Plane of motion
Motion
Sagittal (X-axis)
Dorsiflexion/plantar flexion
Frontal (coronal) (Z-axis)
Inversion/eversion
Transverse (Y-axis)
Forefoot/midfoot: adduction/abduction
Ankle/hindfoot: internal rotation/external rotation
Tri-planar motion
Supination: adduction, inversion, plantar flexion
Pronation: abduction, eversion, dorsiflexion
Gait Cycle
One gait cycle, or “stride,” is measured from heel strike to heel strike.
Ground reaction forces are approximately 1.5 times body weight during walking and 3–4 times body weight during running.
Stance phase: 62 % of gait cycle. Heel strike to toe-off
Heel strike:
Hindfoot valgus, forefoot abduction, dorsiflexion of ankle.
Anterior tibialis contracts eccentrically to control rate at which foot strikes the ground.
Quadriceps contract to stabilize knee.
Hindfoot unlocked/everted for energy absorption.
Foot flat: Single-limb support
Gastrocnemius-soleus complex contracts eccentrically.
Knee extends, hip extensors under concentric contraction.
Hindfoot unlocked/everted for ground accommodation.
Swing phase: 38 % of gait cycle. Toe-off to heel strike
Toe-off:
Hindfoot varus, forefoot adduction, plantarflexion of ankle.
Hip flexors contract. Gastrocnemius-soleus complex contracts concentrically.
Plantar fascia tightens, longitudinal arch is accentuated (windlass mechanism), and transverse tarsal joint locks → allows foot to convert from flexible shock absorber to rigid propellant.
Mid-swing: Foot clearance
Ankle dorsiflexors contract concentrically.
Loss of function results in steppage gait.
Terminal swing: Hamstring muscles decelerate forward motion of thigh.
Bibliography
1.
Chambers HG, Sutherland DH. A practical guide to gait analysis. J Am Acad Orthop Surg. 2002;10:222–31.
2.
Dicharry J. Kinematics and kinetics of gait: from lab to clinic. Clin Sports Med. 2010;29:347–64.
3.
Irwin TA, Kadakia AR. Miller review of orthopedics. 6th ed. Philadelphia: Elsevier Publications; 2012.
4.
Rodgers MM. Dynamic biomechanics of the normal foot and ankle during walking and running. Phys Ther. 1988;68:1822–30.
2 Ankle Arthroscopy
Take-Home Message
Indications for arthroscopy include treatment of OCLT, debridement of osteophytes and synovitis, removal of loose bodies, and cartilage debridement for ankle fusions.
Joint distraction, correct instrumentation, and systematic arthroscopic approach are vital to successful surgical procedure.
Arthroscopic portal options include anterolateral, anteromedial, posterolateral, and posteromedial and require a systematic approach for a thorough procedure.
Superficial peroneal nerve is most at risk from iatrogenic injury.
Relevant Anatomy
Tibiotalar joint: comprised of the ankle mortise superiorly and talar dome inferiorly (Fig. 1).
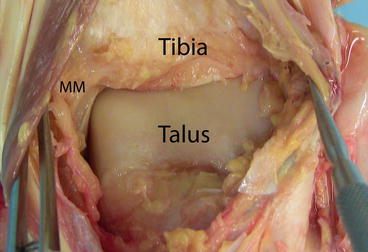
Fig. 1
Anatomic dissection of the anterior aspect of the ankle. The anterior aspect of the distal tibia, medial malleolus, and the talus are visualized
Distal tibiofibular joint: convex surface of medial fibular articulates with incisura fibularis. Syndesmotic ligaments include anterior inferior tibiofibular ligament, posterior inferior tibiofibular ligament, interosseous tibiofibular ligaments, and interosseous membrane.
Deltoid ligament complex: deep and superficial deltoid → to resist lateral talar translation and valgus.
Lateral ankle ligaments: anterior talofibular (ATFL), calcaneofibular (CFL), posterior talofibular (PTFL) → to resist varus forces.
Anterior neurovascular structures: superficial peroneal nerve (SPN), saphenous nerve, anterior tibial artery, vein, and deep peroneal nerve (DPN) (Fig. 2).
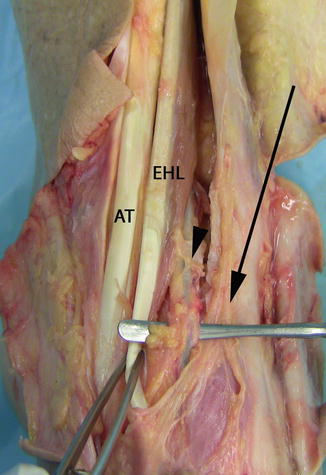
Fig. 2
Anterior tibial artery, vein, and deep peroneal nerve (arrowhead). The bundle lies deep the EHL at the level of the ankle and visualizing of the structures requires retraction of the tendon. The superficial peroneal nerve is also seen distally; it has been transected proximally (arrow)
Posterior neurovascular structures: sural nerve, tibial nerve, posterior tibial artery and vein.
Surgical Indications
Osteochondral lesions – chronic (debridement with microfracture) or acute (fixation of bony component)
Debridement of synovitis
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






