Problematic Hand Fractures
CASE PRESENTATION
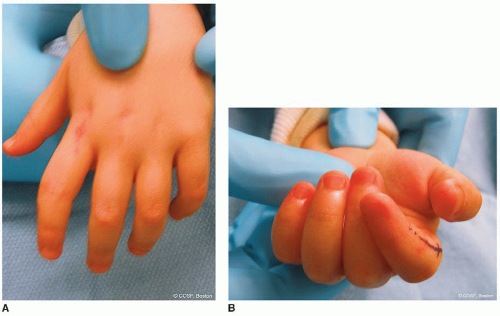
A 6-year-old male presents for evaluation of a “stiff and crooked” index finger. The patient reports that 4 weeks prior to presentation, the finger was “jammed” while catching a football. There were no wounds or lacerations, and no obvious dislocation was present. The injury was attributed to a “sprain,” and no medical evaluation was sought or treatment provided. Given persistent swelling, stiffness, and deformity, the patient presents for hand and upper extremity consultation. Radiographs are shown in Figure 35-1.
CLINICAL QUESTIONS
How common are pediatric hand fractures?
What are the most commonly injured bones? In which digits?
What are the problematic hand fractures that require surgical care?
What are the surgical principles and specific techniques used to treat problematic hand fractures?
What are the anticipated results?
What are the indications for corrective osteotomies of hand fracture malunions?
What are the common complications of hand fractures following nonoperative and surgical treatment?
THE FUNDAMENTALS
To climb steep hills requires slow pace at first.
—William Shakespeare
Hand fractures are fundamental problems cared for by every pediatric hand and upper extremity surgeon. Although many guiding principles and surgical techniques are universally applicable, children are not small adults, and a number of distinctions exist. Indeed, the pediatric hand surgeon must have a firm grasp of characteristic injury patterns, issues of skeletal growth and remodeling, more precise physical examination and surgical fixation techniques, and a rationale approach to postoperative immobilization and stiffness.
Etiology and Epidemiology
Hand injuries are common in the pediatric patient population.1, 2 and 3 Prior studies regarding the epidemiology of hand fractures in the United States, Canada, and England have demonstrated that the incidence of hand fractures is 2 to 9:1,000 children and adolescents per year. There is a bimodal distribution of injuries; toddlers between 0 and 4 years of age typically sustain distal phalangeal fractures and fingertip injuries as they use their hands to explore the world around them, while adolescents between 10 and 14 years of age (a time of rapid skeletal growth) more commonly have phalangeal and metacarpal fractures sustained from sports activities.2, 3 and 4 Overall, the proximal phalanx of the border digits (particularly the small finger) is most commonly fractured.5 Metacarpal fractures are usually diaphyseal, whereas phalangeal fractures typically involve the proximal metaphysis or physis. Indeed, physeal fractures represent 20% to 30% of all hand fractures in children; Salter-Harris type II patterns predominate.5, 6 and 7 Despite the frequency of growth plate involvement, however, post-traumatic growth disturbance rarely occurs in closed fractures.
Clinical Evaluation
Clinical evaluation begins with a careful history, with particular attention to the chronicity of the fracture, mechanism of injury, and presence of any associated wounds or lacerations. Careful history taking is particularly important in the young child, where cooperation with the physical examination and radiographic evaluation may be limited.
Physical examination of the injured hand can be challenging, particularly in the anxious, noncompliant, or nonverbal child. Careful observation, utilization of anatomic principles, such as the tenodesis effect, and gentle maneuvers are mandatory to obtain the information needed for accurate and timely diagnosis. The presence of swelling, ecchymosis, guarded active motion, or soft tissue injury will guide the examiner to the region of pathology. Tenodesis
effect (passive wrist extension produces passive digital flexion and passive wrist flexion results in digital extension) or gentle pressure applied to the more proximal muscle bellies of the forearm (away from the site of injury) will aid in the assessment of both tendon integrity and angular or rotational deformity (Figure 35-2). Assessment of rotational deformity is critical, as rotational malalignment exhibits little remodeling and may result in compromised hand function due to digital overlap or underlap. Malrotation may also be assessed by careful examination of the nail beds of adjacent digits in extension; rotation of >10 degrees out of the plane of adjacent nail plates should alert the examiner to rotational malalignment, though these differences are often subtle and difficult to quantify. In addition, people are usually symmetric and so always compare the rotational alignment of the injured to the uninjured hand. Additional assessment of rotational deformity can be made by evaluation of digital alignment with attempted finger flexion if the child is cooperative. In general, the index through small fingers point to the scaphoid tubercle in flexion, roughly in symmetric alignment to the opposite hand; often patients normally exhibit some degree of digital underlap, small beneath ring fingers. In young anxious or nonverbal patients unable to actively flex their digits during physical examination, the tenodesis effect may be used; gentle passive extension of the wrist should also allow for obligate digital flexion to assess for rotational alignment. Only after all information is derived from observation and indirect examination techniques should direct palpation and/or stress testing be performed.
effect (passive wrist extension produces passive digital flexion and passive wrist flexion results in digital extension) or gentle pressure applied to the more proximal muscle bellies of the forearm (away from the site of injury) will aid in the assessment of both tendon integrity and angular or rotational deformity (Figure 35-2). Assessment of rotational deformity is critical, as rotational malalignment exhibits little remodeling and may result in compromised hand function due to digital overlap or underlap. Malrotation may also be assessed by careful examination of the nail beds of adjacent digits in extension; rotation of >10 degrees out of the plane of adjacent nail plates should alert the examiner to rotational malalignment, though these differences are often subtle and difficult to quantify. In addition, people are usually symmetric and so always compare the rotational alignment of the injured to the uninjured hand. Additional assessment of rotational deformity can be made by evaluation of digital alignment with attempted finger flexion if the child is cooperative. In general, the index through small fingers point to the scaphoid tubercle in flexion, roughly in symmetric alignment to the opposite hand; often patients normally exhibit some degree of digital underlap, small beneath ring fingers. In young anxious or nonverbal patients unable to actively flex their digits during physical examination, the tenodesis effect may be used; gentle passive extension of the wrist should also allow for obligate digital flexion to assess for rotational alignment. Only after all information is derived from observation and indirect examination techniques should direct palpation and/or stress testing be performed.
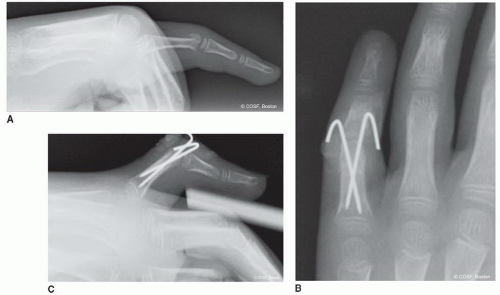
 FIGURE 35-1 Lateral radiograph depicting a displaced phalangeal neck fracture. Note is made of early callus formation, consistent with an incipient malunion. |
Appropriate radiographic imaging is imperative in the evaluation of the child’s injured hand. In general, dedicated anteroposterior (AP), lateral, and oblique radiographs of the injured digit are preferred over hand radiographs, in which overlying structures, projectional
artifact, and lack of bony magnification or detail may lead to errors in diagnosis. In situations in which expedited or very comprehensive radiographic assessment is needed, the use of fluoroscopy and/or a mini-image intensifier may assist in obtaining appropriate views of the injured digit, comparison views of the contralateral hand, or dynamic assessment of bony and articular stability.
artifact, and lack of bony magnification or detail may lead to errors in diagnosis. In situations in which expedited or very comprehensive radiographic assessment is needed, the use of fluoroscopy and/or a mini-image intensifier may assist in obtaining appropriate views of the injured digit, comparison views of the contralateral hand, or dynamic assessment of bony and articular stability.
Be aware of the normal sequence of skeletal ossification as well as common radiographic normal variants, which may be mistaken for traumatic injuries.8,9 The physes of the phalanges are proximal and distal in the metacarpals except the thumb. In general, the proximal phalangeal epiphyses become visible radiographically between 10 and 24 months of age and in females prior to males. The epiphyses of the middle and distal phalanges ossify approximately 6 to 8 months later. Physeal closure proceeds in a distal to proximal direction, typically between the ages of 14 and 16 years. The index through small metacarpal epiphyses ossify at 12 to 27 months of age and fuse between 14 and 16 years of age. The thumb metacarpal epiphysis, however, does not typically ossify until 24 to 36 months of age.
Common radiographic normal variants include the appearance of a pseudoepiphysis of the distal thumb metacarpal and the proximal index metacarpal.10 The pseudoepiphyses become radiographically apparent at an early age, do not contribute to the longitudinal growth of the metacarpal, and typically fuse to the metacarpal diaphysis by the seventh year of life. Other anatomic variants include the double epiphysis, most commonly appearing in the index and thumb metacarpals. These physeal variants can be misinterpreted as a fracture.
Classification of skeletal injuries remains anatomic and descriptive, with injuries described according to location, displacement, and angulation. In the subset of physeal fractures, the Salter and Harris system continues to be used, owing to its simplicity and its ability to guide fracture management and prognosticate outcomes.
Surgical Indications
While the vast majority of pediatric hand fractures may be successfully treated with nonoperative care, there are several characteristic injuries that require surgical care.6,11 Indeed, these problematic hand fractures account for the small percentage of hand fractures that are responsible for a large percentage of complications.
In the now classic series published by Hastings and Simmons,6 354 pediatric hand fractures were retrospectively analyzed with a minimum 2-year follow-up. In that series, several “high-risk” fractures were identified, including displaced articular fractures, Seymour fractures, phalangeal neck fractures, and open fractures. Risk factors associated with malunion and ultimately poor clinical results included failure to assess clinical deformity, failure to obtain proper AP and true lateral radiographs of the affected digit, failure to obtain adequate postreduction radiographs, and false assumptions regarding skeletal remodeling potential. Rather than provide a comprehensive survey of all pediatric hand injuries, it is these problematic hand fractures that will be the focus of this chapter.
SURGICAL PROCEDURES
Many strokes overthrow the tallest oaks.
—John Lyly
A few overarching principles apply to the surgical care of pediatric hand fractures. First, due to the small size of the skeletal structures and relative abundance of surrounding subcutaneous fat and soft tissue, closed or open surgical fixation requires the use of smaller implants placed with greater precision. Second, given the desire to avoid iatrogenic injury to the adjacent or affected growth plate, “physeal-friendly” fixation is preferred, typically utilizing smaller caliber smooth wires avoiding passage across the physis whenever possible. In addition, while it diminishes the risk of delayed union or nonunion—particularly in closed injuries—the robust biological healing potential in children narrows the window of opportunity to effectuate fracture reduction using closed techniques. Furthermore, as children and adolescents will exhibit varying degrees of compliance with postinjury or postoperative care, more restrictive immobilization is required to maximize maintenance of reduction and long-term outcomes. Fortunately, the use of more restrictive immobilization is not associated with as much long-term stiffness in children as opposed to adults. Finally, as with all hand fractures, every effort should be made to utilize the simplest, least invasive technique possible to achieve the desired result. Never open or plate a pediatric finger fracture unless you have to.
• Closed Reduction Percutaneous Pinning of Phalangeal Neck Fractures
Phalangeal neck fractures are characteristic pediatric injuries. Classically due to “door jamb” injuries in which a digit is caught in a closing door and forcefully withdrawn, phalangeal neck fractures are now occurring with greater frequency from sports-related mechanisms. Regardless of the cause, the injury mechanism imparts both extension and rotational forces on the affected digit. Border digits are most commonly affected, and the middle phalanx is injured more frequently than the proximal phalanx. The fracture occurs at the level of the phalangeal neck, and the distal articular segment typically displaces into extension with varying degrees of rotation. Patients will present with swelling, tenderness, ecchymosis, and limited interphalangeal (IP) joint motion, though the latter is often difficult to appreciate in the acutely injured child.
Given that the deformity occurs in the sagittal plane, standard AP views of the affected digit or hand may appear benign.6 A true lateral radiograph of the injured digit is necessary, and a high index of suspicion for rotational deformity must be maintained. In very young patients in whom the
phalangeal head is predominantly cartilaginous, subtle or seemingly innocuous “bony flecks” should raise suspicion for a displaced “cartilaginous cap” or osteochondral fracture. Displaced phalangeal neck fractures result in both abnormal sagittal plane alignment as well as obliteration of the concave subcondylar fossa; this causes a block to IP joint flexion, as the more distal phalangeal base abuts the bony prominence at the distal end of the proximal fracture fragment.
phalangeal head is predominantly cartilaginous, subtle or seemingly innocuous “bony flecks” should raise suspicion for a displaced “cartilaginous cap” or osteochondral fracture. Displaced phalangeal neck fractures result in both abnormal sagittal plane alignment as well as obliteration of the concave subcondylar fossa; this causes a block to IP joint flexion, as the more distal phalangeal base abuts the bony prominence at the distal end of the proximal fracture fragment.
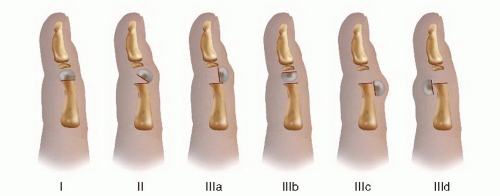 FIGURE 35-3 Schematic diagram of the classification of phalangeal neck fractures.12 |
Al-Qattan classification of extra-articular phalangeal neck fractures is clinically useful, as it portends prognosis and guides treatment12 (Figure 35-3). Type I fractures are nondisplaced. Type II fractures are partially displaced with some bony/cortical contact. Type III fractures are completely displaced without bony apposition. Cast immobilization is sufficient in cases of nondisplaced injuries, though serial radiographic evaluations should be performed to monitor maintenance of reduction.
As the phalangeal physis is proximal, and phalangeal neck fractures occur distally, remodeling potential is limited. Indeed, while there have been a handful of case reports documenting remodeling of displaced phalangeal neck fractures, it is apparent that skeletal remodeling: (1) is more likely in very young patients, (2) occurs over many years, during which persistent IP joint flexion is limited, (3) may be incomplete, and (4) will not spontaneously correct rotational malalignment.13, 14, 15 and 16 Based on this,
observation of displaced phalangeal neck fractures should only be considered if there is no rotational or radioulnar deformity, congruent reduction of the adjacent IP joint, considerable remaining skeletal growth, tolerable loss of IP joint flexion, and willingness on the part of the patient and family to wait months to years for remodeling to occur.13
observation of displaced phalangeal neck fractures should only be considered if there is no rotational or radioulnar deformity, congruent reduction of the adjacent IP joint, considerable remaining skeletal growth, tolerable loss of IP joint flexion, and willingness on the part of the patient and family to wait months to years for remodeling to occur.13
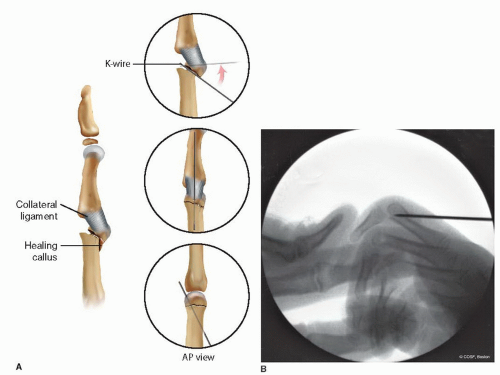
Closed reduction and splinting/cast immobilization alone are insufficient in the treatment of type II and III fractures; therefore, closed reduction and percutaneous pin fixation are recommended for displaced injuries12 (Figure 35-4). Under general anesthesia and with fluoroscopy available, the angular and rotational alignment of the affected digit is assessed. The normal digital cascade of the contralateral hand should be assessed preoperatively to identify what is normal for each individual patient. Closed reduction is then performed with longitudinal traction, followed by correction of the angular and rotational deformity, and subsequent IP joint flexion. Retrograde crossed percutaneous pins (most commonly 0.035″ in size) are then placed, beginning in the collateral recess and engaging the far cortex of the proximal fragment, with care taken to avoid crossing the pins at the fracture site. The starting point is more distal than is usually suspected, and inexperienced surgeons often entirely miss the distal fragment with initial pin placement. Intraoperative imaging will confirm appropriate bony alignment and implant placement. The pins are bent and cut outside the skin in the usual fashion, followed by application of a sterile petroleum gauze (Xeroform, Covidien, Mansfield, MA) and a hand-based short-arm cast.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree