2.2 Proprioception It is likely that the connective tissue continuum of fasciae and fascial structures serves as a body-wide mechanosensitive signaling system with an integrating function analogous to that of the nervous system (Langevin 2006). Without doubt fasciae and fascial structures play a substantial role in the process of proprioception (Langevin 2006; Stecco et al., 2007b; Benjamin 2009). Fascial components like membranes and septa or deep and superficial fascia are an intricate and integrated part of the locomotor apparatus (Wood Jones 1944; Standring 2005). To play that functional, role in proprioception, the fascial structure should be equipped with adequate neuroanatomical substrate (‘proprioceptors’). For the quality of the centripetal information, however, how the mechanical architecture of the connective tissue structure at stake relates to the skeletal and muscular tissue in a given area is an important feature (Benjamin 2009; Van der Wal 2009). Only if a given fascial structure has a mechanical architectural relationship with muscular or skeletal elements, is it able to provide the mechanoreceptive information needed for proprioception. This means that the aptitude of a fascial structure to provide centripetal mechanoreceptive information depends on its architecture and structural relationship with muscular and skeletal tissue and not simply on its topography (Van der Wal 2009). In this chapter proprioception is defined in the neurophysiologic way – as the ability to sense the position and location, orientation, and movement of the body and its parts. In a more strict sense, proprioception could be defined as the process of conscious and subconscious sensing of joint position and/or motion (Skoglund 1973; Fix 2002). Here, the more explicit meaning of the psychological definition of ‘proprioception’ as sometimes applied, as the notion ‘body image sense’ or ‘body awareness’ is not meant. Proprioception, in this context, has to be discriminated from exteroception, relating us with the outer world, as well as from interoception, informing about visceral and metabolic processes (see elsewhere in this book). The morphological substrate of proprioception – encapsulated or unencapsulated mechanosensitive sensory nerve endings (mechanoreceptors) and related afferent neurons (see Fig. 2.2.1) – is considered to provide the centripetal information needed for the control of locomotion or for the maintenance of posture (Barker 1974). On the level of the brain this information is integrated with information originating from other sources (e.g., more specific proprioceptive sense organs like the labyrinth or skin receptors) to the overall conscious and subconscious awareness of position and motion (kinesthesis and statesthesis). Fig. 2.2.1 • Types of mechanoreceptors. In this context, mechanoreception is not synonymous with proprioception. Proprioception relates to mechanoreception as seeing relates to the retina. The mechanoreceptive information needed for the process of proprioception originates not only from fasciae and other connective tissue structures but also from mechanoreceptive or even tactile information from skin, muscles, joint surfaces, and joint structures. Mechanoreceptors are triggered by mechanical deformation like squeezing, stretching or compression. In order to understand their contribution to the proprioceptive information it is not only important to know their topography (where and in which elements of the locomotor apparatus they are located) but also how they are spatially and mechanically related with the various (tissue) components of the system. Proprioception in the fascia is not only provided by the mechanoreceptors that are located within or are immediately attached to the fascial structures, but also the architecture of the fascia plays an instrumental role in the process of proprioception. It can do so by mediating forces that cause deformation of receptors (which in fact represents the main stimulus for mechanoreceptors) that are not directly attached to the fascia itself. The term “ectoskeleton” has been proposed by some authors (Benjamin 2009) to capture the idea that fascia could serve as a significant site of muscle attachment, constituting a kind of “soft tissue skeleton”. Mechanoreceptors situated within muscles as anatomical units may orient as to their distribution and spatial organization to the fascial layers to which the muscle fascicles insert and between which muscular tissue is interposed in the process of force transmission. In such cases, the fascial architecture plays an instrumental role in the process of proprioception without the necessity for the connective tissue structures themselves being directly equipped with mechanoreceptive substrate (Van der Wal 2009). So, to evaluate the significance of fascial structures as to the proprioceptive input from a certain body region it is not only important to know the anatomy of the given fascia (‘where’) but also its architecture, i.e., functional relationship (‘how’). Many fascial structures play a direct or indirect role in force transmission. Most anatomy textbooks, however, describe the locomotor apparatus as a system built up from discrete elements involved in positioning, motion, and force transmission: i.e., muscles (with tendons and aponeuroses) and ligaments. In this outdated concept, muscles represent the main elements in the system, which in atlases are often presented as discrete anatomic structures with the surrounding and ‘enveloping’ connective tissue layers removed. When connective tissue is met as a layer, a membrane, a fascia covering a body structure or organ or region, is usually given a name derived from the anatomic substrate that the layer covers. Fasciae therefore are most often defined as a suborganization of the ‘primary’ anatomy of organs (e.g., muscles) This is all related to the ‘dissectional mind’ that still prevails in the anatomy atlases and textbooks and considers the locomotor apparatus as built up from anatomical elements. When Schleip (2003a, b) mentions the fascia as “the dense irregular connective tissue that surrounds and connects every muscle, even the tiniest myofibril, and every single organ of the body forming continuity throughout the body” or as the “organ of form” (Varela & Frenk 1987), he actually presents fascia as an important integrative element in human posture and organization of movement (locomotor apparatus). Therefore an analytical and ‘dissectional’ approach of the ‘anatomy’ of the fascia cannot do justice to the role of fascial tissue and structures in proprioception. The primary connective tissue of the body is the embryonic mesoderm. The mesoderm represents the matrix and environment within which the organs and structures of the body have been differentiated and in fact are ‘embedded’. Blechschmidt (2004) distinguished the mesoderm, as germinal layer, as an ‘inner tissue’ in opposition to the ectoderm and endoderm as ‘limiting tissues and proposed not to call it a ‘derm’ but to call it ‘inner tissue’. The primary “inner tissue” is the undifferentiated connective tissue mesenchyme, which in principle is organized in three components: cells, intercellular space (interstitial substances), and fibers. In the functional development and differentiation of the primary connective tissue, there are two patterns of ‘connection’. The first pattern is the development of ‘intercellular space’, which represents a fissure functioning as a sliding and slipping space. This is seen in the formation of coelom (body cavities), joint cavities, and also in bursa-like gliding spaces between adjacent tendons or muscle bellies. In this pattern spatial separation is ensured, and in this way motion is enabled. The second pattern is the formation of a binding medium. That can be fibers (e.g., as in regular dense connective tissue structures like the desmal sutures in the skull, interosseous membranes, and ligaments) or interstitial substrate and matrix (for example, in cartilaginous joints). In osteopathic circles, the continuum and continuity of the ‘connective tissue apparatus’ in the human is emphasized. Such a view is in harmony with the view that the principal function of mesoderm as “inner tissue” is ‘mediating’ in the sense of ‘connecting’ (binding) and ‘disconnecting’ (shaping space and enabling movement). • Fasciae of muscles adjacent to spaces that are filled with loose, areolar, connective tissue (‘sliding tissue’) and sometimes with adipose tissue. They enable the sliding and gliding of muscles (and tendons) against each other or against other structures. In such splits globular or oval mechanoreceptors triggered by compression (see below) could inform the brain about the displacement and movement of fascial tissue and related structures. • Intermuscular and epimysial fasciae that serve as areas of insertion for muscle fibers that in this way can mechanically reach a skeletal element without necessarily being attached directly to the bone. They appear as intermuscular septa but also as so-called superficial fasciae (like fascia cruris and fascia antebrachii,) providing a broad insertion area for muscle fibers. If provided with more stretch susceptible receptors, such fascial layers could inform about stresses of the fascial tissue in relation to the transmission of forces. On the other hand, a pattern can be described where connective tissue and muscular tissue are organized mainly in series with each other in a more ‘transmuscular’ organization. Huijing et al. (2003) point out that, often, muscles which from an anatomical perspective are considered as morphologically discrete elements cannot be considered as isolated units controlling forces and movements. Detailed studies of the lateral cubital region of man and rat showed such architecture quite clearly (Van der Wal 2009). Nearly all the deep and superficial regular dense connective tissue (RDCT) layers are organized in series with muscle fascicles (presented as muscle compartment walls). Collagenous fibers that run from bone to bone – thought to be stressed passively by displacement of the articulating bones – hardly occur. Instead, there occur broad aponeurotic layers of RDCT to which relatively short muscle fascicles insert, which, on the opposite side, are directly attached to skeletal elements. Such configurations of muscle fascicles attached to the periosteum of one articulating bone, and via a layer of RDCT indirectly attached to another articulating bone, could be considered ‘dynamic ligaments’. Such ‘dynaments’ are not necessarily situated directly beside the joint cavity or in the deep part of the joint region (Van der Wal 2009).
Proprioception, mechanoreception and the anatomy of fascia
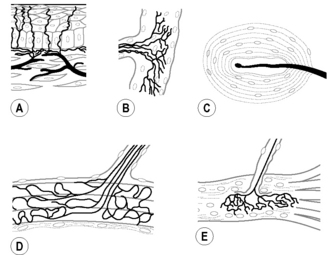
(A) Free nerve ending (FNE); (B) Ruffini corpuscle (RC) or spraylike endings; (C) lamellated corpuscle (LC) or Paciniform ending; (D) Golgi tendon organ (GTO); (E) muscle spindle (MS).
Connectivity and continuity
Architecture is different and more than anatomy
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








