Proximal Humeral Allograft Prosthetic Composites
Joaquin Sanchez-Sotelo
Reconstruction of the shoulder joint in the presence of massive bone loss may be performed with the combination of an allograft and a prosthesis (allograft prosthetic composite or APC) (1,2). Shoulder stability and function largely depend on the surrounding musculotendinous structures and the implant design used. Healing of the deltoid and rotator cuff tendons to the allograft is desirable. Reverse prosthesis designs may prove to play an important role when rotator cuff function cannot be reliably restored by other means. Alternatives to reconstruction with an APC include a tumor prosthesis, osteoarticular allografts, arthrodesis with or without vascularized autograft, Tikhoff-Linberg interscapulothoracic resection, and amputation.
INDICATIONS
Reconstruction of the proximal humerus with an APC is indicated in situations of massive loss of the proximal humerus secondary to
Resection of tumors
Implant failure
Bone resection for deep infection
Severe posttraumatic bone loss
Age and activity play some role in the choice of the reconstructive technique. Osteoarticular allografts are favored by some authors for the younger patients (3,4), whereas tumor prostheses, where the metal body of the prosthesis replaces the length of missing bone, usually are reserved for older patients with lower functional demands and life expectancy (5,6). For most patients, though, an APC represents the best alternative, as it provides restoration of bone stock and the potential for soft tissue healing to the allograft (2) but avoids problems secondary to allogeneic cartilage disintegration (4).
CONTRAINDICATIONS
The use of an APC may be contraindicated for the following reasons:
Active deep infection
Poor soft tissue envelope
Inadequate remaining bone stock for secure fixation of the construct
Oncologic contraindications for limb salvage surgery
PREOPERATIVE PLANNING
Preoperative planning is paramount to achieve a successful reconstruction when performing a shoulder APC. The preoperative evaluation and planning are different depending on the indication for reconstruction.
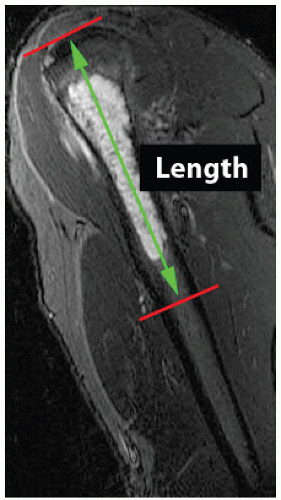
Reconstruction After Tumor Resection
In patients with tumors requiring proximal humerus resection, radiographs should be complemented with magnetic resonance imaging (MRI) to determine a safe resection level to achieve negative margins if possible. An arteriogram may be useful when arterial involvement is suspected. The length of the allograft should match the length of the resected segment as measured on the MRI (Fig. 30.1) and intraoperatively. Radiographs with magnification markers also assist in the preoperative planning for the appropriate allograft size. The length of the allograft used will also depend on the implant used: when the reconstruction is performed with an anatomic hemiarthroplasty, the length of the graft should replicate the length of bone resected; nonanatomic reverse designs change the joint center of rotation to a more inferior position and may require a shorter allograft to avoid excessive overlengthening.
Failed Previous Reconstruction
When a proximal humerus APC is considered in patients for previous failed reconstructions, (failed osteoarticular allografts, failed shoulder replacements, resection after deep infection, large posttraumatic bone loss), the soft
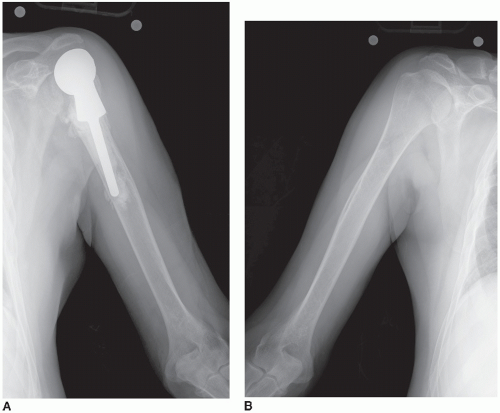
tissues around the shoulder will often present contractures or deficiencies, and the length of the allograft is largely determined intraoperatively based on ease of reduction, passive shoulder motion, soft tissue tension and balance, as well as the ability to perform a satisfactory soft tissue repair. Radiographs of the opposite intact humerus may be used for planning (Fig. 30.2), but intraoperative adjustments are needed to adapt to changes in the soft tissues.
tissues around the shoulder will often present contractures or deficiencies, and the length of the allograft is largely determined intraoperatively based on ease of reduction, passive shoulder motion, soft tissue tension and balance, as well as the ability to perform a satisfactory soft tissue repair. Radiographs of the opposite intact humerus may be used for planning (Fig. 30.2), but intraoperative adjustments are needed to adapt to changes in the soft tissues.
TECHNIQUE
Principles
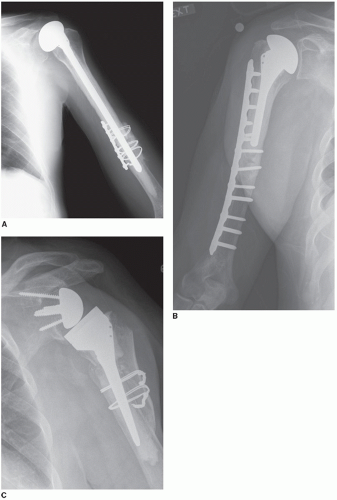
Proximal humeral reconstruction with an APC may be performed with different techniques depending on the size of the defect, cuff integrity, and surgeon preferences (Table 30.1; Fig. 30.3).
Implant Type and Fixation Anatomic (nonreverse) implants are most commonly used for patients with a well-preserved rotator cuff, either after tumor resection or as revision of a previous reconstruction. Humeral head replacement (shoulder hemiarthroplasty) is selected for patients with no glenoid cartilage loss; otherwise, total shoulder arthroplasty should be considered. When an anatomic implant is used, a proximal humeral allograft with rotator cuff tendons attached to it should be used, so that the host rotator cuff can be repaired to the allograft tendons with multiple nonabsorbable sutures.
The design and length of the stem may change depending on the size of the defect and surgeon preferences. The humeral component needs to be fixed to the allograft with bone cement. If the length of the allograft needed is shorter than the length of the stem, the component is cemented into both the allograft and the native humerus (Fig. 30.3A). When the allograft length exceeds the length of a conventional primary stem, the author’s preference is to just cement the standard stem into the allograft (Fig. 30.3B), but many surgeons prefer to bypass the graft-host junction with a long revision cemented stem providing additional intramedullary fixation.
When the integrity of the rotator cuff is severely compromised as a result of previous pathology or the need to remove it as part of a tumor resection, a reverse shoulder arthroplasty may be considered. Safe implantation of the uncemented glenoid component of a reverse prosthesis requires reasonable bone stock, which may be compromised in the revision setting. Reverse total shoulder arthroplasty may provide more stability and active elevation than an anatomic hemiarthroplasty in patients with severe cuff deficiency needing an APC. However, internal and external rotation may end up being more limited and the mid- and long-term complications and outcome are largely unknown.
Nonanatomic prostheses designed specifically to act as spacers are required when part or most of the glenoid needs to be removed as part of the tumor resection, not allowing a stable reconstruction with a hemiarthroplasty or the implantation of the glenoid component of a reverse prosthesis. These spacers
provide suture holes for fixation of the proximal aspect of the implant to the scapula with transosseous nonabsorbable sutures.
provide suture holes for fixation of the proximal aspect of the implant to the scapula with transosseous nonabsorbable sutures.
TABLE 30.1 Options for Proximal Humeral Reconstruction Using an APC | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
Allograft-host Junction




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree