Chapter 13 Principles and components of upper limb orthoses
Upper limb orthoses are distinct from other orthoses because of the complexity of the human hand. Many simultaneous joint motions must be considered for either mobilization or immobilization (e.g., nine interphalangeal [IP], five metacarpophalangeal [MCP], wrist, forearm, elbow, three shoulder), short digital levers (which translates to high forces, high pressures, and skin intolerance), and little soft tissue padding for bands and other components. Orthotic design for the upper limb must give equal focus to mechanical efficiency and precision of fit because comfort is critical for acceptance. Therefore, the small segments, limitations in soft tissue padding, and multiplicity of joint motion create high demands, which require a clinician with both a keen problem-solving sense and finely tuned fabrication skills.4 Frequently, and by design, the useful period is limited; when the treatment goals are met, the orthosis is discontinued. The orthosis can be discarded if the patient finds another, more acceptable means of function or if the benefit of the orthosis is outweighed by the patient’s lack of “gadget tolerance.”
Frequently, upper limb orthoses are applied to insensate limbs, and a well-defined skin inspection regimen must be followed to avoid excessive pressure. In common practice, the patient initially wears the orthosis for a relatively short period (5 to 30 minutes), then removes the orthosis and inspects the skin for persistent red marks. Red marks should disappear within 20 minutes. If they do not, the orthosis should be adjusted to alleviate the excessive pressure on the skin. If the red marks disappear within the 20-minute period, wearing time can be gradually increased (e.g., by 15 minutes) until the patient can tolerate wearing the device for several hours.
Static orthoses
Therapeutic
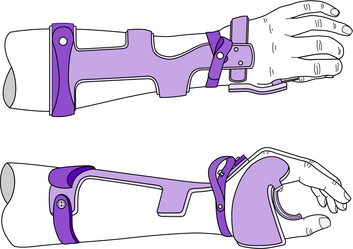
Static WHO
Clinical application: The static WHO (Fig. 13-1) supports the wrist joint, maintains the functional architecture of the hand, and prevents wrist–hand deformities. Occasionally the static WHO is used as a platform for other therapeutic attachments (e.g., MCP extension stop, IP extension assist, thumb extension assist). The static WHO illustrated in Fig. 13-1 is of the Rancho type. Several functionally equivalent metal and plastic designs are available, including those used at the Rehabilitation Institute in Chicago, The Institute for Rehabilitation and Research in Houston, and the Institute of Rehabilitation Medicine at New York University. The reader is referred to previous editions of this text for examples of alternative designs.
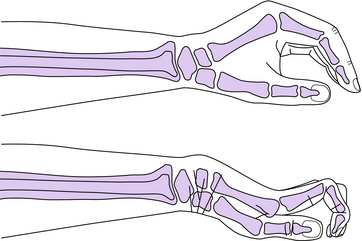
Patient population: Patients with severe weakness or paralysis of the wrist and hand musculature are appropriate candidates for the static WHO. Without support, these individuals are at risk for developing the “clawhand” deformity and/or overstretching weak muscles (Fig. 13-2). For example, quadriplegics usually exhibit the aforementioned weakness and can benefit from a static WHO to preserve the functional posture of the hand and wrist (Figs. 13-1 and 13-2). It is important to prevent encumbering contractures or deformities in patients because they may later become candidates for a functional WHO. The static WHO is often indicated as a positional orthosis for C1–5 quadriplegics with zero wrist extensors and an intrinsic minus hand.
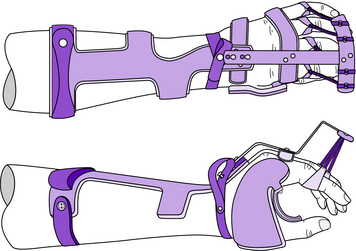
Attachments
Two of the most common attachments used with the static WHO are the MCP extension stop and the IP extension assist (Fig. 13-3). If there is loss of flexion range at the MCP joints and loss of extension range at the proximal IP joints, these two attachments can help prevent a clawhand deformity by preventing hyperextension of the MCP joints while encouraging extension of the IP joints of index through little fingers. Both of these attachments can be mounted on the same outrigger bar. This outrigger bar has two keyholes that facilitate installation and removal of the assembly.
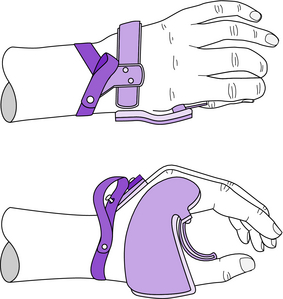
The thumb can be maintained in opposition while allowing a limited range of motion with the addition of a swivel thumb (Fig. 13-4). The swivel thumb acts as a carpometacarpal flexion assist for the thumb and consists of a custom-contoured metal band over the proximal phalanx of the thumb, which is secured to the radial extension of the palmar piece with a simple cantilevered wire spring (Fig. 13-4).
Static hand orthosis
Clinical application: The static HdO (Fig. 13-5) maintains the functional position of the hand and prevents development of deformities. Occasionally the static HdO is used as a platform for other therapeutic attachments. All the attachments described for the static WHO can also be used with the static HdO. Again, the Rancho design is depicted here, and the reader is referred to previous editions of this text for examples of other functionally equivalent upper limb orthoses designs.
Elbow orthosis
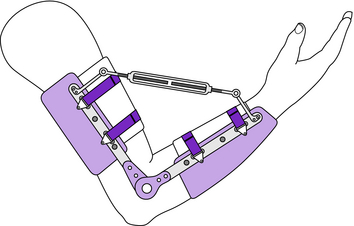
Clinical application: EOs designed for reducing soft tissue contractures must be custom designed and custom fabricated with structural plastic (polypropylene) bands and total-contact flexible plastic (polyethylene) cuffs and straps. They must incorporate at least one of a variety of mechanisms for increasing range of motion. Application of low-magnitude, long-duration forces is preferable when attempting to reduce an elbow flexion or extension contracture (Fig. 13-6). This is necessary to avoid the antagonist response, which accompanies quick, intense stretching. With quick and/or intense orthotic forces, the outcome may be tightening of the muscles in series and parallel with the tight collagen fibers. In addition, the skin is at greater risk for breakdown with higher forces. Particular attention must be given to mechanical/anatomical joint alignment, and the arm and forearm must be restricted to pure rotation with minimum translation to avoid joint subluxation or dislocation. The contracture reduction force must be gradually increased therapeutically (Fig. 13-6; slowly expand or contract the turnbuckle) so that the soft tissue collagen adhesions responsible for contracture can undergo microtears without causing trauma to the joint. The bands and cuffs should be placed near the elbow joint so that the levers of the three-point contracture reduction force system are maximized, correction forces are minimized, and skin pressure is tolerable. The edges of the bands and cuffs should be flared to avoid excessive edge pressure and shear. The therapeutic strategy should be to tease the tissues into lengthening without provoking an antagonistic response, causing permanent red marks on the skin, or creating internal bruising.
Patient population: EOs are used for reduction of soft tissue contractures of the elbow that result in functional limitations. The need to reduce elbow flexion or extension contractures can result from trauma or disease. The largest population affected consists of individuals with spinal cord injury who depend on full range of motion of the elbow for alleviating ischial sitting pressure, propelling a manual wheelchair, or bringing the hand to the face. Another common cause of restricted elbow motion is immobilization after trauma or surgery.
Shoulder–elbow orthosis
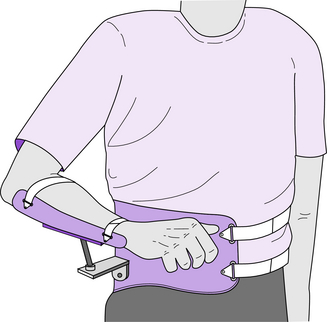
Clinical application: Support of a painful shoulder or traumatized brachial plexus–injured limb with an orthosis may be necessary. In many cases, a conventional arm sling suffices, provided there is no excessive force on the base of the neck and the use is short term. For long-term use, however, a sling offers very little function. The abduction orthosis, properly anchored on the hip, can be a successful alternative. Rancho Los Amigos Medical Center has developed a dynamic arm and shoulder support called the gunslinger (Fig. 13-7). The client’s arm is strapped to a forearm trough, which is mechanically coupled to a plastic hemigirdle anchored on the patient’s pelvis (iliac crest). The coupling between the forearm trough and iliac cap can be customized to permit a variety of motions, including glenohumeral joint internal/external rotation, flexion extension, and horizontal flexion/extension as well as flexion/extension of the elbow joint. The arm and hand are held in a cosmetically pleasing pose, and the hand is available for use, enabling early functional recovery. The gunslinger SEO is easy to put on and take off, and full deweighting of the arm is feasible.
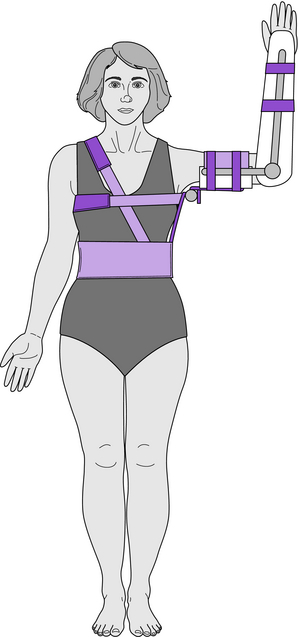
Shoulder–elbow–wrist orthosis
The SEWO depicted in Fig. 13-8 transmits the weight of the upper limb to the ipsilateral pelvis, and the system is stabilized with trunk straps. When this type of SEWO is used by clients with an axillary burn, the objective is to provide as much contact as possible while keeping the glenohumeral joint in maximum abduction. The anatomical elbow joint may be immobilized or free motion allowed. Generally the wrist is supported in extension to protect the associated soft tissues against the forces of gravity.
The orthosis shown in Fig. 13-8 is also known as the airplane orthosis because of the obvious resemblance when the device is used bilaterally. An alternate name for this orthosis is the shoulder stabilizer. By externally rotating the glenohumeral joint with the SEWO (Fig. 13-8), the internal rotators are stretched, and the tension on the deltoid and rotator cuff is relieved, which often are desirable after shoulder surgery.
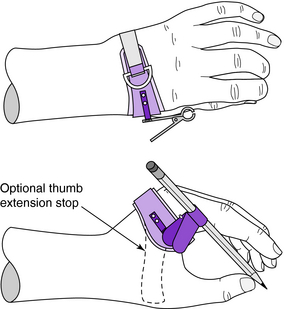
Functional
Clinical application: The static WHO and HdO can be modified to provide functional activities by attaching clips and pockets that hold utensils, writing devices, page turners, and so forth. The static HdO shown in Fig. 13-9 has a butterfly-type clamp attached to the radial extension that clasps the shaft of a writing device. An alternative to the clamp is the truss stud configuration on the palmar extension of the palmar side (Fig. 13-10). Utensils and other attachments are adapted with a slotted plate that engages the truss studs on the palmar side to secure the attachments. A simple HdO can be modified with an aluminum rod to create an ulnar page turner (Fig. 13-11). The rubber end of an eyedropper is used on the end of the aluminum rod for friction to facilitate page turning. Numerous devices can be attached to an HdO or WHO, including toothbrushes, razors, combs, brushes, hygiene aids, eating utensils, arts and crafts implements, and devices unique to the injured individual’s work environment.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree