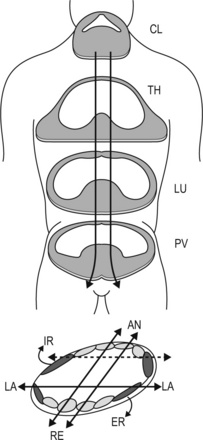
7.7 Fascial manipulation Fascial Manipulation© is a manual therapy for the treatment of musculoskeletal pain developed by Luigi Stecco, an Italian physiotherapist. This method, which has evolved over the last 30 years through anatomical studies and clinical practice, is based on a three-dimensional biomechanical model for the human fascial system (Stecco 1988, 1990, 1996, 2004; Stecco & Stecco 2009). The key premise of this model is that fascia is not just a uniform membrane, but it presents a specific organization and relationship with the underlying muscles. In particular, the fascia is seen as a: • coordinating element for motor units (grouped together in myofascial units) • uniting element between unidirectional myofascial units (myofascial sequences) • connecting element between body joints via myofascial expansions and retinacula (myofascial spirals). • muscular fiber insertions directly onto deep fascia (Stecco et al. 2007a) • fiber distribution according to precise motor directions (Stecco et al. 2008a, 2009a) • myotendinous expansions that link adjacent segments (Stecco et al. 2009b). Extensive histological analysis of deep muscular fascia has also provided evidence for hypotheses concerning fascia’s role in proprioception and tensional force distribution within the fascial system (Stilwell 1957; Yahia et al. 1992; Stecco et al. 2006, 2007a). Current anatomical research is oriented towards studies of: • the superficial fascia, for its influence on lymphatic and venous return mechanisms • the internal fasciae, for its influence on visceral dysfunctions (Stecco in press). Treatment modalities specifically addressing these fascial layers have been developed. The Fascial Manipulation© method for musculoskeletal dysfunctions is characterized by an analytical procedure that results in personalized treatment for each subject. A combination of codified movement and palpatory tests permits therapists to determine which fascial points1 are involved in any given dysfunction. Each of these fascial points has a precise anatomical location within the fascial system, based on a functional interpretation of movement, as provided by the biomechanical model. A fundamental aspect of this method lies in differentiating between the area where the patient actually perceives pain, and the fascial points that require treatment. • the force-exerting element – the unidirectional muscle fibers • the coordinating element – the fascia • the perceptive element – the nerve structures, the joint capsule and ligaments. A significant characteristic of each MFU is the presence of both monoarticular and biarticular muscular fibers. The monoarticular fibers in each MFU are generally deeper fibers, specialized in moving a joint on one plane, and these fibers could be involved in the interplay between agonists and antagonists. In almost every MFU, a number of monoarticular fibers insert onto the intermuscular septum that separates two antagonist MFUs on the same plane. Whenever the agonist MFU is activated, traction exerted on the intermuscular septum could cause tension in the antagonist MFU, contributing to simultaneous adaptation, according to the inclination of the fibers and the segment involved. Recent studies of agonist and antagonist interaction by Huijing (2009) support this hypothesis. Different studies evidence the role of monoarticular and biarticular muscle fibers in multiple joint movements (Savelberg & Meijer 2003; Kurtzer et al. 2006). Within each MFU, some muscle fibers also insert directly onto the overlying fascia. These insertions could contribute to the maintenance of a basal tension of the fascia, and guarantee that fascia is stretched in a specific direction each time these muscle fibers contract (Stecco et al. 2008a, 2009b). Within each MFU, two specific points can be identified (Fig. 7.7.1): • A center of perception (CP): a precise area of the joint where traction exerted by the MFU on the joint capsule, tendons and ligaments is thought to converge. In a dysfunctional MFU this traction is not aligned along the correct physiological axis, causing joint movement to be incongruent or out of alignment. Over time, this could determine joint conflict, with friction and subsequent inflammation of periarticular soft tissues resulting in sensations of pain or joint instability. • A center of coordination (CC): a small area on the deep muscular fascia where force exerted by the muscular fibers of a MFU converges (the ‘point,’ referred to earlier). The resultant myofascial forces could be transmitted to the surface of the deep fascia via its continuity with the endomysium, perimysium, and epimysium. The CC within each MFU is thought to have the role of coordinating the motor units that are comprised within that MFU. Evidence exists regarding reduced coordination of motor units in the presence of joint pain (Mellor & Hodges 2005), although the mechanism is unknown. The Fascial Manipulation model suggests a new neurophysiological basis for the coordinating role of the CC. During any movement, motor units are activated, causing muscle fibers to contract according to the degree and direction of required joint movement. Muscle spindle capsules, embedded between muscle fibers, are continuous with surrounding endomysium; therefore, when gamma fiber stimulation causes intrafusal spindle fibers to contract, a minimal stretch is propagated throughout the entire fascial continuum, including the fascia at the CC. If the fascia at the CC is elastic, then it will adapt to this stretch, permitting muscle spindles to contract normally, correct activation of alpha motor fibers, and subsequent muscular contraction to proceed smoothly. If fascia at the CC is not elastic, the muscle spindle contraction could interfere with motor unit activation. Incongruent motor unit activation would then result in uncoordinated movement, perceived at the CP either as joint instability or as pain (Pedrelli et al. 2009a). Each MFU is located on one of the three spatial planes. The MFUs associated with the movement of antemotion2 (AN) are located in the anterior region of the limbs and trunk while the MFUs associated with retromotion3 (RE) are located in the posterior region. The MFUs associated with lateromotion (LA), movement away from the midline, are all located in the lateral region of the limbs and trunk, and those MFUs associated with mediomotion (ME), movement towards the midline, are located in the medial region. The MFUs associated with extrarotation (ER) are located in the retrolateral region of the limbs and trunk, and those associated with intrarotation (IR) in the anterolateral region (Fig. 7.7.2). Each MFU is named according to the segment it moves and the direction in which it moves that segment. There are 14 body segments and 6 directions, making a total of 84 CC and 84 CP (Fig. 7.7.3).
Introduction
The biomechanical model
The myofascial unit
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Fascial manipulation