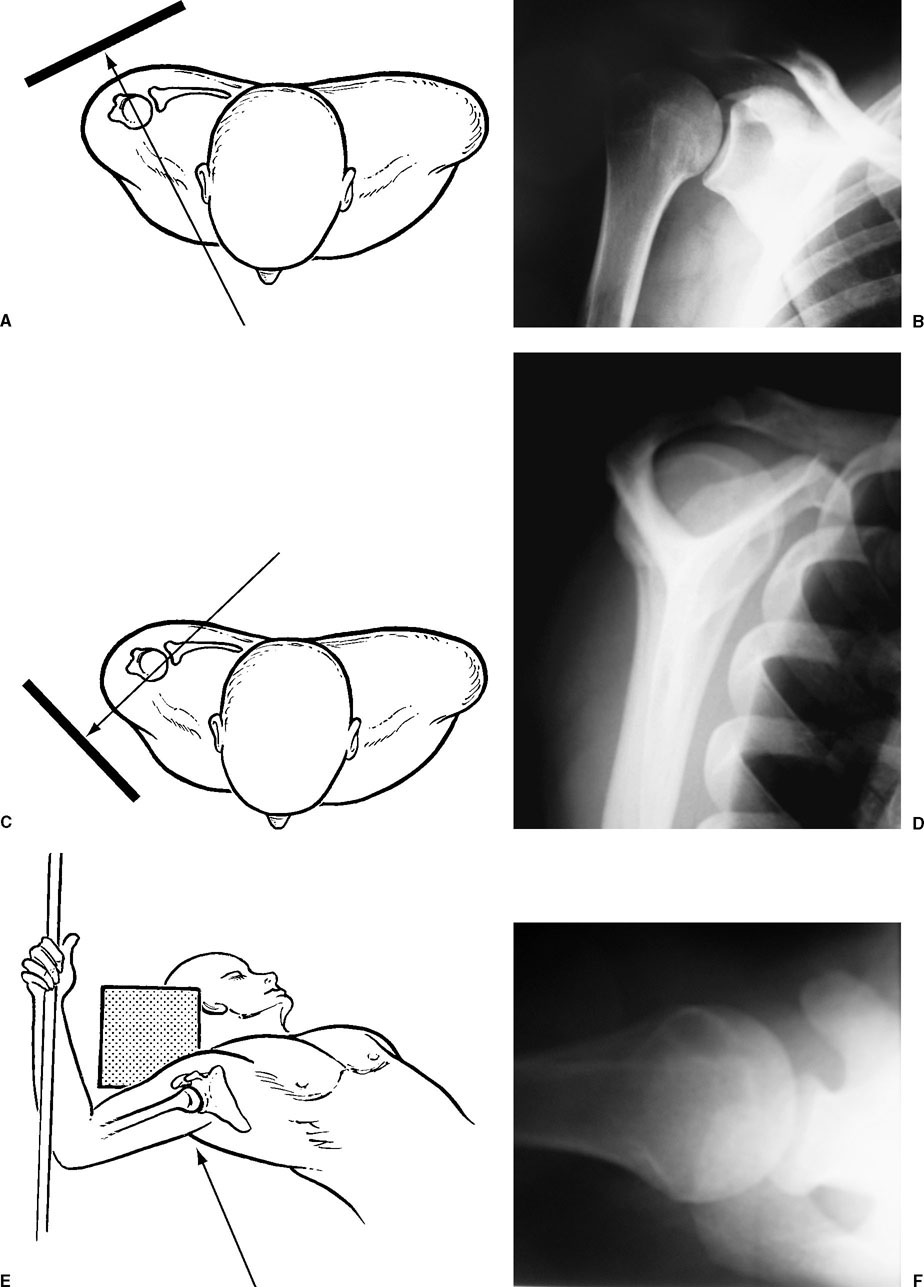
Fractures of the proximal humerus are potentially complex injuries that can be challenging to diagnose and treat. A comprehensive evaluation of the entire shoulder girdle is an essential component of the management of these injuries. Imaging of the proximal humerus can be difficult. An accurate radiographic evaluation must be obtained, however. Classification systems have evolved over time, and their ability to reliably predict outcome and guide treatment have greatly improved. This chapter focuses on the clinical and radiographic evaluation of the patient who sustains a proximal humerus fracture, and describes the classification systems that are currently in use. Proximal humerus fractures are relatively common, representing 4 to 5% of all fractures.1 They are considered to be an osteoporosis-related fracture based on an increased incidence in elderly women and this location in metaphyseal bone.2,3 Approximately 75% of proximal humerus fractures occur in elderly postmenopausal women, and they are most commonly associated with simple falls.1 Lind et al4 demonstrated this female predominance (3:1), as well as a low-energy injury pattern in an epidemiologic study of 730 proximal humerus fractures.4 Like other osteoporosis-related fractures, a unipolar age distribution exists, with the highest incidence occurring in octogenarian woman.3 Fractures of the proximal humerus tend to occur most commonly in the subset of the elderly population that is relatively healthy and physically fit. Court-Brown et al3 evaluated 1027 proximal humerus fractures in Edinburgh over a 5-year period, and found that less than 10% of these fractures occurred in institutionalized patients and more than two thirds of the patients were living independently at the time of fracture. A large epidemiologic study from Sweden demonstrated a steady and significant increase in the incidence of proximal humerus fractures over the last 30 years.5 Other investigators have reported similar results and have partially attributed these findings to the increased average life span.4 All epidemiologic data confirm that fractures of the proximal humerus are primarily an osteoporosis injury. As our population ages, these fractures will represent an increasingly significant socioeconomic problem and source of morbidity in the elderly population.1,6,7 When evaluating a patient with a proximal humerus fracture, it is essential to obtain a detailed history and perform a comprehensive examination. The history should include the mechanism of injury, to determine if a high- or low-energy event occurred. It is critical to determine whether a fall was secondary to a syncopal episode and if the patient sustained a head injury. If either occurred, full medical and neurologic evaluation is necessary. The patient’s handedness, occupation, and health status should be determined. It is also important to inquire about previous injuries to the shoulder or preexisting loss of function. The patient’s overall psychological well-being should be assessed during the initial interview, as well as the patient’s expectations of treatment. The patient’s own assessment of the impact of the injury may very well impact the ultimate outcome.8,9 The physical examination of the injured extremity requires visualization of the entire shoulder region and upper extremity. Proximal humerus fractures usually result in varied degrees of swelling, which may make it difficult to palpate specific bony landmarks. Significant ecchymosis can develop 24 to 48 hours after the injury, frequently with extension to the chest wall flank and distally into the arm, elbow, and forearm (Fig. 3-1). It is important to instruct patients to remove any jewelry from the ipsilateral extremity, as tendon swelling of the wrist and hand can also develop within 24 to 48 hours. Palpation of the proximal humerus area is anticipated to be painful, and attempts to initiate active motion will also be painful and possibly associated with crepitance.10 Careful inspection of the contours of the shoulder is important. Although swelling may obscure these landmarks, a significant deformity should raise a suspicion for fracture dislocation. Anterior prominence, posterior flattening, and the prominence of the posterolateral acromion should suggest an anterior dislocation component. Conversely, posterior prominence, prominent coracoid process, and anterior flattening should suggest a posterior dislocation.10,11 FIGURE 3-1 Ecchymosis of the arm down to the elbow is evident in this 58-year-old man less than 48 hours after sustaining a one-part fracture. The chest wall should be carefully examined because rib fractures may occur in association with the fall. More significant associated thoracic injury, although rare, can occur with proximal humerus fractures and especially with fracture dislocations. Pneumothorax and intra-thoracic penetration of the humeral head have been reported. These more significant injuries usually occur in association with fracture dislocations.12,13 The stability of the fracture should be assessed during the physical exam. Gentle rotation of the humeral shaft is performed while palpating its proximal portion (Fig. 3-2). If the humerus moves as a unit, some degree of fracture stability is present. If the humerus does not move as a unit or if crepitance is present, the fracture is unstable. It is important to note that fracture stability and adequate alignment are different issues. A stable fracture pattern may be significantly malaligned but impacted, providing some stability.7 FIGURE 3-2 The stability of the fracture can be most easily assessed by gently rotating the humeral shaft while palpating its proximal portion to determine if the humerus “moves as a unit.” A detailed neurovascular examination must be done and documented at the time of the initial examination. The close proximity to the brachial plexus and axillary artery makes them susceptible to injury. Distal pulses must be documented; however, the presence of a distal pulse does not preclude an arterial injury.14–16 A thorough sensory exam is essential. The axillary nerve is most commonly injured, followed by the suprascapular nerve. Nerve injuries have a reported prevalence of 5 to 30%.17 These injuries are typically neuropraxias and occur with displaced fractures. It is difficult to assess deltoid activity due to pain inhibition; however, the sensory component of the axillary nerve can easily be assessed by examination of the lateral aspect of the deltoid.10 If a complete and reliable neurologic exam cannot be obtained at the time of the initial assessment, it should be repeated as symptoms subside. Deltoid atony may occur after a proximal humerus fracture or in a postoperative setting. This condition results in inferior subluxation of the humeral head, which is visualized on the anteroposterior (AP) radiograph (Fig. 3-3). This condition must be differentiated from an axillary nerve injury. The inferior subluxation associated with deltoid atony usually resolves within 3 to 4 weeks of injury as deltoid function improves.18 FIGURE 3-3 Inferior subluxation (“pseudosubluxation”) may be evident following proximal humerus fractures as a result of pain inhibition of the deltoid (“deltoid atony”). FIGURE 3-4 Following closed reduction of a displaced surgical neck fracture, diminished distal pulses were noted in this 68-year-old patient. Angiogram showed the axillary artery to be caught in the fracture site, requiring vascular repair and fracture stabilization. The axillary artery injuries are much less common than neurologic injuries. Excellent collateral circulation exists around the shoulder, which may mask a thrombosis or laceration. Injury to the vasculature can occur as a result of direct impingement by fracture fragments or by entrapment of the vessel in the fracture site (Fig. 3-4). Distal pulses may still be present in the setting of a vascular injury. An expanding hematoma may be the only clinical sign suggesting a vascular injury. An associated brachial plexus deficit should raise the suspicion of a possible vascular injury.15,16 Proximal humerus fractures most commonly result from a fall onto an outstretched hand from a standing position.4,6 The fracture results from an indirect force that is transmitted to the proximal humerus as the patient attempts to cushion the fall with the outstretched arm. Two alternative injury mechanisms include: (1) a direct lateral blow to the shoulder, or (2) an axial load transmitted through the elbow.11 Codman described an additional mechanism of injury that involved excessive rotation of the arm in an abducted position that leads to impingement of the humerus on the acromion.10 Electrical shock or seizure activity can lead to violent and powerful muscle contractions around the shoulder girdle, resulting in fracture, dislocation, or fracture-dislocation.19–22 Proximal humerus fractures in young adults typically represent injuries in polytrauma. When a very low energy injury results in a proximal humerus fracture, a pathologic etiology should be considered. A critical aspect of evaluating proximal humerus fractures is determining the position of the fracture fragments and the degree of displacement. The radiographic imaging of the glenohumeral joint can be difficult due to the fact that it lies between the sagittal and coronal planes of the body.23 Therefore, anteroposterior and lateral views oriented to the body do not provide true images of the glenohumeral joint. Overlapping osseous and soft tissue shadows in combination with multiple fracture lines further increases the difficulty of interpreting radiographs. Nonetheless, accurate radiographic evaluations are essential to determine the appropriate treatment plan. The trauma series is considered the gold standard for the radiographic evaluation of proximal humerus fractures. Fracture classification and treatment decisions are typically based on these views, which include AP and lateral views of the plane of the scapula and an axillary lateral view24,25 (Fig. 3-5). By orienting the projection of the x-ray to the scapula instead of to the body, a view of in the plane of the glenohumeral joint can be obtained. These three radiographs allow for evaluation of the fracture in three distinct orthogonal planes.26 The scapula AP view provides a general overview of the fracture and is typically evaluated first (Fig. 3-6). It can be obtained easily with the injured extremity maintained in a sling for comfort. Because the scapula lies posterior and somewhat lateral on the thorax (angulated 45° from the frontal plane), the true plane of the glenohumeral joint lies in this 45° plane, not in the plane of the thorax. The x-ray must be angled 45° from medial to lateral to demonstrate the glenohumeral joint in profile. This view avoids the overlap of the humeral head and the glenoid; that is, there should be clear separation of the glenoid from the humeral head.24,26 When an x-ray is taken in the plane of the thorax, an oblique view of the glenohumeral joint will be obtained. In this situation, overlap of the humeral head and glenoid can obscure the details of the fracture. The axillary view is obtained with the patient supine and the arm abducted 30° to 90°. The beam is directed into the axilla angulated toward the coracoid in an inferior to superior direction. The x-ray cassette is placed on the superior aspect of the shoulder. The patient’s head is tilted to the opposite side so that the plate could be placed medially.27 This view is excellent for visualizing dislocations and fractures involving the articular surface (Fig. 3-7). Positioning of the patient for the axillary view is more difficult because of the need for shoulder abduction. Proper positioning usually requires the physician to gently abduct the arm, and at times hold the arm in position while the x-ray is obtained. The scapula lateral, like the scapula AP view, can be obtained with the arm in a sling. It does not require manipulation of the arm and is less painful for the patient. The x-ray beam is directed parallel to the spine of the scapula. A true lateral projection of the scapula forms the letter Y in which the upper arms of the Y are formed by the coracoid process anteriorly and the scapula spine posteriorly. The vertical portion of the Y is formed by the scapula body. All three limbs of the Y intersect in the position of the glenoid and the humeral head (Fig. 3-8). It should be visualized overlapping this point.14,22 This view assists in delineating the position of the humeral head relative to the glenoid and demonstrates anteriorly and posteriorly displaced fragments.28,29 A study by Sidor et al25 evaluated the relative contributions of the axillary and scapula lateral views to the fracture classification using the Neer system. Each x-ray of the trauma series in 50 proximal humerus fractures was evaluated by four orthopaedic surgeons and one musculoskeletal radiologist using different sequences: scapula AP, axillary view and scapula lateral versus scapula AP, scapula lateral, and axillary view. They found that the combination of the axillary and AP view was just as effective in determining fracture classification as the entire trauma series. The axillary view had a much greater impact on fracture classification than the scapula lateral view. Inadequate x-rays are probably the most common problem encountered when evaluating proximal humerus fractures. The three views of the trauma series should be obtained first using proper technique so they will provide as much information as possible. Other views have been described that may provide additional information to augment the trauma series. The Velpeau axillary view is a modification of the axillary view that was designed for the acutely injured patient because it allows the x-ray to be taken with the arm adducted in the sling (Fig. 3-9). The patient sits or stands near the x-ray table and leans back 20° to 30°. The x-ray cassette is placed in the table slot directly beneath the patient’s shoulder. The beam passes vertically from superior to inferior through the shoulder.30 This radiograph results in a magnified view of the glenohumeral joint and is helpful for identifying anterior/posterior dislocations. Our experience has been that it does not provide the details of fracture anatomy, and a properly positioned supine standard axillary and lateral view is preferred. Other modifications of the axillary view have been described such as the stripp axial.31
Proximal Humeral Fractures: Clinical Evaluation and Classification
 Epidemiology
Epidemiology
 Clinical Evaluation
Clinical Evaluation
History and Physical Examination




Mechanism of Injury
Radiographic Evaluation
Trauma Series
Additional Radiograph Views
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






