I. Fracture Description
A. Soft Tissues
1. Closed fractures—The fracture is not exposed to the external environment. The soft-tissue injury ranges from minor to massive (e.g., crush injury). Closed soft-tissue injuries are commonly graded by the method of Tscherne.
• Grade 0 injuries have negligible soft-tissue injury.
• Grade 1 injuries have superficial abrasions or contusions of the soft tissues overlying the fracture.
• Grade 2 injuries have significant contusion to the muscle, contaminated skin abrasions, or both types of injury. The bony injury is usually severe in these injuries.
• Grade 3 injuries have a severe injury to the soft tissues, with significant degloving, crushing, compartment syndrome, or vascular injury.
2. Open fractures—The fracture is exposed to the external environment. The amount of soft-tissue destruction is related to the level of energy imparted to the limb during the traumatic episode.
• Classification—Open fractures are commonly described using the Gustilo grading system.
(a) Type I open fractures have small (<1 cm), clean wounds; minimal injury to the musculature; and no significant stripping of periosteum from bone.
(b) Type II open fractures have larger (>1 cm) wounds, but do not have significant soft-tissue damage, flaps, or avulsions.
(c) Type III open fractures have larger wounds and are associated with extensive injury to the integument, muscle, periosteum, and bone. Gunshot injuries and open fractures caused by a farm injury are special categories of Type III open fractures.
(d) Type IIIa injuries have extensive contamination and/or injury to the underlying soft tissues, but adequate viable soft tissue is present to cover the bone and neurovascular structures without a muscle transfer.
(e) Type IIIb injuries have such an extensive injury to the soft tissues that a rotational or free muscle transfer is necessary to achieve coverage of the bone and neurovascular structures. These injuries usually have massive contamination.
(f) Type IIIc injuries are any open fractures with an associated vascular injury that requires an arterial repair.
Often, what appears to be a Type I or II open fracture on initial examination in the emergency room is noted to have significant periosteal stripping and muscle injury at the time of operative debridement, and may require muscle transfer for coverage after serial debridements. Thus, there is a tendency for the Gustilo classification type to increase with time.
• Antibiotic prophylaxis for open fractures—Prophylactic antibiotics following an open fracture are given for 48 to 72 hours (as compared with only 24 hours in clean surgical cases). In patients returning to the operating room for serial debridement, most orthopedic surgeons continue the antibiotics for 48 hours following the final debridement. The regimen for prophylactic antibiotic coverage is dependent on the severity (Gustilo type) of the open fracture.
(a) Gustilo Type I—First or second generation cephalosporin (most commonly, Ancef)
(b) Gustilo Type II—First or second generation cephalosporin (most commonly, Ancef)
(c) Gustilo Type IIIa—First or second generation cephalosporin plus an Aminoglycoside
(d) Gustilo Type IIIb and IIIc—First- or second-generation cephalosporin plus an Aminoglycoside plus Penicillin (additional antibiotic coverage with a third-generation cephalosporin should be considered for patients with open marine [such as swamp] injuries).
• Tetanus prophylaxis—See Chapter 1, General Principles of Trauma.
• Traumatic amputation—The recommended sequence of structural repair during replantation is skeletal stabilization, arterial repair, venous repair, nerve repair, and muscle suture.
3. Soft-tissue injuries
• Overview—The requirements for wound healing are oxygenation, functioning cellular mechanisms, and a clean wound without contamination or necrotic tissue. There are four phases of wound healing:
(a) Coagulation phase (minutes)
(b) Inflammatory phase (hours)
(c) Granulation phase (days)
(d) Scar formation phase (weeks)
• Specific issues
(a) Skeletal muscle—Muscle injuries typically heal with dense scarring. Surgical repair of clean lacerations of skeletal muscle usually result in minimal regeneration of muscle fibers distally, scar formation at the laceration, and recovery of approximately 50% of muscle strength.
(b) Tendons—Tendons are composed of fibroblasts arranged in parallel rows in fascicles. Two types of tendons exist:
• Paratenon—Covered tendons (vascular tendons)—many vessels supply a rich capillary system.
• Sheathed tendons—A mesotenon (vincula) carries a vessel that supplies only one segment of the tendon; avascular areas receive nutrition via diffusion from vascularized segments. Because of these differences in vascular supply, paratenon-covered tendons heal better than sheathed tendons.
Tendinous healing in response to injury is initiated by fibroblasts that originate in the epitenon and macrophages that initiate healing and remodeling. Tendon repairs are weakest at 7 to 10 days; they regain most of their original strength at 21 to 28 days and achieve maximum strength at 6 months.
(c) Ligaments—The ultrastructure of ligament is similar to that of tendons, but the fibers are more variable and have a higher elastin content. Unlike tendons, ligaments have a “uniform microvascularity,” which receives its supply at the insertion site. Ligament healing benefits from normal stress and strain across the joint. Early ligament healing is with Type III collagen that is later converted to Type I collagen. Immobilization adversely affects the strength (elastic modulus decreases) of an intact ligament and of a ligament repair. The most common mechanism of ligament failure is rupture of sequential series of collagen fiber bundles distributed throughout the body of the ligament and not localized to one specific area. Ligaments do not plastically deform (“they break not bend”). Midsubstance ligament tears are common in adults; avulsion injuries are more common in children. Avulsion of ligaments typically occurs between the unmineralized and mineralized fibrocartilage layers.
• Management of soft-tissue injuries associated with fractures
(a) Overview—The care of patients with soft-tissue injuries proceeds in an orderly fashion through three phases. The acute phase includes wound irrigation, wound debridement, skeletal stabilization, reconstruction of the soft tissues, and resumption of joint range of motion. The reconstructive phase deals with sequelae of the traumatic injury (delayed unions, nonunions, deformities, infections). The rehabilitative phase addresses the patients’ psychological, social, and vocational recovery.
(b) General principles of the acute phase treatment
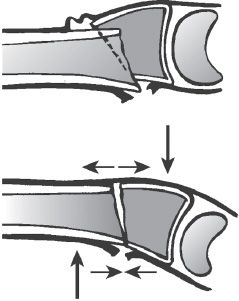
• Assess for the zone of soft-tissue injury—The soft-tissue zone of injury is generally much larger than the area of the fracture itself (Fig. 2-1).
• Assess for associated vascular injuries (limb viability).
• Assess for nerve injuries.
• Pulsating irrigation in the operating room should be performed with copious isotonic solution, removing necrotic and foreign material.
• Debridement (meticulous) of all foreign and necrotic material from the wound. This should be performed every 24 to 48 hours until the wound is felt to be ready for closure or coverage.

FIGURE 2-1 Diagrammatic representation of the zone of soft-tissue injury. Note that the area of soft-tissue injury is much greater than the area of the fracture site.
• Open wounds should be extended using a scalpel to allow access to underlining tissues for assessment and debridement.
• Free bony ends should be delivered into the open wound; small devitalized pieces of cortical bone are removed. The intramedullary cavity is examined and cleaned.
(c) Types of wound closure or coverage
• Primary closure
• Delayed primary closure
• Healing by secondary intention
• Split-thickness skin grafts
• Random flaps—Such as a cross finger flap
• Vascularized pedicle flaps—Such as gastrocnemius flap
• Free flaps (Fig. 2-2)—These may be fasciocutaneous flaps or myocutaneous flaps.
(d) Timing of wound closure or coverage—Early wound closure or coverage (3 to 5 days) is associated with improved outcomes.
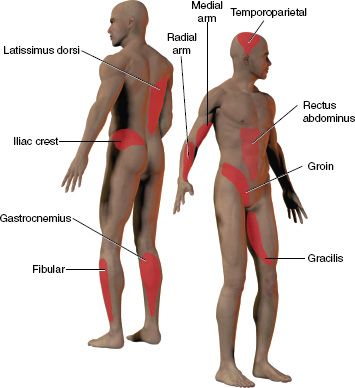
FIGURE 2-2 Topical atlas of the most commonly used donor sites for free tissue transfer.
1. Anatomic location—Name of bone(s) involved
2. Regional location
• Diaphysis
• Metaphysis
• Epiphysis
(a) Extra-articular
(b) Intra-articular
• Physis (in skeletally immature individuals)
3. Direction of fracture lines
• Transverse—The loading mode resulting in fracture is tension
• Oblique—The loading mode resulting in fracture is compression
• Spiral—The loading mode resulting in fracture is torsion
4. Condition of bone (Fig. 2-3)
• Comminution—A comminuted fracture is one with three or more bony fragments. Comminuted fractures generally result from high-energy injuries.
• Pathologic fracture—A fracture through an area of pre-existing disease with weakened bone (primary bone tumors, metastases to bone, bone infections, osteoporosis, metabolic bone disease, and others).
• Incomplete fracture—One in which the bone is not broken into separate fragments.
• Segmental fracture—One in which there is a middle fragment of bone surrounded by a proximal and a distal segment. The middle fragment usually has an impaired blood supply. These injuries are typically high-energy injuries with soft-tissue stripping (muscle and periosteum) from bone, and are therefore prone to poor healing (delayed union or nonunion).
• Fracture with bone loss—This may be caused by an open fracture where bone is left at the scene of the injury (a high-energy open injury) or is devitalized by the injury and requires debridement, or a closed fracture where a segment is comminuted so severely that from a practical standpoint there is a “missing” segment of bone.
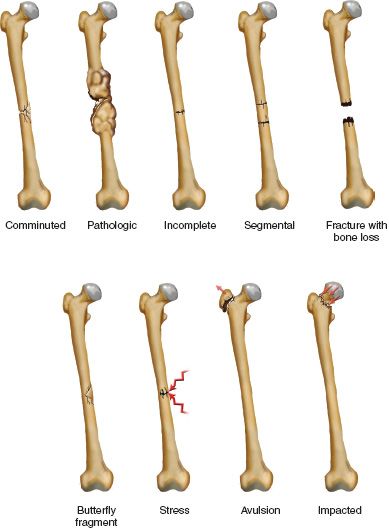
FIGURE 2-3 Condition of the bone in fractures.
• Fracture with a butterfly fragment—This is similar to a segmental fracture except that the butterfly segment does not span the entire cross-section of the bone. The loading mode resulting in fracture is bending.
• Stress fracture—A fracture caused by repeated loading such as in military recruits (who march all day) or ballet dancers. Amenorrheic female runners are also prone to stress fractures. Common sites of stress fractures include the metatarsals, calcaneus, and tibia (other sites are possible).
• Avulsion fracture—Caused by the pull of a tendon or ligament at its site of bony insertion. Acute avulsion fractures display irregular borders on radiography. These should not be confused with sesamoid bones (hands, foot, others) or an unfused center of ossification (bipartite patella, accessory navicular, os trigonum).
• Impacted fracture—The fracture fragments are compressed together (generally the result of an axial load).
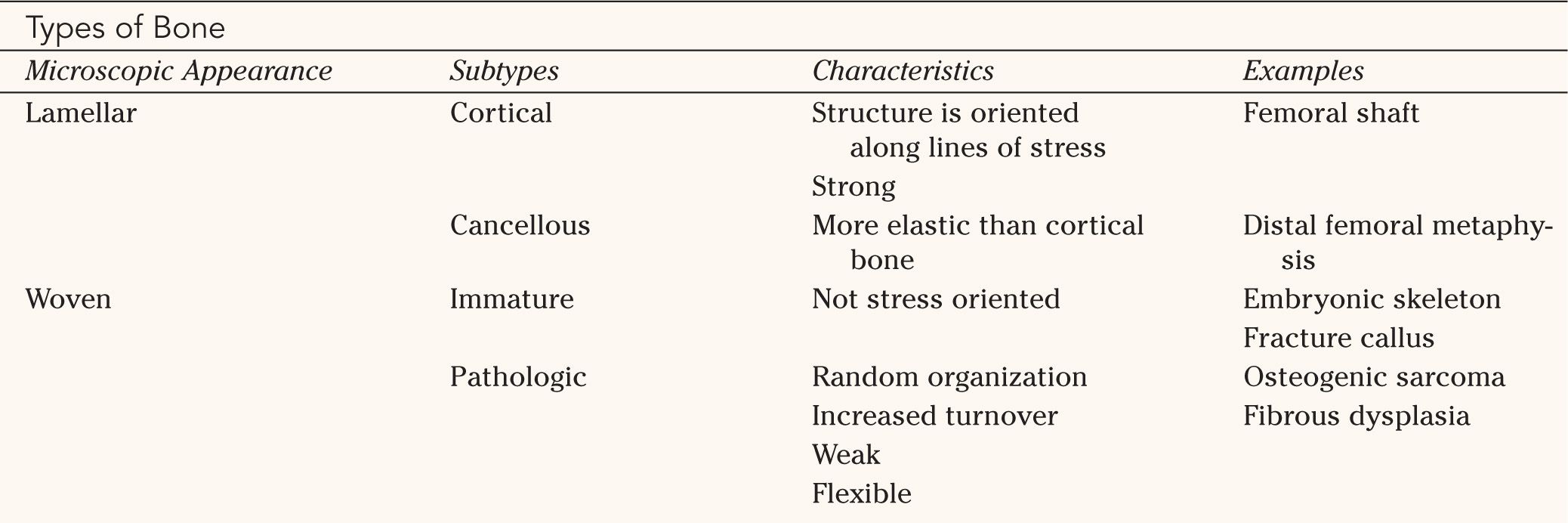
5. Type of bone involved (Table 2-1)
6. Deformities—See Chapter 3, Principles of Deformities
• Length—Describes shortening or overlengthening
• Angulation—Describes the direction (frontal, sagittal, oblique) in which the apex of the angulation points
• Rotation—Describes the turning of fracture fragments (or healed bony segments) along the long axis of a bone
• Translation—Describes anteroposterior and medial-lateral displacement of fracture fragments such that the fragments remain parallel to their initial position or each other
II. Fracture Management
A. Nonoperative Treatment—It is best used in patients with lower-energy injuries or with patients who are not candidates for operative treatment because of systemic or local factors.
1. Reduction via manipulation
• Three steps
(a) Longitudinal traction
(b) Disengagement of the fracture fragments (accentuating the deformity)
(c) Reapposition of the fracture ends
2. Casting techniques
• Three-point fixation (Fig. 2-4)
• Cylinder hydraulics
3. Traction techniques
• Skin traction
• Skeletal traction
B. Operative Treatment
1. External fixation—Indicated for open fractures, closed fractures with a severe soft-tissue injury, and fractures (or nonunions) associated with infection.


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






