Prosthetic Options for Persons with High-Level and Bilateral Lower-Limb Amputation
John W. Michael and Milagros Jorge
Learning Objectives
On completion of this chapter, the reader will be able to do the following:
1. Discuss the incidence and prevalence of high-level and bilateral lower-limb amputations.
2. Describe the etiology of high-level and bilateral lower-limb amputations.
4. Estimate the relative energy cost of ambulation with high-level or bilateral limb loss.
High-level transfemoral amputation and bilateral amputation of the lower extremity are the result of trauma or disease pathology such as peripheral vascular disease because of health conditions such as diabetes. The twenty-first century has started out to be a time of war in many nations around the globe. The United States and other North Atlantic Treaty Organization (NATO) countries have engaged in war and military conflicts. Traumatic amputation associated with war due to the use of landmines, improvised explosive devices (IEDs), and combat fire has resulted in an increase incidence and prevalence of high-level and bilateral lower-limb amputation.1 Peripheral vascular disease either primary or diabetes related is the leading cause of bilateral amputation in the United States.2 Such a significant limb loss presents a substantial challenge to the patient, the prosthetist, and other rehabilitation professionals. Successful prosthesis fitting is often time consuming and difficult; however, for many individuals with high-level or bilateral lower-extremity amputation, prostheses can enhance the ability to increase functional independence and mobility. This chapter summarizes key concepts for high-level transfemoral and bilateral lower-extremity prostheses prescription, fabrication, and rehabilitation based on clinical factors, research evidence, and expected outcomes.
High-level lower-limb loss
The first part of this chapter focuses on options for patients with a unilateral high-level lower-limb absence, which is an amputation at or above the hip joint. Hip disarticulation and transpelvic and translumbar losses have been estimated to comprise fewer than 2% of all amputations in the United States.3 As a result, only those clinicians associated with specialty centers, such as major trauma hospitals, have the opportunity to see significant numbers of such cases. Most prosthetists, therapists, and physicians see only a handful of patients with such high-level loss in a practice lifetime. One result of treating each high-level patient as one-of-a-kind is that many differing approaches can be found in the literature.
Etiology
Hip disarticulation is a relatively rare amputation. The incidence is reported at 0.5% to 3.0%.3,4 There are three distinct causes of hip disarticulation: vascular disease, trauma, and malignancy. Vascular impairment, whether or not associated with diabetes mellitus, is the most common cause for lower-limb loss in the industrialized world. Dysvascular symptoms are generally most pronounced in the distal limb, leading to nonhealing ulceration, infection, gangrene, and ablation. The trunk and a portion of the upper thigh are usually spared even in the presence of severe peripheral vascular disease. Although rarely, vascular disease at times, leads to high-level amputation.5 The assumptions about healing, cardiovascular limitations, and tolerance of activity derived from the experience with patients with dysvascular amputation do not apply to those with high-level amputation. Most patients with high-level amputation are relatively healthy and have reasonable cardiopulmonary reserves, excellent cognition, and a strong desire to attempt prosthetic fitting.
The more common cause for hip disarticulation or high-level lower-limb amputation today is a traumatic injury resulting in life-saving emergency medical services and surgical intervention. In civilian life, within the industrialized countries, motor vehicle accidents are the most common cause of lower-extremity amputation. The use of landmines in developing nations throughout the twentieth century contributed to high-level limb loss. Although the international community has banned the practice of placing landmines, many landmines still exist and continue to inflict trauma that results in high-level amputation. Military conflicts in Iraq and Afghanistan and the aggressive rebel tactic of use of IEDs has resulted in wounded warriors that survive the trauma and are transported to military hospitals for medical care and rehabilitation. Military hospitals are aggressively addressing the rehabilitation needs of soldiers with amputation. The Intrepid Center for Fallen Heroes Fund constructed the Center for the Intrepid at Brooke Army Medical Center in San Antonio, Texas. The Center for the Intrepid is a state-of-the-art rehabilitation facility for wounded warriors. Today, soliders with limb loss may be able to continue their military careers. The Center for the Intrepid rehabilitation programs work to maximize the functional abilities of men and women whether they plan to return to active duty or assume civilian life. Because of the prolonged U.S. involvement in the Iraq and Afghanistan wars, there are greater numbers of individuals with hip disarticulations.6
Many high-level amputations are performed for tumor of the femur, such as osteosarcoma. Fortunately, the frequency of tumor-related high-level amputation is decreasing with advances in limb-salvage procedures and more effective chemotherapy and radiation therapy.7–9 Patients who require amputation because of tumor can be divided into two groups: those with benign or fully contained tumors who require no further oncological intervention and those undergoing chemotherapy and radiation after amputation. Persons with benign or fully contained tumors are typically in excellent physical condition after the amputation, eager to return to their former lifestyle as much as possible, and ready for early prosthetic fitting. The benefits of early prosthetic fitting are well established and are both physical and psychological.10 Early mobilization and single-limb gait training on the contralateral limb with an appropriate assistive device is recommended to reduce the risk of deconditioning, which occurs even after a few days of hospitalization.11,12 The rehabilitation and prosthetic management of patients requiring chemotherapy or radiation therapy may have to be adapted or delayed depending on the patient’s physical condition, energy level, tolerance of activity, and healing of the surgical site.
Most patients with high-level amputation should be offered the opportunity for prosthetic fitting and rehabilitation. A multidisciplinary team rehabilitation team experienced in the management of persons with amputation is essential to assure the most desirable outcomes.12
Biomechanics
Although, historically, loss of the entire lower limb assumed the use of locked joints in the prosthesis, ample clinical evidence is available that locked prosthetic joints are seldom necessary. Since the 1950s, free-motion hip, knee, and ankle joints for hip disarticulation and transpelvic prostheses have become the norm. The Canadian design hip disarticulation prosthesis was introduced by Colin McLaurin,13 and the biomechanics of this prosthesis were clarified by Radcliffe in 1957.14 These same biomechanical principles are also used in the functional design of prostheses for patients with higher level amputation.
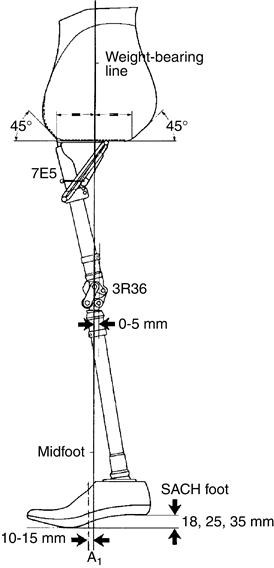
In essence, the high-level prosthesis is stabilized by the ground reaction force (GRF), which occurs during walking.15 For example, when standing quietly in the prosthesis, the person’s weight-bearing line falls posterior to the hip joint, anterior to the knee joint, and anterior to the ankle joint. The resultant hip and knee extension moments are resisted by mechanical hyperextension stops of the prosthetic hip and knee joints, and the dorsiflexion moment is resisted by the stiffness of the prosthetic foot (Figure 25-1). This same principle permits the patient with paraplegia using bilateral Scott-Craig knee-ankle-foot orthoses to stand without external support.16
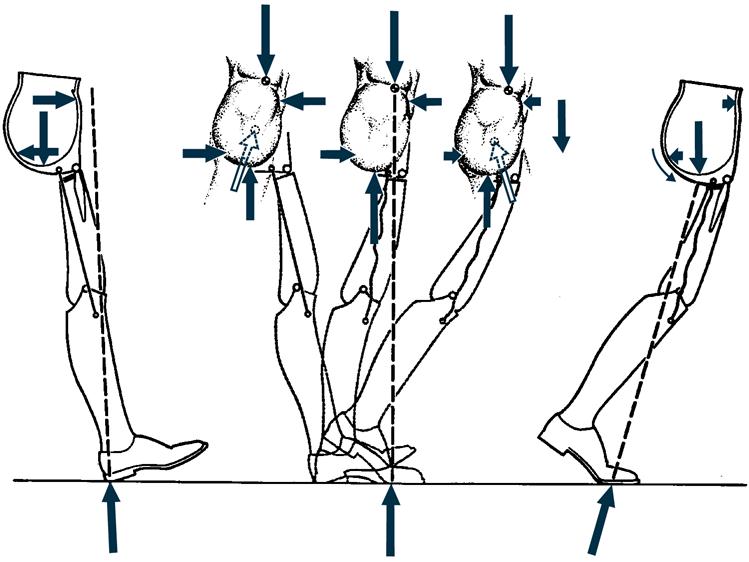
Ambulation with a high-level prosthesis also relies on the GRF (Figure 25-2). When an experienced prosthetic wearer walks with an optimally aligned hip disarticulation or transpelvic prosthesis, the dynamic gait is surprisingly smooth and consistent. Patients with hip disarticulation or transpelvic amputations who have sufficient balance and strength can learn to walk without any external aids, although the use of a cane is also common.
The basic functions of the GRF during ambulation with one type of high-level prosthesis can be summarized as follows. At initial contact, as the prosthetic heel touches the ground, the GRF passes posterior to the ankle axis, the heel cushion compresses, and the foot is lowered to the ground. At the same time, an extension moment is created at the prosthetic knee as the GRF passes anterior to the knee joint axis (see Figure 25-2, A). By midstance, alignment stability is maximal as the GRF passes posterior to the prosthetic hip joint axis and anterior to the prosthetic knee joint axis, just as it does during quiet standing (see Figure 25-2, B). As forward progression continues into preswing, the GRF moves posterior to the knee joint axis, allowing the knee to bend passively to facilitate swing phase foot clearance while weight is being shifted onto the opposite limb (see Figure 25-2, C).
Two major biomechanical deficits are inherent with hip disarticulation and transpelvic prostheses: First, the prosthetic limb is always fully extended at midswing because of the loss of active hip flexion. As a result, the length of the prosthesis is typically shortened slightly, compared with the remaining limb, to assist in toe clearance during the swing phase of gait. The consequence of this strategy, however, is a second biomechanical deficit—limb length discrepancy.17
Component Selection
The earliest hip disarticulation prosthesis designers insisted on locking all prosthetic joints. Later, proponents of free-axis joints for hip disarticulation prostheses advocated the use of only basic components, such as a single-axis knee and ankle. In recent years, a strong consensus has emerged that, to meet the patient’s functional needs and goals fully, components for patients with hip disarticulation and transpelvic amputations should be selected for the same reasons and with the same criteria as for those with transfemoral and transtibial amputation.18,19
Choosing a Prosthetic Foot
All prosthetic feet have been successfully used for high-level amputations. Nonarticulating designs are often chosen because of their dependability, durability, and low maintenance; these designs rarely require servicing as a result of wear and tear. Single-axis feet (which allow the patient to quickly attain a stable foot-flat position) are used when enhanced knee stability is a concern. Multiaxial and dynamic response designs are usually reserved for higher-activity individuals who appreciate the added mobility of such components.20
Choosing a Prosthetic Knee Unit
The prosthetist selects a particular knee unit on the basis of the patient’s functional needs. Because of the biomechanical stability of these prostheses, locked knee designs are rarely necessary. Locked knee designs have two additional drawbacks: they must be unlocked before sitting, and they may increase the risk of injury in the event of a fall. When stability is a primary concern, stance control or polycentric knees may be most appropriate. Single-axis knees, when properly aligned, also work well. The prosthetist might choose a pneumatic or hydraulic knee unit to provide fluid swing phase control for patients who are active and want the ability to change cadence.19 Most recently, quite encouraging clinical results have been reported with a microprocessor-controlled, hydraulic stance and swing control knee, allowing active individuals to descend stairs foot-over-foot with a hip disarticulation prosthesis for the first time.21
Choosing a Prosthetic Hip Joint
The majority of patients with hip disarticulation benefit from a free-motion hip joint, although locking joints are still sometimes chosen for those with quite limited ambulation capabilities. Much effort has been made to provide some measure of active hip flexion motion in these prostheses because that would reduce or eliminate the key biomechanical deficits previously noted. In prior decades, modification of the hip joint by adding a coil spring mechanism that induced hip flexion when the prosthesis was unweighted was tried with some success, but maintenance and breakage of the spring precluded widespread acceptance. More recently, a flexible carbon fiber thigh “strut” that functions as a leaf spring has been used clinically in selected cases. Initial reports suggest that this approach increases cadence and that the improved swing clearance achieved by better prosthetic hip and knee flexion eliminates the need to shorten the prosthesis.22 The use of vertical shock-absorbing shin elements and knees with stance flexion features is also being explored, with encouraging clinical acceptance.
Torque Absorbers
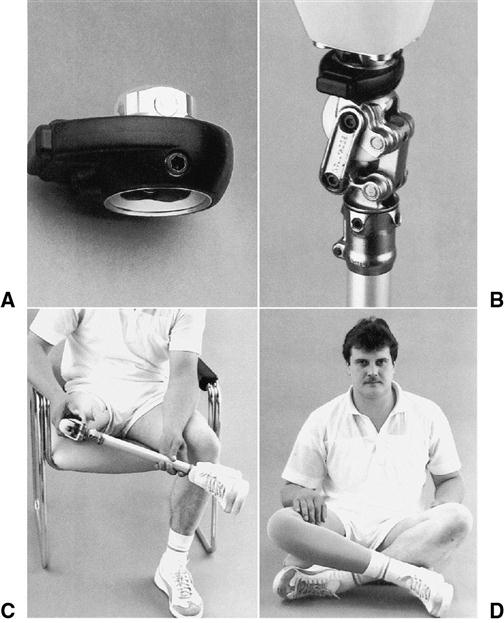
With the loss of three major biological joints of the lower limb, a corresponding loss of the body’s ability to compensate for rotary motions inherent in gait occurs. For this reason, many prosthetists strongly recommend that a torque-absorbing device be included in these high-level prostheses. Torque absorbers typically improve both stride length and comfort by absorbing transverse forces that would otherwise be transmitted to the socket as skin shear.23,24 Incorporation of a lockable turntable above the prosthetic knee is also suggested to facilitate common daily activities such as dressing and entering an automobile (Figure 25-3).
Energy Consumption
The major unresolved drawback to prosthetic fitting for those with high-level amputation is the tremendous increase in effort required to control a prosthetic limb with passive joints. Walking with a hip disarticulation or transpelvic prosthesis is much like controlling a flail biological leg. The concentration and energy required to ambulate makes short distance ambulation much more practical than distance walking for all but the most vigorous adult wearers.
Gait studies suggest that the use of a hip disarticulation prosthesis requires approximately 200% more effort than unimpaired walking.25 This is approximately the same effort required when using axillary crutches in single-limb gait. Because single-limb amputation with crutches tends to be faster than walking with a hip disarticulation prosthesis, the relatively high rejection rate of such prostheses is not surprising. Schnall and colleagues found that kinematic changes and energy expenditure increased 100% or more during ambulation in persons with hip disarticulation.6
Most rehabilitation professionals believe that any patient with an amputation who is physically and mentally capable of prosthetic use should, if interested, be fitted with an initial prosthesis. This recommendation is particularly true for those with high-level amputation who may feel “cheated” and become depressed if their clinical teams do not allow them to try prosthetic ambulation.
Socket Design
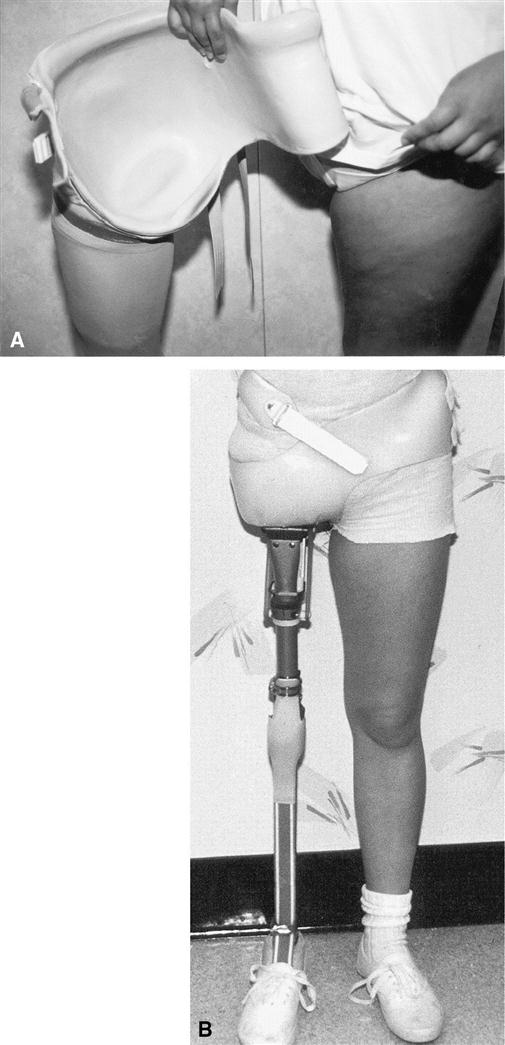
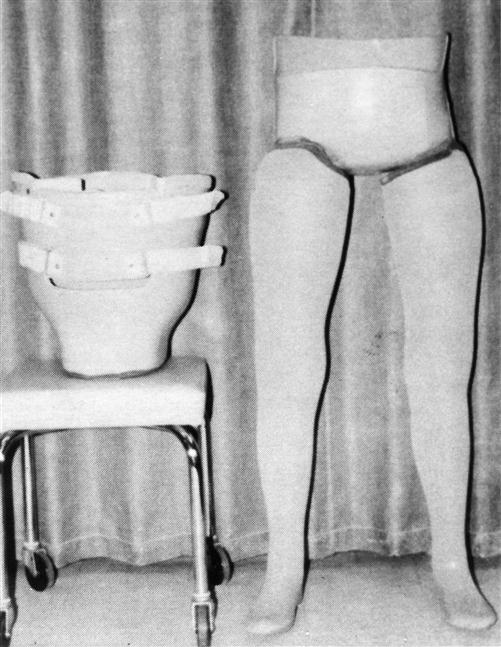
A variety of socket designs have been described in the clinical literature. The most critical factors for successful use are careful fitting and secure suspension, regardless of which socket design is selected. For patients with hip disarticulation, encapsulation of the ascending pubic ramus may add stability, although not every patient is able to tolerate a proximal trim line in the perineum.15,26 Flexible thermoplastic or silicone materials within a rigid laminated frame are more comfortable and increasingly popular than the more common hard plastic sockets (Figure 25-4).27–29
Suspension is achieved by carefully contouring the socket just proximal to the iliac crests whenever possible. When the patient is obese or has no ileum, shoulder straps may be necessary to minimize swing phase pistoning of the prosthesis.
The transpelvic socket must fully enclose the gluteal fold and perineal tissues and completely contain the soft tissues on the amputated side. Full enclosure provides comfortable weight bearing on the residual limb tissues despite the absence of hemipelvis. Early transpelvic sockets extended upward to contain the lower ribs.30 Clinical experience has shown that this may not always be necessary for relatively muscular or lean individuals. Failure to contain the transpelvic residuum adequately results in obvious protrusion where the trim lines are insufficient. Prosthetists modify the positive plaster model of the transpelvic residuum to incorporate a diagonally directed compressive force in the socket design to support and contain transpelvic tissues and eliminate the risk of perineal shear and tissue breakdown.31
For patients with translumbar amputation, weight bearing is achieved with a combination of soft tissue compression and thoracic rib support. Because of the loss of more than half of the body mass in this amputation, weight-bearing tolerance is better than might be expected. Designs that allow the patient to vary the compression by adjustable straps are often useful.32
Patients with translumbar amputation require a socket for effective seating and wheeled mobility (Figure 25-5). Many patients with translumbar amputation successfully progress to ambulation for short distances with a prosthesis and choose to wear prosthetic limbs to enhance their cosmetic appearance and self-image. Long-term followup demonstrates positive prosthetic outcomes; return to work or school is usually a realistic goal.33 For most patients, polycentric knees provide sufficient stability for the household ambulation typical of this population, making locking joints unnecessary.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree