Fig. 1
AP and lateral view of a patient with hallux rigidus. Note the narrowing of the joint space on the AP with the common findings of a dorsal osteophyte on the metatarsal head with a loose body within the first MTP. Hallux rigidus is most easily identified on the lateral radiograph
MRI scan: look for osteochondral injury in the setting of normal X-rays.
Classification
Coughlin clinical-radiographic classification of hallux rigidus (Table 1)
Table 1
Coughlin clinical-radiographic classification of hallux rigidus
Grade | Dorsiflexion | Radiographic findings | Clinical findings |
|---|---|---|---|
0 | 40–60° and/or 10–20 % loss compared with normal side | Normal | No pain; stiffness, loss of motion |
1 | 30–40° and/or 20–50 % loss compared with normal side | Dorsal osteophytes; minimal joint-space narrowing, periarticular sclerosis, flattening of metatarsal head | Pain at extremes of dorsiflexion and/or plantar flexion |
2 | 10–30° and/or 50–75 % loss compared with normal side | Dorsal, lateral, and possibly medial osteophytes; flattened appearance to metatarsal head, ¼ or less of dorsal joint space involved on lateral radiograph, mild-to-moderate joint-space narrowing and sclerosis; sesamoids not usually involved | Moderate-to-severe pain and stiffness; pain occurs just before maximum dorsiflexion/plantar flexion on examination |
3 | =10° and/or 75–100 % loss compared with normal side. There is notable loss of metatarsophalangeal plantar flexion | Substantial joint space narrowing, periarticular cystic changes, more than 1/4 of dorsal joint space involved on lateral radiograph, sesamoids enlarged and/or cystic and/or irregular | Constant pain and stiffness at extremes of range of motion but not at mid-range |
4 | Same as in Grade 3 | Same as in Grade 3 | Definite pain at mid-range of passive motion |
Treatment Algorithm
Nonoperative: short period of rest followed by activity modifications, NSAIDS, intra-articular steroid injections, shoe modification (rigid sole). Orthotic = Morton’s extension carbon fiber plate
Operative (Table 2)
Table 2
Operative algorithm for hallux rigidus
Grade
Operative
0
Arthroscopic or open débridement, drilling, or grafting of metatarsal head OCD (if present)
1
Cheilectomy
2
Cheilectomy
3
Cheilectomy
4
MTP joint arthrodesis
Simplified
Cheilectomy: some preservation of joint space without pain in the central range of motion (Grades 1–3) (Fig. 2)
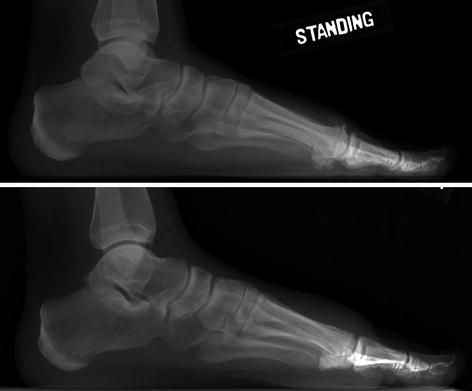
Fig. 2
Preoperative appearance of the dorsal osteophyte (top radiograph) and the postoperative appearance (bottom radiograph) following a cheilectomy. No more than 30 % of the metatarsal head should be resected to prevent iatrogenic instability
Fusion for deformity, pain with grind at central range of motion (grade 4), 100 % joint space loss, no motion (Figs. 3 and 4)

Fig. 3
Patient presented with hallux valgus and hallux rigidus (a). Correction of both deformities is best corrected with an arthrodesis (b) as an isolated cheilectomy or osteotomy to correct the hallux valgus will not be successful

Fig. 4
Patient with grade 4 hallux rigidus (a) (>50 % joint space loss with central grind). This is best treated with an arthrodesis (b)
Complications
Persistent pain
Recurrence of osteophyte formation
Progression of joint degeneration requiring additional surgery
Iatrogenic hallux valgus or varus deformity
Nonunion or malunion (ideal position – neutral rotation, slight hallux valgus, and dorsiflexion parallel to the floor. Best done with a flat plate intraoperatively to simulate the final clinical position. Superior to absolute values secondary to anatomic variability)
Bibliography
1.
Coughlin MJ, Shurnas PS. Hallux rigidus. Grading and long-term results of operative treatment. J Bone Joint Surg Am Vol. 2003;85-A:2072–88.
2.
Deland JT, Williams BR. Surgical management of hallux rigidus. J Am Acad Orthop Surg. 2012;20:347–58.
3.
Seibert NR, Kadakia AR. Surgical management of hallux rigidus: cheilectomy and osteotomy (phalanx and metatarsal). Foot Ankle Clin. 2009;14:9–22.
4.
Simpson GA, Hembree WC, Miller SD, Hyer CF, Berlet GC. Surgical strategies: hallux rigidus surgical techniques. Foot Ankle Int. 2011;32:1175–86.
2 Hallux Valgus
Take-Home Message
Hallux valgus is defined as a lateral deviation of the great toe with medial deviation of the first metatarsal.
DJD of the first MTP requires arthrodesis.
Hypermobility of first TMT requires Lapidus (first TMT arthrodesis).
Increased DMAA required redirectional osteotomy of distal metatarsal, in addition to other required osteotomies to correct the IMA.
Increased HVI requires an Akin osteotomy (medial closing wedge of phalanx).
Definition
Hallux valgus is defined as a lateral deviation of the great toe with medial deviation of the first metatarsal (Fig. 5).


Fig. 5
Two patients (a, b) with hallux valgus deformity. Note the increased medial deviation of the metatarsal head in the patient with a more severe deformity (b)
Etiology
Related to multiple factors and more common in females
Extrinsic Causes
Improper shoe wear (high-heeled shoes, pointed-toe shoes, and shoes with narrow toe boxes)
Intrinsic Causes
Genetic predisposition, ligamentous laxity, and predisposing anatomy (convex metatarsal head, pes planus) are contributory.
Inflammatory arthropathies (rheumatoid arthritis), metabolic bone disorders (gout), neuromuscular disorders (cerebral palsy, stroke)
Pathoanatomy
Medial capsular attenuation.
Proximal phalanx drifts laterally, leading to the following conditions:
Plantar-lateral migration of abductor hallucis; change in position causes the muscle to plantar flex and pronate the phalanx.
Stretching of the extensor hood of the extensor hallucis longus.
Lateral deviation of the extensor hallucis longus and flexor hallucis longus (FHL), causing a muscular imbalance and deforming force for valgus progression and pronation of the great toe.
The first metatarsal head moves medially off the sesamoids, increasing the intermetatarsal angle (IMA).
Secondary contracture of the lateral capsule, adductor hallucis, lateral metatarsal-sesamoid ligament, and intermetatarsal ligament.
Radiography
Multiple measurements can be obtained from standard radiographs that guide treatment options
Hallux valgus angle (HVA): angle formed by a line along the first metatarsal shaft and a line along the shaft of proximal phalanx (Fig. 6)

Fig. 6
AP radiograph denoting the hallux valgus angle. The acute angle (HV) formed by a line parallel to the first metatarsal shaft and a line parallel to the proximal phalangeal shaft is measured
Normal <15°
First to second intermetatarsal angle (IMA): angle formed by a line along the first metatarsal shaft and a line along the second metatarsal shaft (Fig. 7)
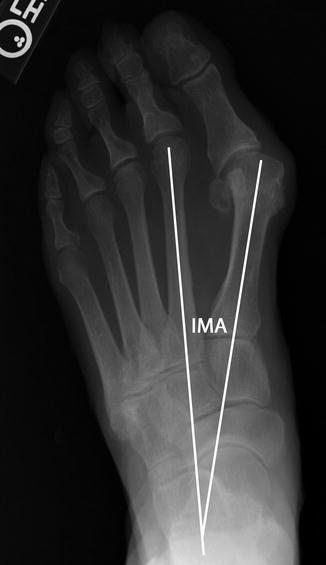
Fig. 7
AP radiograph denoting the intermetatarsal angle. The acute angle (IMA) formed by a line parallel to the first metatarsal shaft and the second metatarsal shaft is measured
Normal <9°
Hallux valgus interphalangeus (HVI) angle: angle formed by a line along the shaft of proximal phalanx and a line along the shaft of distal phalanx (Fig. 8)

Fig. 8
AP radiograph of the proximal phalanx denoting the hallux valgus interphalangeus angle. A line is drawn parallel to the proximal and distal articular surfaces. Perpendicular lines are drawn relative to these lines. The acute angle (HVI) formed by the perpendiculars is measured
Normal <10°
Associated with a congruent deformity
Distal metatarsal articular angle (DMAA): angle formed by a line along the articular surface of the first metatarsal and a line perpendicular to the axis of the first metatarsal
Normal <10°
Associated with a congruent deformity
Classification
There is no specific classification for hallux valgus that is routinely utilized. Specific recommendations are based upon the degree of deformity, which is discussed below.
The use of the term congruency has been utilized and is a source of confusion
Congruency is determined by comparing the line connecting the medial and lateral edge of the first metatarsal head articular surface with the similar line for the proximal phalanx, and when these lines are parallel, the joint is congruent; otherwise, it is incongruent (Fig. 9).

Fig. 9
This patient has an incongruent deformity noted by the lack of parallelism between the articular surface of the metatarsal and the proximal phalanx
The implication is that the patient has an intrinsic deformity of either an increased DMAA or HVI. These can be present with an incongruent deformity as well, and therefore each radiograph must be carefully reviewed.
Treatment
Nonoperative
NSAIDS for associated bursitis, shoe modifications (wide toe box, flat sole), orthotics (arch support in flat foot and metatarsal pad for second metatarsalgia), toe spacers if flexible deformity. These will not correct the deformity.
Operative

Algorithmic approach to identifying the appropriate surgical intervention. Rigid deformity, pain within the first MTP joint, inflammatory arthropathy, or radiographic evidence of arthritis requires the first MTP arthrodesis (Fig. 10).
All patients should undergo a soft tissue release with all associated osteotomies and the first TMT arthrodesis (Lapidus).

Fig. 10
This patient has a significant hallux valgus deformity with hallux rigidus and pain within the first MTP joint. (a) Correction of both the IMA and HVA is easily achieved with an arthrodesis without the need for additional metatarsal osteotomy (b)
IMA is ≤13° and HVA is ≤40°
Distal metatarsal osteotomy (chevron) (Fig. 11)

Fig. 11
In patients with a HVA ≤40 and an IMA ≤13 (a), a distal osteotomy with soft tissue correction is the most appropriate procedure (b)
Distal soft tissue release
Medial eminence resection and capsular repair
IMA is >13° or HVA is >40°
Proximal metatarsal osteotomy
Distal soft tissue release
Medial eminence resection and capsular repair
Instability of the First TMT/Joint Laxity
Lapidus (fusion of the first TMT joint) (Fig. 12)

Fig. 12
Regardless of preoperative deformity (a), in a patient with hypermobility, a Lapidus procedure is required (b)
Soft tissue release
Medial eminence resection and capsular repair
Increased DMAA (>10°)
Distal medial closed-wedge metatarsal osteotomy in addition to what is required based on the angular measurements.
IMA is ≤13°, and HVA is ≤40°
Distal biplanar closed-wedge metatarsal osteotomy.
Translate and redirect the metatarsal head simultaneously.
IMA is >13° HVA is >40°
Proximal metatarsal osteotomy and distal medial closed-wedge metatarsal osteotomy (Fig. 13)

Fig. 13
In this patient with an IMA >13 and an increased DMAA >10 (a), a double osteotomy is required (b). A proximal osteotomy in addition to a distal closing wedge osteotomy fully corrects the deformity
Instability of the first TMT/joint laxity
Lapidus and distal medial closed-wedge metatarsal osteotomy
Hallux valgus interphalangeus
Akin osteotomy can be done in isolation if no other deformity present.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






